Korean Circ J.
2012 Aug;42(8):538-542. 10.4070/kcj.2012.42.8.538.
Antithrombotic or Anti-Platelet Agents in Patients Undergoing Permanent Pacemaker Implantation
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, University of Ulsan College of Medicine, Gangneung Asan Hospital, Gangneung, Korea. jinkumc@gmail.com
- KMID: 2225003
- DOI: http://doi.org/10.4070/kcj.2012.42.8.538
Abstract
- BACKGROUND AND OBJECTIVES
The growing implantations of electrophysiological devices in the context of increasing rates of chronic antithrombotic therapy in cardiovascular disease patients underscore the importance of an effective periprocedural prophylactic strategy for prevention of bleeding complications. We assessed the risk of significant bleeding complications in patients receiving anti-platelet agents or anticoagulants at the time of permanent pacemaker (PPM) implantation.
SUBJECTS AND METHODS
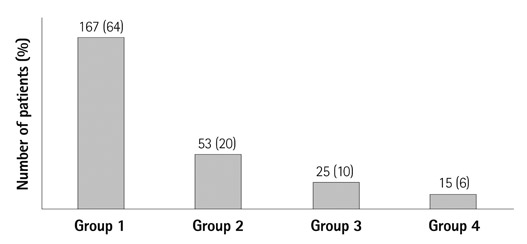
We reviewed bleeding complications in patients undergoing PPM implantation. The use of aspirin or clopidogrel was defined as having taking drugs within 5 days of the procedure and warfarin was changed to heparin before the procedure. A significant bleeding complication was defined as a bleeding incident requiring pocket exploration or blood transfusion.
RESULTS
Permanent pacemaker implantations were performed in 164 men and 96 women. The mean patient age was 73+/-11 years old. Among the 260 patients, 14 patients took warfarin (in all of them, warfarin was changed to heparin at least 3 days before procedure), 54 patients took aspirin, 4 patients took clopidogrel, and 25 patients took both. Significant bleeding complications occurred in 8 patients (3.1%), all of them were patients with heparin bridging (p<0.0001). Heparin bridging markedly increased the length of required hospital stay when compare with other groups and the 4 patients (1.5%) that underwent the pocket revision for treatment of hematoma.
CONCLUSION
This study suggests that hematoma formation after PPM implantation was rare, even among those who had taken the anti-platelet agents. The significant bleeding complications frequently occurred in patients with heparin bridging therapy. Therefore, heparin bridging therapy was deemed as high risk for significant bleeding complication in PPM implantation.
Keyword
MeSH Terms
Figure
Reference
-
1. Gupta A, Halleran SM, Krishnan K, Trohman RG. Rescue permanent iliac vein pacing after epicardial lead failure: an unusual reversal of pacing fortune. Europace. 2008. 10:1236–1238.2. Moss AJ, Zareba W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002. 346:877–883.3. Lee GY, Chang BS, Song JU, et al. Deglutition syncope associated with ventricular asystole in a patient with permanent atrial fibrillation. Korean Circ J. 2010. 40:99–101.4. Lee CK, Shin DH, Jang JK, et al. Progressive familial heart block type I in a Korean patient. Korean Circ J. 2011. 41:276–279.5. Maree AO, Fitzgerald DJ. Variable platelet response to aspirin and clopidogrel in atherothrombotic disease. Circulation. 2007. 115:2196–2207.6. Giudici MC, Paul DL, Bontu P, Barold SS. Pacemaker and implantable cardioverter defibrillator implantation without reversal of warfarin therapy. Pacing Clin Electrophysiol. 2004. 27:358–360.7. Hirsh J, Anand SS, Halperin JL, Fuster V. American Heart Association. Guide to anticoagulant therapy: Heparin: a statement for healthcare professionals from the American Heart Association. Circulation. 2001. 103:2994–3018.8. Möllmann H, Nef HM, Hamm CW, Elsässer A. How to manage patients with need for antiplatelet therapy in the setting of (un-)planned surgery. Clin Res Cardiol. 2009. 98:8–15.9. Llau JV, Lopez-Forte C, Sapena L, Ferrandis R. Perioperative management of antiplatelet agents in noncardiac surgery. Eur J Anaesthesiol. 2009. 26:181–187.10. Phan TG, Koh M, Wijdicks EF. Safety of discontinuation of anticoagulation in patients with intracranial hemorrhage at high thromboembolic risk. Arch Neurol. 2000. 57:1710–1713.11. Marquie C, De Geeter G, Klug D, et al. Post-operative use of heparin increases morbidity of pacemaker implantation. Europace. 2006. 8:283–287.12. Goldstein DJ, Losquadro W, Spotnitz HM. Outpatient pacemaker procedures in orally anticoagulated patients. Pacing Clin Electrophysiol. 1998. 21:1730–1734.13. Ahmed I, Gertner E, Nelson WB, et al. Continuing warfarin therapy is superior to interrupting warfarin with or without bridging anticoagulation therapy in patients undergoing pacemaker and defibrillator implantation. Heart Rhythm. 2010. 7:745–749.14. Cheng A, Nazarian S, Brinker JA, et al. Continuation of warfarin during pacemaker or implantable cardioverter-defibrillator implantation: a randomized clinical trial. Heart Rhythm. 2011. 8:536–540.15. Daubert JC, Mabo P. Continue or withhold oral anticoagulation in high-risk patients undergoing pacemaker or ICD implantation. Eur Heart J. 2009.16. Wiegand UK, LeJeune D, Boguschewski F, et al. Pocket hematoma after pacemaker or implantable cardioverter defibrillator surgery: influence of patient morbidity, operation strategy, and perioperative antiplatelet/anticoagulation therapy. Chest. 2004. 126:1177–1186.17. Dreger H, Grohmann A, Bondke H, Gast B, Baumann G, Melzer C. Is antiarrhythmia device implantation safe under dual antiplatelet therapy? Pacing Clin Electrophysiol. 2010. 33:394–399.18. Kutinsky IB, Jarandilla R, Jewett M, Haines DE. Risk of hematoma complications after device implant in the clopidogrel era. Circ Arrhythm Electrophysiol. 2010. 3:312–318.19. Tompkins C, Cheng A, Dalal D, et al. Dual antiplatelet therapy and heparin "bridging" significantly increase the risk of bleeding complications after pacemaker or implantable cardioverter-defibrillator device implantation. J Am Coll Cardiol. 2010. 55:2376–2382.20. Eisenberg MJ, Richard PR, Libersan D, Filion KB. Safety of short-term discontinuation of antiplatelet therapy in patients with drug-eluting stents. Circulation. 2009. 119:1634–1642.21. Furie B, Furie BC. Mechanisms of thrombus formation. N Engl J Med. 2008. 359:938–949.22. Vane JR, Botting RM. The mechanism of action of aspirin. Thromb Res. 2003. 110:255–258.23. Hirsh J, Dalen J, Anderson DR, et al. Oral anticoagulants: mechanism of action, clinical effectiveness, and optimal therapeutic range. Chest. 2001. 119:1 Suppl. 8S–21S.24. Grines CL, Bonow RO, Casey DE Jr, et al. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: a science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. J Am Coll Cardiol. 2007. 49:734–739.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of antithrombotic agents and current issues in patients undergoing endoscopic submucosal dissection
- Results of Permanent Cardiac Pacemaker Implantation in Ewha Womans University Mokdong Hospital
- Early Detection of Perforation of the Right Ventricle by a Permanent Pacemaker Lead
- A Case of Pacemaker Implantation after Balloon Venoplasty on Innominate Vein Stenosis
- A Case Report of Rare Complications after Epicardial Permanent Pacemaker Implantation in an Infant: Airway Compression, Skin Necrosis, and Bowel Perforation