Korean Circ J.
2013 Sep;43(9):615-621. 10.4070/kcj.2013.43.9.615.
Utility of Global Strain by Two-Dimensional and Three-Dimensional Speckle Tracking for Assessing Left Ventricular Diastolic Function: Comparison with Pressure Wire Analysis
- Affiliations
-
- 1Division of Cardiology, Inha University College of Medicine, Incheon, Korea. sshin@inha.ac.kr
- KMID: 2224817
- DOI: http://doi.org/10.4070/kcj.2013.43.9.615
Abstract
- BACKGROUND AND OBJECTIVES
We evaluated the utility of two-dimensional (2D) and three-dimensional (3D) left ventricular (LV) global myocardial deformity parameters for assessing LV diastolic function by comparing invasive measures of LV performance.
SUBJECTS AND METHODS
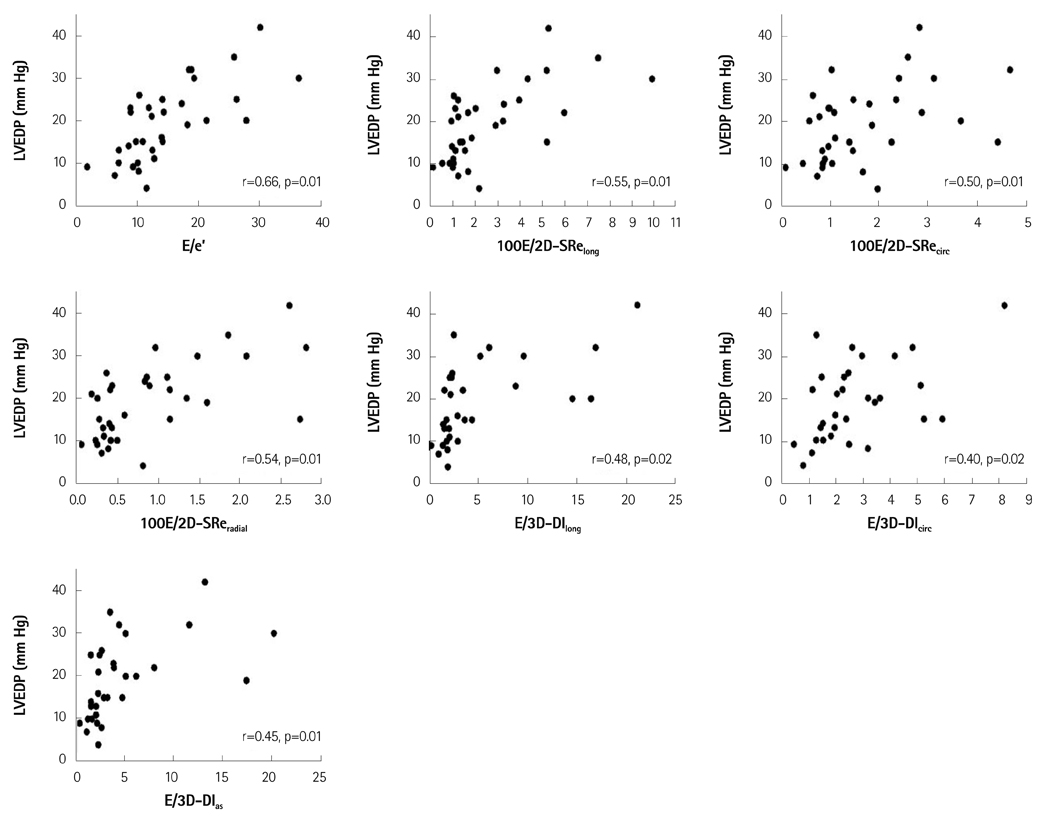
Echocardiography and LV pressure were assessed in 39 patients. Myocardial LV longitudinal, circumferential, and radial deformations, as well as area strain, were evaluated utilizing 2D and 3D speckle tracking software. The 2D early diastolic strain rate (2D-SRe) was measured from the 3 apical and 3 short axis views. The 3D diastolic index (3D-DI) was calculated by the % change of global strain during the first one-third of the diastolic period. LV end diastolic pressure (LVEDP) and the rate of LV pressure change (dP/dt) were collected using a pressure-conducted catheter and tau was calculated.
RESULTS
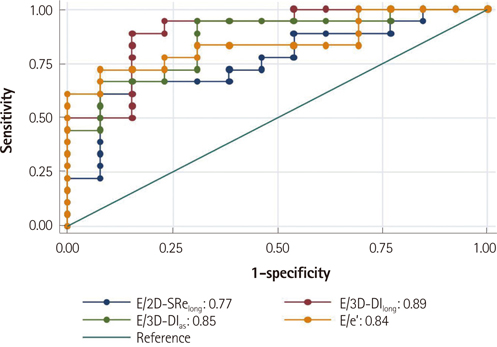
dP/dt(min) were related to early mitral annular velocity (e'), 2D-SRe(long), 2D-SRe(radial), as well as 3D-DI(long), and 3D-DI(as). Additionally, LVEDP was associated with the ratio of mitral early diastolic velocity (E) to 2D-SRe(long), 2D-SRe(circ), 2D-SRe(radial), 3D-DI(long), 3D-DI(circ), and 3D-DI(as). E/2D-SRe(long), E/2D-SRe(radial), E/3D-DI(long), and E/3D-DI(as) were comparable with E/e' in predicting patients with elevated LVEDP. Among those patients with E/e' of 8 to 15, E/3D-DI(long) provided incremental value in identifying those with LVEDP > or =15 mm Hg.
CONCLUSION
2D-SRe(long), 2D-SRe(radial), 3D-DI(long), and 3D-DI(as) were related to LV relaxation, and the ratios of E to those parameters were associated with LVEDP. In addition, among patients with indeterminate E/e', E/3D-DI(long) offered incremental value in predicting elevated LVEDP, suggesting it may provide supplementary information in the evaluation of LV diastolic function.
Keyword
MeSH Terms
Figure
Reference
-
1. Moller JE, Hillis GS, Oh JK, et al. Left atrial volume: a powerful predictor of survival after acute myocardial infarction. Circulation. 2003; 107:2207–2212.2. Pritchett AM, Mahoney DW, Jacobsen SJ, Rodeheffer RJ, Karon BL, Redfield MM. Diastolic dysfunction and left atrial volume: a population-based study. J Am Coll Cardiol. 2005; 45:87–92.3. Anavekar NS, Mirza A, Skali H, et al. Risk assessment in patients with depressed left ventricular function after myocardial infarction using the myocardial performance index--Survival and Ventricular Enlargement (SAVE) experience. J Am Soc Echocardiogr. 2006; 19:28–33.4. Meta-Analysis Research Group in Echocardiography (MeRGE) AMI Collaborators. Møller JE, Whalley GA, et al. Independent prognostic importance of a restrictive left ventricular filling pattern after myocardial infarction: an individual patient meta-analysis: Meta-Analysis Research Group in Echocardiography acute myocardial infarction. Circulation. 2008; 117:2591–2598.5. Sohn DW, Chai IH, Lee DJ, et al. Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol. 1997; 30:474–480.6. Nagueh SF, Appleton CP, Gillebert TC, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr. 2009; 22:107–133.7. Marwick TH. Measurement of strain and strain rate by echocardiography: ready for prime time? J Am Coll Cardiol. 2006; 47:1313–1327.8. Oh JK, Park SJ, Nagueh SF. Established and novel clinical applications of diastolic function assessment by echocardiography. Circ Cardiovasc Imaging. 2011; 4:444–455.9. Ishii K, Suyama T, Imai M, et al. Abnormal regional left ventricular systolic and diastolic function in patients with coronary artery disease undergoing percutaneous coronary intervention: clinical significance of post-ischemic diastolic stunning. J Am Coll Cardiol. 2009; 54:1589–1597.10. Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006; 355:251–259.11. Bhatia RS, Tu JV, Lee DS, et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med. 2006; 355:260–269.12. Penicka M, Bartunek J, Trakalova H, et al. Heart failure with preserved ejection fraction in outpatients with unexplained dyspnea: a pressure-volume loop analysis. J Am Coll Cardiol. 2010; 55:1701–1710.13. Hillis GS, Møller JE, Pellikka PA, et al. Noninvasive estimation of left ventricular filling pressure by E/e' is a powerful predictor of survival after acute myocardial infarction. J Am Coll Cardiol. 2004; 43:360–367.14. Stevenson LW, Tillisch JH, Hamilton M, et al. Importance of hemodynamic response to therapy in predicting survival with ejection fraction less than or equal to 20% secondary to ischemic or nonischemic dilated cardiomyopathy. Am J Cardiol. 1990; 66:1348–1354.15. Ommen SR, Nishimura RA, Appleton CP, et al. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation. 2000; 102:1788–1794.16. Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quiñones MA. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol. 1997; 30:1527–1533.17. Park TH, Nagueh SF, Khoury DS, et al. Impact of myocardial structure and function postinfarction on diastolic strain measurements: implications for assessment of myocardial viability. Am J Physiol Heart Circ Physiol. 2006; 290:H724–H731.18. Pislaru C, Bruce CJ, Anagnostopoulos PC, et al. Ultrasound strain imaging of altered myocardial stiffness: stunned versus infarcted reperfused myocardium. Circulation. 2004; 109:2905–2910.19. Wang J, Khoury DS, Thohan V, Torre-Amione G, Nagueh SF. Global diastolic strain rate for the assessment of left ventricular relaxation and filling pressures. Circulation. 2007; 115:1376–1383.20. Seo Y, Ishizu T, Enomoto Y, et al. Validation of 3-dimensional speckle tracking imaging to quantify regional myocardial deformation. Circ Cardiovasc Imaging. 2009; 2:451–459.21. Mor-Avi V, Lang RM, Badano LP, et al. Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of Echocardiography. J Am Soc Echocardiogr. 2011; 24:277–313.22. Urbano-Moral JA, Patel AR, Maron MS, Arias-Godinez JA, Pandian NG. Three-dimensional speckle-tracking echocardiography: methodological aspects and clinical potential. Echocardiography. 2012; 29:997–1010.23. Urbano-Moral JA, Arias-Godinez JA, Ahmad R, et al. Evaluation of myocardial mechanics with three-dimensional speckle tracking echocardiography in heart transplant recipients: comparison with two-dimensional speckle tracking and relationship with clinical variables. Eur Heart J Cardiovasc Imaging. 2013; [Epub ahead of print].
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status of 3-Dimensional Speckle Tracking Echocardiography: A Review from Our Experiences
- Morning blood pressure surge in the early stage of hypertensive patients impacts three-dimensional left ventricular speckle tracking echocardiography
- Left Ventricular Radial Strain in Children with Dilated Cardiomyopathy: Analyzed with Two Dimensional Speckle Tracking Imaging Method
- Global Circumferential Strain by 2-Dimensional Speckle Tracking Method for the Evaluation of the Left Ventricular Function
- Two-dimensional speckle-tracking of antral contraction in dogs