Korean Circ J.
2012 Mar;42(3):197-200. 10.4070/kcj.2012.42.3.197.
Subarachnoid Hemorrhage Mimicking Leakage of Contrast Media After Coronary Angiography
- Affiliations
-
- 1Department of Cardiology, Heart Center, Chung-Ang University College of Medicine, Seoul, Korea. kdoc97@lycos.co.kr
- 2Department of Radiology, Chung-Ang University College of Medicine, Seoul, Korea.
- 3Department of Neurosurgery, Chung-Ang University College of Medicine, Seoul, Korea.
- KMID: 2225034
- DOI: http://doi.org/10.4070/kcj.2012.42.3.197
Abstract
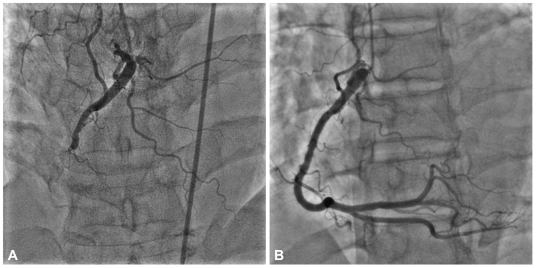
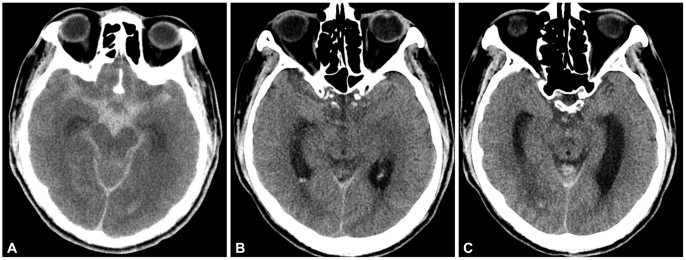
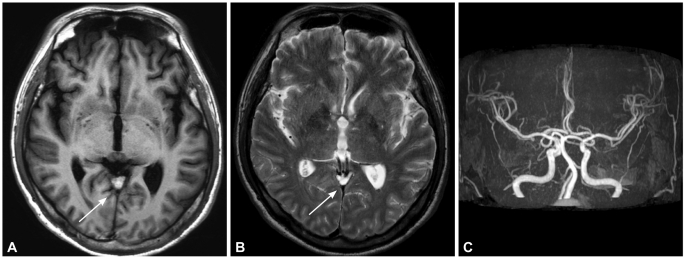
- We report a patient who developed subarachnoid hemorrhage (SAH) just after coronary angiography (CAG) with non-ionic contrast media (CM) and minimal dose of heparin. The 55-year-old man had a history of acute ST elevation myocardial infarction that had been treated with primary percutaneous coronary intervention and was admitted for a follow-up CAG. The CAG was performed by the transradial approach, using 1000 U of unfractionated heparin for the luminal coating and 70 mL of iodixanol. At the end of CAG, he complained of nausea and rapidly became stuporous. Brain CT showed a diffusely increased Hounsfield unit (HU) in the cisternal space, similar to leakage of CM. The maximal HU was 65 in the cisternal space. No vascular malformations were detected on cerebral angiography. The patient partially recovered his mental status and motor weakness after 2 days. Two weeks later, subacute SAH was evident on magnetic resonance imaging. The patient was discharged after 28 days.
MeSH Terms
-
Brain
Cerebral Angiography
Contrast Media
Coronary Angiography
Follow-Up Studies
Heparin
Humans
Magnetic Resonance Imaging
Middle Aged
Myocardial Infarction
Nausea
Percutaneous Coronary Intervention
Phenobarbital
Stupor
Subarachnoid Hemorrhage
Triiodobenzoic Acids
Vascular Malformations
Contrast Media
Heparin
Phenobarbital
Triiodobenzoic Acids
Figure
Reference
-
1. Sobieraj-Teague M, Gallus AS, Eikelboom JW. The risk of iatrogenic bleeding in acute coronary syndromes and long-term mortality. Curr Opin Cardiol. 2008; 23:327–334. PMID: 18520716.2. Kim DH, Lee SJ, Jeon U, et al. Spontaneous retroperitoneal hemorrhage and hemothorax after intravenous heparin treatment. Korean Circ J. 2009; 39:32–36.3. Melton LG, Muga KM, Gabriel DA. Effect of iodixanol on in vitro bleeding time. Acad Radiol. 1996; 3:407–411. PMID: 8796693.4. Sharp S, Stone J, Beach R. Contrast agent neurotoxicity presenting as subarachnoid hemorrhage. Neurology. 1999; 52:1503–1505. PMID: 10227646.5. Eikelboom JW, Mehta SR, Anand SS, Xie C, Fox KA, Yusuf S. Adverse impact of bleeding on prognosis in patients with acute coronary syndromes. Circulation. 2006; 114:774–782. PMID: 16908769.6. Velden J, Milz P, Winkler F, Seelos K, Hamann GF. Nonionic contrast neurotoxicity after coronary angiography mimicking subarachnoid hemorrhage. Eur Neurol. 2003; 49:249–251. PMID: 12736546.7. Weaver JP, Fisher M. Subarachnoid hemorrhage: an update of pathogenesis, diagnosis and management. J Neurol Sci. 1994; 125:119–131. PMID: 7807157.8. Chakeres DW, Bryan RN. Acute subarachnoid hemorrhage: in vitro comparison of magnetic resonance and computed tomography. AJNR Am J Neuroradiol. 1986; 7:223–228. PMID: 3082153.9. Hayman LA, Pagani JJ, Kirkpatrick JB, Hinck VC. Pathophysiology of acute intracerebral and subarachnoid hemorrhage: applications to MR imaging. AJR Am J Roentgenol. 1989; 153:135–139. PMID: 2660531.10. Yoon W, Seo JJ, Kim JK, Cho KH, Park JG, Kang HK. Contrast enhancement and contrast extravasation on computed tomography after intra-arterial thrombolysis in patients with acute ischemic stroke. Stroke. 2004; 35:876–881. PMID: 14988575.11. May EF, Ling GS, Geyer CA, Jabbari B. Contrast agent overdose causing brain retention of contrast, seizures and parkinsonism. Neurology. 1993; 43:836–838. PMID: 8469350.12. Torvik A, Walday P. Neurotoxicity of water-soluble contrast media. Acta Radiol Suppl. 1995; 399:221–229. PMID: 8610520.13. Eckel TS, Breiter SN, Monsein LH. Subarachnoid contrast enhancement after spinal angiography mimicking diffuse subarachnoid hemorrhage. AJR Am J Roentgenol. 1998; 170:503–505. PMID: 9456974.14. Sticherling C, Berkefeld J, Auch-Schwelk W, Lanfermann H. Transient bilateral cortical blindness after coronary angiography. Lancet. 1998; 351:570. PMID: 9492782.15. Culebras A, Kase CS, Masdeu JC, et al. Practice guidelines for the use of imaging in transient ischemic attacks and acute stroke: a report of the stroke council, American Heart Association. Stroke. 1997; 28:1480–1497. PMID: 9227705.16. Melton LG, Muga KM, Gabriel DA. Effect of contrast media on in vitro bleeding time: assessment by a hollow fiber instrument. Acad Radiol. 1995; 2:239–243. PMID: 9419555.17. Schwartz TH, Solomon RA. Perimesencephalic nonaneurysmal subarachnoid hemorrhage: review of the literature. Neurosurgery. 1996; 39:433–440. PMID: 8875472.18. Rinkel GJ, van Gijn J, Wijdicks EF. Subarachnoid hemorrhage without detectable aneurysm: a review of the causes. Stroke. 1993; 24:1403–1409. PMID: 8362440.19. De Wispelaere JF, Trigaux JP, Van Beers B, Gillard C. Cortical and CSF hyperdensity after iodinated contrast medium overdose: CT findings. J Comput Assist Tomogr. 1992; 16:998–999. PMID: 1430459.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Subarachnoid Hemorrhage Presenting with Seizure due to Cerebrospinal Fluid Leakage after Spinal Surgery
- The Effect of Non-Ionic Contrast Media on Q-T Interval and ST-T Wave of ECG during Coronary Angiography
- Salvage treatment with stenting and temporary balloon occlusion for subarachnoid hemorrhage after stent retrieval following acute proximal M3 occlusion treatment
- A Delayed, Unusual Non-Cardiogenic Pulmonary Edema after Intravascular Administration of Non-Ionic, Low Osmolar Radiocontrast Media for Coronary Angiography
- A Case of Severe Localized Reaction due to Extravasation of Contrast Media