Korean Circ J.
2014 Mar;44(2):82-88. 10.4070/kcj.2014.44.2.82.
Randomized Comparison of the Platelet Inhibitory Efficacy between Low Dose Prasugrel and Standard Dose Clopidogrel in Patients Who Underwent Percutaneous Coronary Intervention
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Inje University College of Medicine, Busan Paik Hospital, Busan, Korea. yangthmd@naver.com
- KMID: 2223896
- DOI: http://doi.org/10.4070/kcj.2014.44.2.82
Abstract
- BACKGROUND AND OBJECTIVES
Increased bleeding rates with standard dose prasugrel have led to increased questions about the effectiveness and safety of the lower maintenance dose. We compared platelet inhibitory efficacy between low dose prasugrel and standard dose clopidogrel in patients on maintenance dose dual antiplatelet therapy.
SUBJECTS AND METHODS
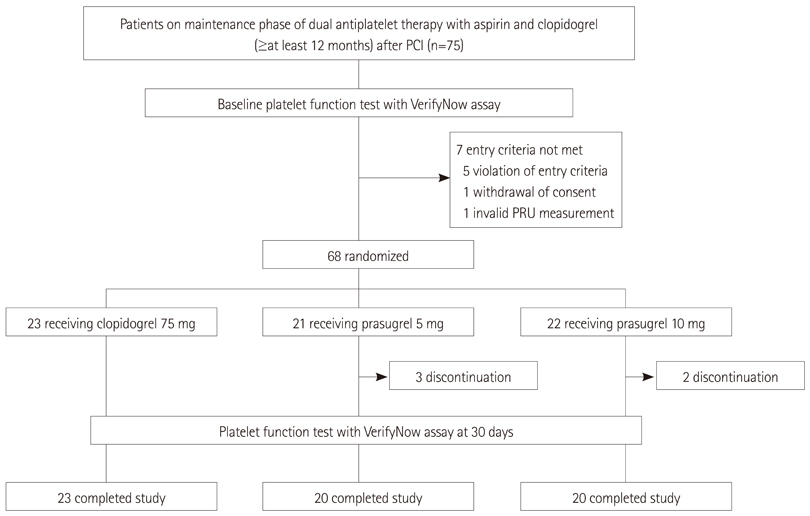
Forty-three patients who underwent percutaneous coronary intervention were randomized to receive 75 mg clopidogrel (n=23) or 5 mg prasugrel (n=20). Another 20 patients were allocated to 10 mg prasugrel as a reference comparison group. All patients (weight, > or =60 kg; age, <75 years) had been receiving 100 mg aspirin and 75 mg clopidogrel daily. The platelet function test was performed at baseline and 30 days after randomization. The primary endpoint was P2Y12 reaction unit (PRU) at 30 days between 5 mg prasugrel and 75 mg clopidogrel.
RESULTS
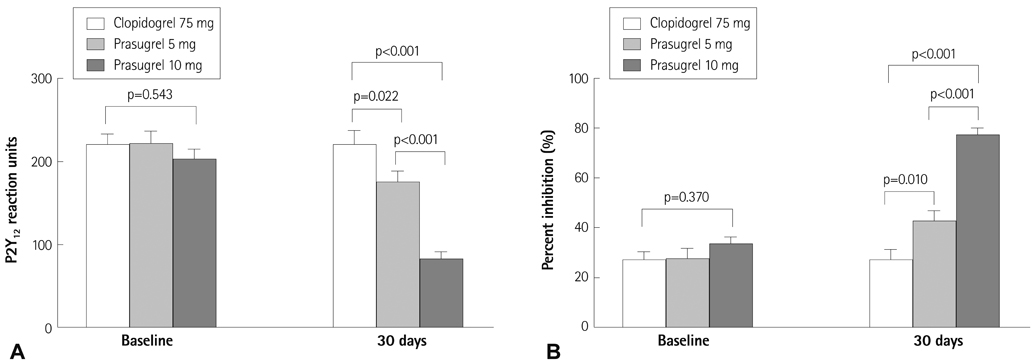
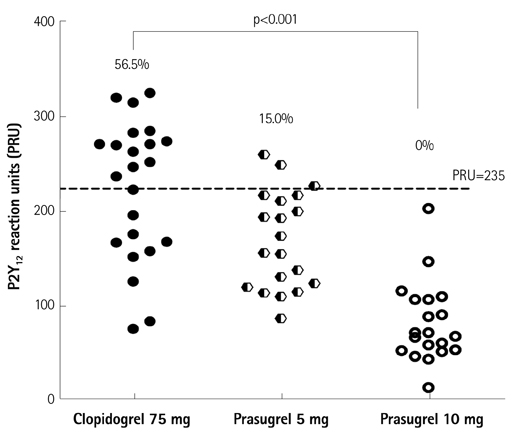
No differences in baseline PRU values were observed among the three groups. The prasugrel (5 mg) group had a significantly lower PRU value compared with that of 75 mg clopidogrel (174.6+/-60.2 vs. 223.4+/-72.9, p=0.022) group at 30 days, whereas the 10 mg prasugrel group showed a lower PRU value (71.9+/-34.4) compared with that of the 5 mg prasugrel (p<0.001). The rate of high on-treatment platelet reactivity (PRU >235) was significant lower in the 5 mg prasugrel group than that in the 75 mg clopidogrel group (15.0% vs. 56.5%, p=0.010).
CONCLUSION
Prasugrel (5 mg) is more potent antiplatelet therapy than 75 mg clopidogrel in non-low body weight and non-elderly patients on a maintenance dose dual antiplatelet therapy.
Keyword
MeSH Terms
Figure
Reference
-
1. Hamm CW, Bassand JP, Agewall S, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2011; 32:2999–3054.2. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011; 124:2574–2609.3. Serebruany VL, Steinhubl SR, Berger PB, Malinin AI, Bhatt DL, Topol EJ. Variability in platelet responsiveness to clopidogrel among 544 individuals. J Am Coll Cardiol. 2005; 45:246–251.4. Mega JL, Close SL, Wiviott SD, et al. Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med. 2009; 360:354–362.5. Buonamici P, Marcucci R, Migliorini A, et al. Impact of platelet reactivity after clopidogrel administration on drug-eluting stent thrombosis. J Am Coll Cardiol. 2007; 49:2312–2317.6. Cuisset T, Frere C, Quilici J, et al. Predictive values of post-treatment adenosine diphosphate-induced aggregation and vasodilator-stimulated phosphoprotein index for stent thrombosis after acute coronary syndrome in clopidogrel-treated patients. Am J Cardiol. 2009; 104:1078–1082.7. Jin HY, Yang TH, Kim DI, et al. High post-clopidogrel platelet reactivity assessed by a point-of-care assay predicts long-term clinical outcomes in patients with ST-segment elevation myocardial infarction who underwent primary coronary stenting. Int J Cardiol. 2013; 167:1877–1881.8. Parodi G, Marcucci R, Valenti R, et al. High residual platelet reactivity after clopidogrel loading and long-term cardiovascular events among patients with acute coronary syndromes undergoing PCI. JAMA. 2011; 306:1215–1223.9. Brandt JT, Payne CD, Wiviott SD, et al. A comparison of prasugrel and clopidogrel loading doses on platelet function: magnitude of platelet inhibition is related to active metabolite formation. Am Heart J. 2007; 153:66.e9–66.e16.10. Jernberg T, Payne CD, Winters KJ, et al. Prasugrel achieves greater inhibition of platelet aggregation and a lower rate of non-responders compared with clopidogrel in aspirin-treated patients with stable coronary artery disease. Eur Heart J. 2006; 27:1166–1173.11. Wiviott SD, Trenk D, Frelinger AL, et al. Prasugrel compared with high loading- and maintenance-dose clopidogrel in patients with planned percutaneous coronary intervention: the Prasugrel in Comparison to Clopidogrel for Inhibition of Platelet Activation and Aggregation-Thrombolysis in Myocardial Infarction 44 trial. Circulation. 2007; 116:2923–2932.12. Michelson AD, Frelinger AL 3rd, Braunwald E, et al. Pharmacodynamic assessment of platelet inhibition by prasugrel vs. clopidogrel in the TRITON-TIMI 38 trial. Eur Heart J. 2009; 30:1753–1763.13. Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007; 357:2001–2015.14. Erlinge D, Ten Berg J, Foley D, et al. Reduction in platelet reactivity with prasugrel 5 mg in low-body-weight patients is noninferior to prasugrel 10 mg in higher-body-weight patients: results from the FEATHER trial. J Am Coll Cardiol. 2012; 60:2032–2040.15. Erlinge D, Gurbel PA, James S, et al. Prasugrel 5 mg in the very elderly attenuates platelet inhibition but maintains noninferiority to prasugrel 10 mg in nonelderly patients: the GENERATIONS trial, a pharmacodynamic and pharmacokinetic study in stable coronary artery disease patients. J Am Coll Cardiol. 2013; 62:577–583.16. Varenhorst C, James S, Erlinge D, et al. Assessment of P2Y(12) inhibition with the point-of-care device VerifyNow P2Y12 in patients treated with prasugrel or clopidogrel coadministered with aspirin. Am Heart J. 2009; 157:562.e1–562.e9.17. Price MJ, Endemann S, Gollapudi RR, et al. Prognostic significance of post-clopidogrel platelet reactivity assessed by a point-of-care assay on thrombotic events after drug-eluting stent implantation. Eur Heart J. 2008; 29:992–1000.18. Bonello L, Tantry US, Marcucci R, et al. Consensus and future directions on the definition of high on-treatment platelet reactivity to adenosine diphosphate. J Am Coll Cardiol. 2010; 56:919–933.19. Roe MT, Armstrong PW, Fox KA, et al. Prasugrel versus clopidogrel for acute coronary syndromes without revascularization. N Engl J Med. 2012; 367:1297–1309.20. Stone GW, Witzenbichler B, Weisz G, et al. Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): a prospective multicentre registry study. Lancet. 2013; 382:614–623.21. Unger EF. Weighing benefits and risks--the FDA's review of prasugrel. N Engl J Med. 2009; 361:942–945.22. Wiviott SD, Antman EM, Braunwald E. Prasugrel. Circulation. 2010; 122:394–403.23. Fifth Organization to Assess Strategies in Acute Ischemic Syndromes Investigators. Yusuf S, Mehta SR, et al. Comparison of fondaparinux and enoxaparin in acute coronary syndromes. N Engl J Med. 2006; 354:1464–1476.24. Eikelboom JW, Mehta SR, Anand SS, Xie C, Fox KA, Yusuf S. Adverse impact of bleeding on prognosis in patients with acute coronary syndromes. Circulation. 2006; 114:774–782.25. Mehran R, Pocock SJ, Stone GW, et al. Associations of major bleeding and myocardial infarction with the incidence and timing of mortality in patients presenting with non-ST-elevation acute coronary syndromes: a risk model from the ACUITY trial. Eur Heart J. 2009; 30:1457–1466.26. Wiviott SD, Desai N, Murphy SA, et al. Efficacy and safety of intensive antiplatelet therapy with prasugrel from TRITON-TIMI 38 in a core clinical cohort defined by worldwide regulatory agencies. Am J Cardiol. 2011; 108:905–911.27. Gurbel PA, Erlinge D, Ohman EM, et al. Platelet function during extended prasugrel and clopidogrel therapy for patients with ACS treated without revascularization: the TRILOGY ACS platelet function substudy. JAMA. 2012; 308:1785–1794.28. Small DS, Farid NA, Payne CD, et al. Effect of intrinsic and extrinsic factors on the clinical pharmacokinetics and pharmacodynamics of prasugrel. Clin Pharmacokinet. 2010; 49:777–798.29. Li YG, Ni L, Brandt JT, et al. Inhibition of platelet aggregation with prasugrel and clopidogrel: an integrated analysis in 846 subjects. Platelets. 2009; 20:316–327.30. Breet NJ, van Werkum JW, Bouman HJ, et al. Comparison of platelet function tests in predicting clinical outcome in patients undergoing coronary stent implantation. JAMA. 2010; 303:754–762.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lower Loading Dose of Prasugrel Compared with Conventional Loading Doses of Clopidogrel and Prasugrel in Korean Patients Undergoing Elective Coronary Angiography: A Randomized Controlled Study Evaluating Pharmacodynamic Efficacy
- New Oral Antiplatelet Agents
- Low-Dose Prasugrel in Patients with Resistance to Clopidogrel for the Treatment of Cerebral Aneurysms
- Oral antiplatelet agent hypersensitivity and cross-reactivity managed by successful desensitisation
- De-Escalation of P2Yâ‚â‚‚ Receptor Inhibitor Therapy after Acute Coronary Syndromes in Patients Undergoing Percutaneous Coronary Intervention