Korean Circ J.
2013 Apr;43(4):265-268. 10.4070/kcj.2013.43.4.265.
Percutaneous Transluminal Angioplasty of Contralateral Iliac and Superficial Femoral Arteries via Graft Vessel in a Patient with FemoroFemoral Bypass Graft
- Affiliations
-
- 1Department of Cardiology, College of Medicine, Dongguk University, Gyeongju Hospital, Gyeongju, Korea. ptca@dongguk.ac.kr
- KMID: 2224950
- DOI: http://doi.org/10.4070/kcj.2013.43.4.265
Abstract
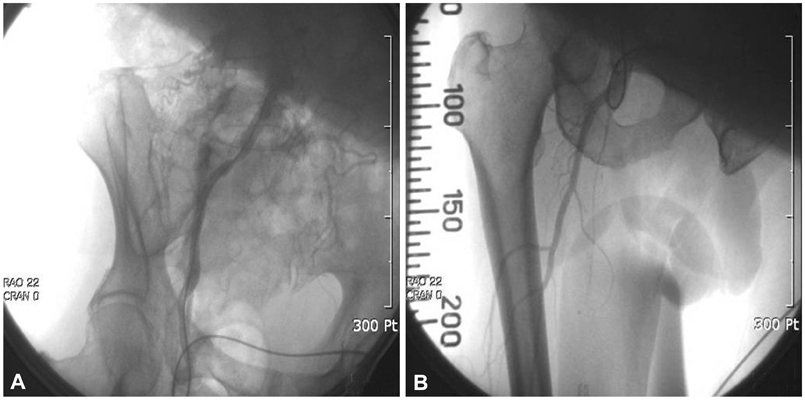
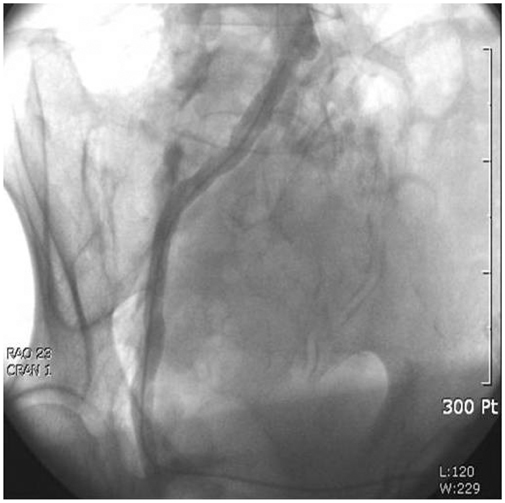
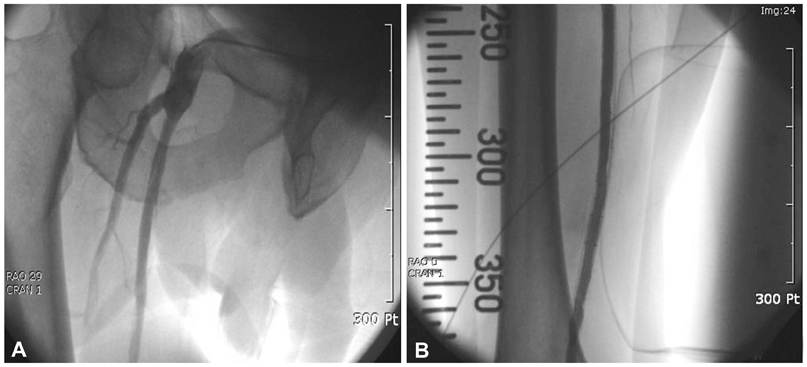
- Peripheral arterial disease represents a significant problem, particularly among the elderly population. There has been great progress made in the treatment of peripheral arterial disease in recent years. Percutaneous transluminal angioplasty (PTA) has been employed as a method of treatment for patients with a variety of peripheral arterial disease. We report our experience with PTA of contralateral common iliac and superficial femoral arteries via graft vessel in a patient with femorofemoral bypass due to ipsilateral iliac artery occlusion.
Keyword
MeSH Terms
Figure
Reference
-
1. Norgren L, Hiatt WR, Dormandy JA, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007. 45:Suppl S. S5–S67.2. Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation. 2004. 110:738–743.3. Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): executive summary a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease) endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. J Am Coll Cardiol. 2006. 47:1239–1312.4. Brosi P, Dick F, Do DD, Schmidli J, Baumgartner I, Diehm N. Revascularization for chronic critical lower limb ischemia in octogenarians is worthwhile. J Vasc Surg. 2007. 46:1198–1207.5. Chang JB, Stein TA. Infrainguinal revascularizations in octogenarians and septuagenarians. J Vasc Surg. 2001. 34:133–138.6. Gallagher MJ, Dixon SR, Safian RD, et al. Safety of percutaneous transfemoral coronary and peripheral procedures via aortofemoral synthetic vascular grafts. Am J Cardiol. 2005. 96:382–385.7. Narins CR. Access strategies for peripheral arterial intervention. Cardiol J. 2009. 16:88–97.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- 2 Cases of Aortoiliac Disease Treated with Strecker Stent Followed by Femoro-Femoral Bypass Graft
- Percutaneous Transluminal Angioplasty of a Stenosis of an Internal Mammary Artery Graft
- A Dual (Brachial and Contralateral Femoral) Approach for Subintimal Angioplasty of Long Ilio-Femoral Occlusive Disease Including the Iliac Ostium
- Combined Angioplasty and Femorofemoral Bypass in the Treatment of Unilateral Iliac Arterial Occlusive Disease
- Patency Rates of Femorofemoral Bypass: Effects of Concomitant Leg Arterial Bypass