Korean Circ J.
2013 Nov;43(11):731-738. 10.4070/kcj.2013.43.11.731.
Progressive Dilation of the Left Atrium and Ventricle after Acute Myocardial Infarction Is Associated with High Mortality
- Affiliations
-
- 1The Heart Center of Chonnam National University Hospital, Korea Cardiovascular Stent Research Institute of Chonnam National University, Gwangju, Korea. myungho@chollian.net
- KMID: 2224804
- DOI: http://doi.org/10.4070/kcj.2013.43.11.731
Abstract
- BACKGROUND AND OBJECTIVES
The purpose of this study is to identify the prevalence of progressive dilation in patients with acute myocardial infarction (AMI) combined with heart failure (HF) and determine the prognostic significance and associated factors with a geometric change of an infarcted heart.
SUBJECTS AND METHODS
A total of 1310 AMI patients with HF (63.9+/-12.5 years, 70% male) between November 2005 and April 2011 underwent echocardiography at admission and one year later. Left ventricular (LV) remodeling is defined as 20% progression, and left atria (LA) remodeling is 10% compared with the initial volume index.
RESULTS
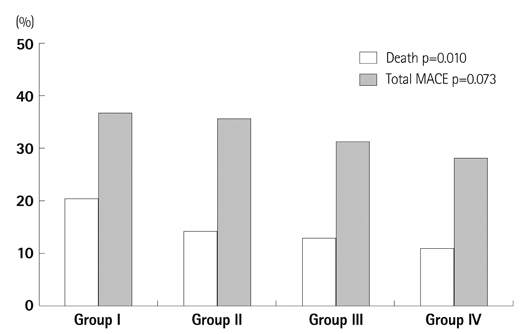
The prevalence of both LA and LV remodeling was 13.9%; LV only was 9.3%, LA only 22.8% and non-remodeling was 55.1%, respectively. In the non-remodeling group, Killip class II was more frequent (83.9%, p<0.001) whereas in other remodeling groups, Killip class III was more frequent. Initial wall motion score index, ejection fraction, maximal cardiac enzyme, high sensitive C-reactive protein, B type natriuretic peptide, and triglyceride serum levels were significantly associated with heart remodeling. All causes of death occurred in 168 cases (12.8%) during the follow-up period. Mortality was the highest in the LV and LA remodeling group (20.9%) and the lowest in the non-remodeling group (11.4%). During the period of follow-up, the cumulative survival rate was significantly lower in the groups of LA and LV remodeling than in others (log rank p=0.006).
CONCLUSION
Total mortality was significantly increased in patients AMI with geometrically progressive LA and LV dilatation.
MeSH Terms
Figure
Cited by 1 articles
-
Therapeutic Hypothermia for Cardioprotection in Acute Myocardial Infarction
In Sook Kang, Ikeno Fumiaki, Wook Bum Pyun
Yonsei Med J. 2016;57(2):291-297. doi: 10.3349/ymj.2016.57.2.291.
Reference
-
1. Gaudron P, Eilles CH, Kugler I, Ertl G. Progressive left ventricular dysfunction and remodeling after myocardial infarction. Potential mechanisms and early predictors. Circulation. 1993; 87:755–763.2. Giannuzzi P, Temporelli PL, Bosimini E, et al. Heterogenity of left ventricular remodeling after myocardial infarction: results of the Gruppo Italiano per lo Studio della Supravvivenza nell Infarcto Miocardico-3 Echo Substudy. Am Heart J. 2001; 141:131–138.3. Cohn JN, Ferrari R, Sharpe N. Cardiac remodeling--concepts and clinical implications: a consensus paper from an international forum on cardiac remodeling. Behalf of an International Forum on Cardiac Remodeling. J Am Coll Cardiol. 2000; 35:569–582.4. Gaudron P, Kugler I, Hu K, Bauer W, Eilles C, Ertl G. Time course of cardiac structural, functional and electrical changes in asymptomatic patients after myocardial infarction: their inter-relation and prognostic impact. J Am Coll Cardiol. 2001; 38:33–40.5. Bolognese L, Neskovic AN, Parodi G, et al. Left ventricular remodeling after primary coronary angioplasty: patterns of left ventricular dilation and long-term prognostic implications. Circulation. 2002; 106:2351–2357.6. Appleton CP, Galloway JM, Gonzalez MS, Gaballa M, Basnight MA. Estimation of left-ventricular filling pressure using two-dimensional and Doppler echocardiography in adult patients with cardiac disease. Additional value of analyzing left atrial size, left atrial ejection fraction and the difference in duration of pulmonary venous and mitral flow velocity at atrial contraction. J Am Coll Cardiol. 1993; 22:1972–1982.7. Basnight MA, Gonzalez MS, Kershenovich SC, Appleton CP. Pulmonary venous flow velocity: relation to hemodynamics, mitral flow velocity and left atrial volume, and ejection fraction. J Am Soc Echocardiogr. 1991; 4:547–558.8. Moller JE, Hillis GS, Oh JK, et al. Left atrial volume: a powerful predictor of survival after acute myocardial infarction. Circulation. 2003; 107:2207–2212.9. Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003; 289:2560–2573.10. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 1997; 27:1183–1197.11. Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004; 110:227–239.12. Hatzitolios AI, Athyros VG, Karagiannis A, et al. Implementation of strategy for the management of overt dyslipidemia: the IMPROVE-dyslipidemia study. Int J Cardiol. 2009; 134:322–329.13. Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction--executive summary A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction). Circulation. 2004; 110:588–636.14. Killip T 3rd, Kimball JT. Treatment of myocardial infarction in a coronary care unit. A two year experience with 250 patients. Am J Cardiol. 1967; 20:457–464.15. Simonson JS, Schiller NB. Descent of the base of the left ventricle: an echocardiographic index of left ventricular. J Am Soc Echocardiogr. 1989; 2:25–35.16. Cerqueira MD, Weissman NJ, Dilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of American Heart Association. Circulation. 2002; 105:539–542.17. Brzezińska B, Loboz-Grudzień K, Sokalski L. Patterns of post-MI left ventricular volume changes - clinical implications. Kardiol Pol. 2007; 65:1190–1198.18. Kuppahally SS, Akoum N, Badger TJ, et al. Echocardiographic left atrial reverse remodeling after catheter ablation of atrial fibrillation is predicted by preablation delayed enhancement of left atrium by magnetic resonance imaging. Am Heart J. 2010; 160:877–884.19. Tiyyagura SR, Pinney S. Left ventricular remodeling after myocardial infarction: past, present, and future. Mt Sinai J Med. 2006; 73:840–851.20. Zimmer HG, Gerdes AM, Lortet S, Mall G. Changes in heart function and cardiac cell size in rats with chronic myocardial infarction. J Mol Cell Cardiol. 1990; 22:1231–1243.21. Rouleau JL, de Champlain J, Klein M, et al. Activation of neurohumoral systems in postinfarction left ventricular dysfunction. J Am Coll Cardiol. 1993; 22:390–398.22. Gerdes AM, Kellerman SE, Moore JA, et al. Structural remodeling of cardiac myocytes in patients with ischemic cardiomyopathy. Circulation. 1992; 86:426–430.23. Sutton MG, Sharpe N. Left ventricular remodeling after myocardial infarction: pathophysiology and therapy. Circulation. 2000; 101:2981–2988.24. Yoon HJ, Jeong MH, Bae JH, et al. Dyslipidemia, low left ventricular ejection fraction and high wall motion score index are predictors of progressive left ventricular dilatation after acute myocardial infarction. Korean Circ J. 2011; 41:124–129.25. Ko JS, Jeong MH, Lee MG, et al. Left ventricular dyssynchrony after acute myocardial infarction is a powerful indicator of left ventricular remodeling. Korean Circ J. 2009; 39:236–242.26. Yun KH, Shin IS, Shin SN, et al. Effect of previous statin therapy in patients with acute coronary syndrome and percutaneous coronary intervention. Korean Circ J. 2011; 41:458–463.27. Eefting FD, Cramer MJ, Stella PRS, Rensing BJ, Doevendans PA. Rational of the REPARATOR study: A randomised trial with serial cardiac MRI follow-up testing the ability of atorvastatin to reduce reperfusion damage after primary PCI for acute MI. Neth Heart J. 2006; 14:95–99.28. Hong YJ, Jeong MH, Hyun DW, et al. Prognostic significance of simvastatin therapy in patients with ischemic heart failure who underwent percutaneous coronary intervention for acute myocardial infarction. Am J Cardiol. 2005; 95:619–622.29. Benjamin EJ, D'Agostino RB, Belanger AJ, Wolf PA, Levy D. Left atrial size and the risk of stroke and death. The Framingham Heart Study. Circulation. 1995; 92:835–841.30. Giannuzzi P, Temporelli PL, Bosimini E, et al. Independent and incremental prognostic value of Doppler-derived mitral deceleration time of early filling in both symptomatic and asymptomatic patients with left ventricular dysfunction. J Am Coll Cardiol. 1996; 28:383–390.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ventricular Remodeling after Acute Myocardial Infarction
- Two Cases of Successful Surgical Treatment of Postmyocardial Infarction Ventricular Septal Defect-Repeated Performation After the First Operation
- Aneurysm of the inferobasal wall and ventricular septal rupture complicated with inferior myocardial infarction
- A Case of a Single Coronary Artery Mimicking Anterior Wall Myocardial Infarction
- A Case of Left Ventricular Pseudoaneurysm Extending to Lateral Side of Left Atrium after Myocardial Infarction