J Rheum Dis.
2014 Dec;21(6):336-339. 10.4078/jrd.2014.21.6.336.
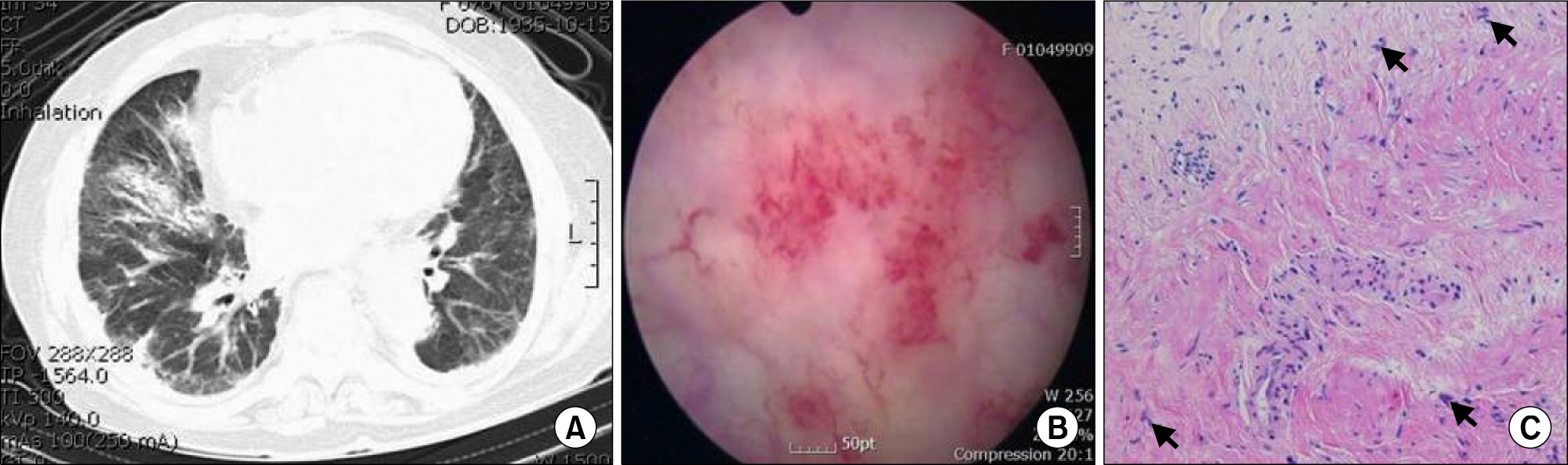
Hemorrhagic Cystitis with Giant Cells in Rheumatoid Arthritis Treating with Tacrolimus
- Affiliations
-
- 1Department of Rheumatology, Chonbuk National University Medical School and Research Institute of Clinical Medicine of Chonbuk National University Hospital-Chonbuk National University, Jeonju, Korea. ywhim@jbnu.ac.kr
- KMID: 2222941
- DOI: http://doi.org/10.4078/jrd.2014.21.6.336
Abstract
- Hemorrhagic cystitis is a diffuse inflammation of the mucosa of the bladder, characterized by hematuria and burning upon urination. This might be caused by a variety of reasons, including undergoing chemotherapy (such as cyclophosphamide), radiation therapy, bladder cancer, certain viruses, urinary infections, and thrombocytopenia. There are no previous reports of hemorrhagic cystitis associated with the use of tacrolimus. This is the first case of hemorrhagic cystitis due to tacrolimus for the treatment of rheumatoid arthritis. We describe a case of hemorrhagic cystitis with giant cells in a patient with rheumatoid arthritis treating with tacrolimus. Hematuria resolved spontaneously with discontinuation of the drug.
MeSH Terms
Figure
Reference
-
1. Russo P. Urologic emergencies in the cancer patient. Semin Oncol. 2000; 27:284–98.2. Nguyen ML, Borochovitz D, Thomas G, McClure T, Ruben FL. Hemorrhagic cystitis with herpes simplex virus type 2 in the bladder mucosa. Clin Infect Dis. 1992; 14:767–8.
Article3. Drake MJ, Nixon PM, Crew JP. Drug-induced bladder and urinary disorders. Incidence, prevention and management. Drug Saf. 1998; 19:45–55.4. Levine LA, Richie JP. Urological complications of cyclophosphamide. J Urol. 1989; 141:1063–9.
Article5. Brügger-Andersen T, Reiersen R. A 34-year-old man with hemorrhagic cystitis. Tidsskr Nor Laegeforen. 2004; 124:3075–7.6. Andriole GL, Brickman C, Lack EE, Sesterhenn IA, Javadpour N, Linehan WM, et al. Danazol-induced cystitis: an undescribed source of hematuria in patients with hereditary angioneurotic edema. J Urol. 1986; 135:44–6.
Article7. Martinez-Suarez HJ, Wang R, Faerber GJ. Atorvastatin-induced hemorrhagic cystitis: a case report. Urology. 2009; 73:681.
Article8. Sakuma S, Kato Y, Nishigaki F, Sasakawa T, Magari K, Miyata S, et al. FK506 potently inhibits T cell activation induced TNF-alpha and IL-1beta production in vitro by human peripheral blood mononuclear cells. Br J Pharmacol. 2000; 130:1655–63.9. Takeuchi T, Kawai S, Yamamoto K, Harigai M, Ishida K, Miyasaka N. Postmarketing surveillance of the safety and effectiveness of tacrolimus in 3,267 Japanese patients with rheumatoid arthritis. Mod Rheumatol. 2014; 24:8–16.
Article10. Nakamura T, Yamamura Y, Tomoda K, Tsukano M, Baba S. Massive hematuria due to bladder amyloidosis in patients with rheumatoid arthritis: three case reports. Clin Exp Rheumatol. 2003; 21:673–4.11. Droller MJ, Saral R, Santos G. Prevention of cyclophosphamide-induced hemorrhagic cystitis. Urology. 1982; 20:256–8.
Article12. Grignon DJ, Sakr W. Inflammatory and other conditions that can mimic carcinoma in the urinary bladder. Pathol Annu. 1995; 30:95–122.13. Kopterides P, Theodorakopoulou M, Mentzelopoulos S, Armaganidis A. Cyclophosphamide-induced hemorrhagic cystitis successfully treated with conjugated estrogens. Am J Hematol. 2005; 80:166–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Add-on Clarithromycin and Tacrolimus Treatment for Rheumatoid Arthritis
- Cytologic Findings of Rheumatoid Pleuritis in Pleural Effusion: A Case Report
- A Case of Multicentric Reticulohistiocytosis Misdiagnosed as Rheumatoid Arthritis
- A Case of Rheumatoid Arthritis accompanied by Organizing Pneumonia Successfully Treated with Prednisolone, Clarithromycin and Tacrolimus
- Synovial Chondromatosis in Knee Masquerading as Tuberculosis Arthritis