Ann Dermatol.
2009 May;21(2):185-188. 10.5021/ad.2009.21.2.185.
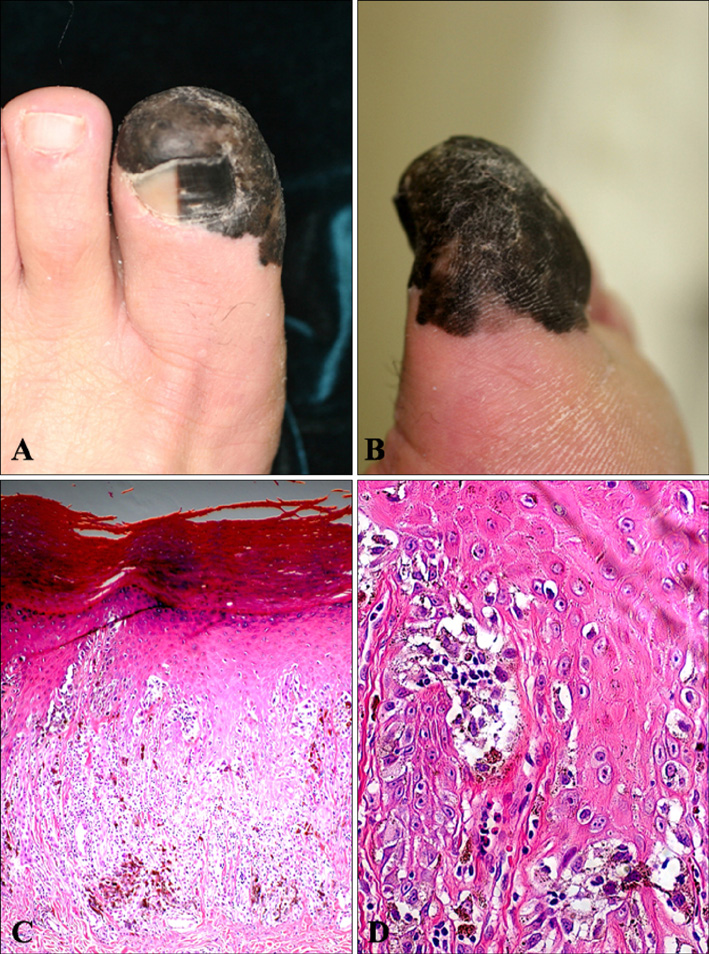
Progression from Acral Lentiginous Melanoma in situ to Invasive Acral Lentiginous Melanoma
- Affiliations
-
- 1Department of Dermatology, Seoul St. Mary`s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. yymmpark6301@ hotmail.com
- KMID: 2219393
- DOI: http://doi.org/10.5021/ad.2009.21.2.185
Abstract
- Acral lentiginous melanoma (ALM) is the most common type of cutaneous melanoma in Asians. The very early stage of ALM demonstrates only a proliferation of a few atypical melanocytes within the epidermis, and has been termed ALM in situ. A 74-year-old male patient presented with a pigmented lesion on the left great toe for 12 years, which had initially showed only a few scattered hyperplastic atypical melanocytes without dermal invasion upon biopsy 5 years ago. This time however, rebiopsy of the lesion confirmed a diagnosis of ALM, stage IIIB. It could be inferred that the lesion had slowly progressed from ALM in situ to invasive ALM over a period of 12 years. Herein we report a case of ALM in situ which progressed to invasive ALM over a long period of time. We expect this report may assist physicians in early recognition and proper management of future cases of ALM in situ.
Figure
Cited by 1 articles
-
Double Primary Acral Lentiginous Melanoma of both Soles
Jae Ho Lee, Youngkyung Lim, You Jin Lee, Ji-Hye Park, Dong-Youn Lee
Ann Dermatol. 2017;29(1):129-131. doi: 10.5021/ad.2017.29.1.129.
Reference
-
1. Seiji M, Takematsu H, Hosokawa M, Obata M, Tomita Y, Kato T, et al. Acral melanoma in Japan. J Invest Dermatol. 1983. 80:Suppl. 56s–60s.
Article2. Cho KH, Kim BS, Chang SH, Lee YS, Kim KJ. Pigmented nail with atypical melanocytic hyperplasia. Clin Exp Dermatol. 1991. 16:451–454.
Article3. Nogita T, Wong TY, Ohara K, Mizushima J, Mihm MC Jr, Kawashima M. Atypical melanosis of the foot. A report of three cases in Japanese populations. Arch Dermatol. 1994. 130:1042–1045.
Article4. Saida T. Malignant melanoma in situ on the sole of the foot. Its clinical and histopathologic characteristics. Am J Dermatopathol. 1989. 11:124–130.5. Kwon IH, Lee JH, Cho KH. Acral lentiginous melanoma in situ: a study of nine cases. Am J Dermatopathol. 2004. 26:285–289.
Article6. Rhodes AR, Mihm MC Jr, Weinstock MA. Dysplastic melanocytic nevi: a reproducible histologic definition emphasizing cellular morphology. Mod Pathol. 1989. 2:306–319.7. Frankel KA. Intraepithelial melanocytic neoplasia: a classification by pattern analysis of proliferations of atypical melanocytes. Am J Dermatopathol. 1987. 9:80–81.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acral Lentiginous Melanoma in situ
- Acral Lentiginous Melanoma Developing during Long-standing Atypical Melanosis: Usefulness of Dermoscopy for Detection of Early Acral Melanoma
- A Case of Acral Lentiginous Melanoma
- Acral Lentiginous Melanoma, Indolent Subtype Diagnosed by En Bloc Excision: A Case Report
- A Case of Thin Acral Lentiginous Melanoma with Lymph Node Metastasis and Regression