Korean Circ J.
2015 Sep;45(5):398-407. 10.4070/kcj.2015.45.5.398.
Relationship between Right Ventricular Longitudinal Strain, Invasive Hemodynamics, and Functional Assessment in Pulmonary Arterial Hypertension
- Affiliations
-
- 1Department of Cardiovascular Medicine, Heart and Vascular Institute, Cleveland Clinic, Cleveland, Ohio, USA. popoviz@ccf.org
- 2Cardiology Division of Internal Medicine, Chungnam National University, Chungnam National University Hospital, Daejeon, Korea.
- 3Department of Cardiovascular Medicine, Tokushima University Hospital, Tokushima, Japan.
- 4Department of Pathobiology, Lerner Research Institute, Cleveland Clinic, Cleveland, Ohio, USA.
- 5Pulmonary and Critical Care Medicine, Respiratory Institute, Cleveland Clinic, Cleveland, Ohio, USA.
- 6Menzies Research Institute, Tasmania, Australia.
- KMID: 2223804
- DOI: http://doi.org/10.4070/kcj.2015.45.5.398
Abstract
- BACKGROUND AND OBJECTIVES
Right ventricular longitudinal strain (RVLS) is a new parameter of RV function. We evaluated the relationship of RVLS by speckle-tracking echocardiography with functional and invasive parameters in pulmonary arterial hypertension (PAH) patients.
SUBJECTS AND METHODS
Thirty four patients with World Health Organization group 1 PAH (29 females, mean age 45+/-13 years old). RVLS were analyzed with velocity vector imaging.
RESULTS
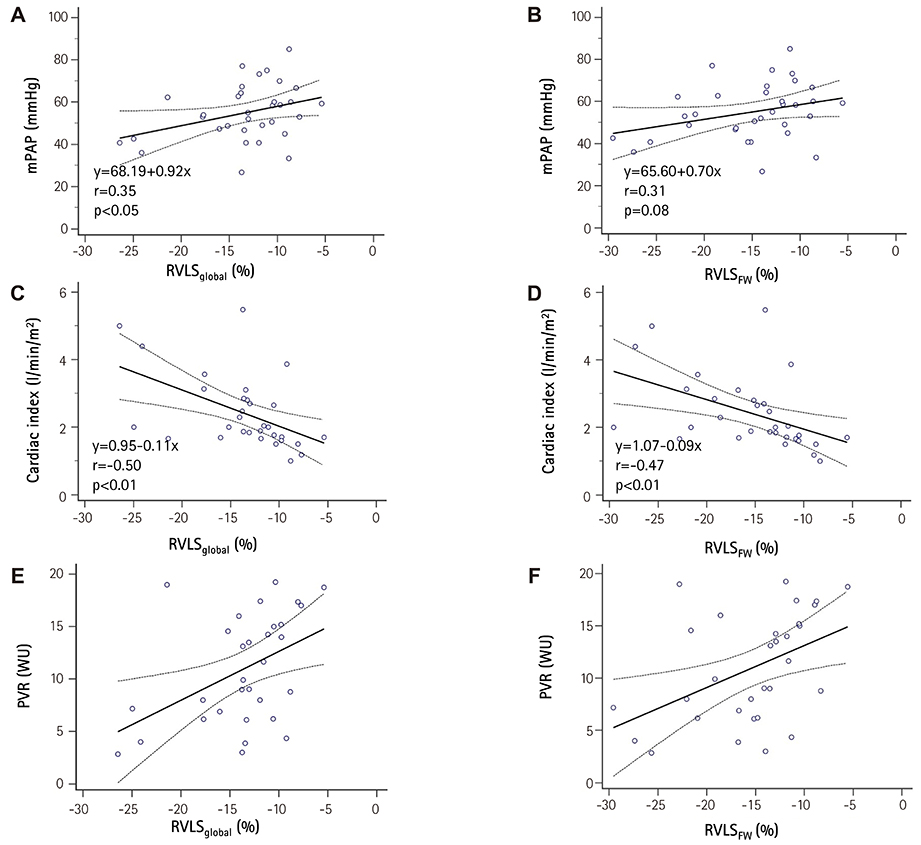
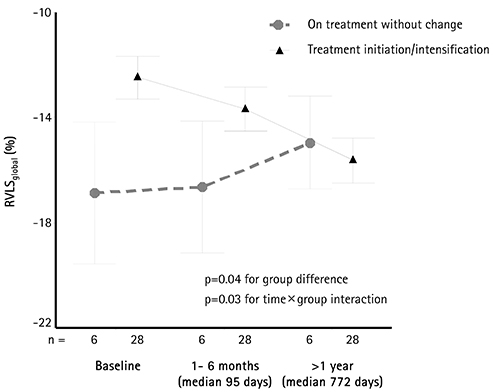
Patients with advanced symptoms {New York Heart Association (NYHA) functional class III/IV} had impaired RVLS in global RV (RVLS(global), -17+/-5 vs. -12+/-3%, p<0.01) and RV free wall (RVLS(FW), -19+/-5 vs. -14+/-4%, p<0.01 to NYHA class I/II). Baseline RVLS(global) and RVLS(FW) showed significant correlation with 6-minute walking distance (r=-0.54 and r=-0.57, p<0.01 respectively) and logarithmic transformation of brain natriuretic peptide concentration (r=0.65 and r=0.65, p<0.01, respectively). These revealed significant correlations with cardiac index (r=-0.50 and r=-0.47, p<0.01, respectively) and pulmonary vascular resistance (PVR, r=0.45 and r=0.45, p=0.01, respectively). During a median follow-up of 33 months, 25 patients (74%) had follow-up examinations. Mean pulmonary arterial pressure (mPAP, 54+/-13 to 46+/-16 mmHg, p=0.03) and PVR (11+/-5 to 6+/-2 wood units, p<0.01) were significantly decreased with pulmonary vasodilator treatment. RVLS(global) (-12+/-5 to -16+/-5%, p<0.01) and RVLS(FW) (-14+/-5 to -18+/-5%, p<0.01) were significantly improved. The decrease of mPAP was significantly correlated with improvement of RVLS(global) (r=0.45, p<0.01) and RVLS(FW) (r=0.43, p<0.01). The PVR change demonstrated significant correlation with improvement of RVLS(global) (r=0.40, p<0.01).
CONCLUSION
RVLS correlates with functional and invasive hemodynamic parameters in PAH patients. Decrease of mPAP and PVR as a result of treatment was associated with improvement of RVLS.
MeSH Terms
Figure
Cited by 2 articles
-
Two-dimensional Echocardiographic Assessment of Myocardial Strain: Important Echocardiographic Parameter Readily Useful in Clinical Field
Jae-Hyeong Park
Korean Circ J. 2019;49(10):908-931. doi: 10.4070/kcj.2019.0200.Strain Analysis of the Right Ventricle Using Two-dimensional Echocardiography
Ju-Hee Lee, Jae-Hyeong Park
J Cardiovasc Imaging. 2018;26(3):111-124. doi: 10.4250/jcvi.2018.26.e11.
Reference
-
1. Humbert M, Sitbon O, Simonneau G. Treatment of pulmonary arterial hypertension. N Engl J Med. 2004; 351:1425–1436.2. Bogaard HJ, Abe K, Vonk Noordegraaf A, Voelkel NF. The right ventricle under pressure: cellular and molecular mechanisms of right-heart failure in pulmonary hypertension. Chest. 2009; 135:794–804.3. D'Alonzo GE, Barst RJ, Ayres SM, et al. Survival in patients with primary pulmonary hypertension. Results from a national prospective registry. Ann Intern Med. 1991; 115:343–349.4. Barst RJ, Rubin LJ, Long WA, et al. A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension. N Engl J Med. 1996; 334:296–301.5. Channick RN, Simonneau G, Sitbon O, et al. Effects of the dual endothelin-receptor antagonist bosentan in patients with pulmonary hypertension: a randomised placebo-controlled study. Lancet. 2001; 358:1119–1123.6. Sachdev A, Villarraga HR, Frantz RP, et al. Right ventricular strain for prediction of survival in patients with pulmonary arterial hypertension. Chest. 2011; 139:1299–1309.7. Brown SB, Raina A, Katz D, Szerlip M, Wiegers SE, Forfia PR. Longitudinal shortening accounts for the majority of right ventricular contraction and improves after pulmonary vasodilator therapy in normal subjects and patients with pulmonary arterial hypertension. Chest. 2011; 140:27–33.8. Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010; 23:685–713.9. Giusca S, Dambrauskaite V, Scheurwegs C, et al. Deformation imaging describes right ventricular function better than longitudinal displacement of the tricuspid ring. Heart. 2010; 96:281–288.10. Jamal F, Bergerot C, Argaud L, Loufouat J, Ovize M. Longitudinal strain quantitates regional right ventricular contractile function. Am J Physiol Heart Circ Physiol. 2003; 285:H2842–H2847.11. Verhaert D, Mullens W, Borowski A, et al. Right ventricular response to intensive medical therapy in advanced decompensated heart failure. Circ Heart Fail. 2010; 3:340–346.12. Pirat B, McCulloch ML, Zoghbi WA. Evaluation of global and regional right ventricular systolic function in patients with pulmonary hypertension using a novel speckle tracking method. Am J Cardiol. 2006; 98:699–704.13. Galiè N, Hoeper MM, Humbert M, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension: the task force for the diagnosis and treatment of pulmonary hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the International Society of Heart and Lung Transplantation (ISHLT). Eur Heart J. 2009; 30:2493–2537.14. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005; 18:1440–1463.15. ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002; 166:111–117.16. Yuan XP, Bach D, Skanes A, Drangova M. Assessment of intra- and interobserver variability of pulmonary vein measurements from CT angiography. Acad Radiol. 2004; 11:1211–1218.17. Puwanant S, Park M, Popović ZB, et al. Ventricular geometry, strain, and rotational mechanics in pulmonary hypertension. Circulation. 2010; 121:259–266.18. Fine NM, Chen L, Bastiansen PM, et al. Outcome prediction by quantitative right ventricular function assessment in 575 subjects evaluated for pulmonary hypertension. Circ Cardiovasc Imaging. 2013; 6:711–721.19. Parent F, Bachir D, Inamo J, et al. A hemodynamic study of pulmonary hypertension in sickle cell disease. N Engl J Med. 2011; 365:44–53.20. Rich S, Kaufmann E, Levy PS. The effect of high doses of calcium-channel blockers on survival in primary pulmonary hypertension. N Engl J Med. 1992; 327:76–81.21. Hoeper MM, Lee SH, Voswinckel R, et al. Complications of right heart catheterization procedures in patients with pulmonary hypertension in experienced centers. J Am Coll Cardiol. 2006; 48:2546–2552.22. Beygui F, Furber A, Delépine S, et al. Routine breath-hold gradient echo MRI-derived right ventricular mass, volumes and function: accuracy, reproducibility and coherence study. Int J Cardiovasc Imaging. 2004; 20:509–516.23. Torbicki A. Cardiac magnetic resonance in pulmonary arterial hypertension: a step in the right direction. Eur Heart J. 2007; 28:1187–1189.24. Vonk Noordegraaf A, Galiè N. The role of the right ventricle in pulmonary arterial hypertension. Eur Respir Rev. 2011; 20:243–253.25. Haeck ML, Scherptong RW, Marsan NA, et al. Prognostic value of right ventricular longitudinal peak systolic strain in patients with pulmonary hypertension. Circ Cardiovasc Imaging. 2012; 5:628–636.26. Miyamoto S, Nagaya N, Satoh T, et al. Clinical correlates and prognostic significance of six-minute walk test in patients with primary pulmonary hypertension. Comparison with cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2000; 161(2 Pt 1):487–492.27. Galiè N, Manes A, Negro L, et al. A meta-analysis of randomized controlled trials in pulmonary arterial hypertension. Eur Heart J. 2009; 30:394–403.28. Gomberg-Maitland M, Dufton C, Oudiz RJ, Benza RL. Compelling evidence of long-term outcomes in pulmonary arterial hypertension? A clinical perspective. J Am Coll Cardiol. 2011; 57:1053–1061.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Right Ventricular Longitudinal Strain: A Target Indicator in the Treatment of Pulmonary Arterial Hypertension
- Erratum: Relationship between Right Ventricular Longitudinal Strain, Invasive Hemodynamics, and Functional Assessment in Pulmonary Arterial Hypertension
- Diagnosis and treatment of idiopathic pulmonary arterial hypertension
- Diagnosis and assessment of pulmonary arterial hypertension
- Echocardiographic Screening Methods for Pulmonary Hypertension: A Practical Review