Allergy Asthma Respir Dis.
2015 Nov;3(6):456-460. 10.4168/aard.2015.3.6.456.
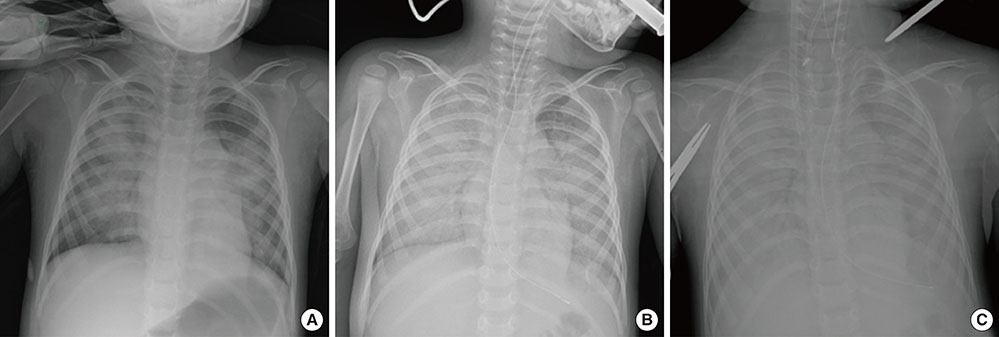
Life-threatening human metapneumovirus pneumonia requiring extracorporeal membrane oxygenation in a 26-month-old child
- Affiliations
-
- 1Department of Pediatrics, Yonsei University College of Medicine, Seoul, Korea. yhkim@yuhs.ac
- 2Institute of Allergy, Yonsei University College of Medicine, Seoul, Korea.
- 3Division of Cardiovascular Surgery, Congenital Heart Disease Center, Severance Cardiovascular Hospital, Department of Thoracic and Cardiovascular Surgery, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2218637
- DOI: http://doi.org/10.4168/aard.2015.3.6.456
Abstract
- We present the first case report of a child with human metapneumovirus (hMPV) pneumonia who survived by extracorporeal membrane oxygenation (ECMO) in Korea. A 26-month-old boy with a previous history of Lennox-Gastaut syndrome and delayed development suffered from respiratory failure after 4 days of fever, cough, and sputum. The boy underwent intubation and required ECMO application due to failure of conventional mechanical ventilation. He was on the ECMO support for 7 days. To our knowledge, this is the shortest period reported for ECMO application among successfully treated patients with hMPV infection accompanied by acute respiratory distress syndrome. This case highlights 2 clinical implications: the potentially fatal causative role of hMPV in respiratory failure in a pediatric population and the timely utilization of ECMO.
Keyword
MeSH Terms
Figure
Reference
-
1. Arnold JC, Singh KK, Spector SA, Sawyer MH. Undiagnosed respiratory viruses in children. Pediatrics. 2008; 121:e631–e637.
Article2. Allander T, Tammi MT, Eriksson M, Bjerkner A, Tiveljung-Lindell A, Andersson B. Cloning of a human parvovirus by molecular screening of respiratory tract samples. Proc Natl Acad Sci U S A. 2005; 102:12891–12896.
Article3. van den Hoogen BG, de Jong JC, Groen J, Kuiken T, de Groot R, Fouchier RA, et al. A newly discovered human pneumovirus isolated from young children with respiratory tract disease. Nat Med. 2001; 7:719–724.
Article4. Panda S, Mohakud NK, Pena L, Kumar S. Human metapneumovirus: review of an important respiratory pathogen. Int J Infect Dis. 2014; 25:45–52.
Article5. Principi N, Esposito S. Paediatric human metapneumovirus infection: epidemiology, prevention and therapy. J Clin Virol. 2014; 59:141–147.
Article6. Ghani AS, Morrow BM, Hardie DR, Argent AC. An investigation into the prevalence and outcome of patients admitted to a pediatric intensive care unit with viral respiratory tract infections in Cape Town, South Africa. Pediatr Crit Care Med. 2012; 13:e275–e281.
Article7. Ulloa-Gutierrez R, Skippen P, Synnes A, Seear M, Bastien N, Li Y, et al. Life-threatening human metapneumovirus pneumonia requiring extracorporeal membrane oxygenation in a preterm infant. Pediatrics. 2004; 114:e517–e519.
Article8. Schlapbach LJ, Agyeman P, Hutter D, Aebi C, Wagner BP, Riedel T. Human metapneumovirus infection as an emerging pathogen causing acute respiratory distress syndrome. J Infect Dis. 2011; 203:294–295.
Article9. Evashuk KM, Forgie SE, Gilmour S, Huynh H, Lee BE, Robinson JL. Respiratory failure associated with human metapneumovirus infection in an infant posthepatic transplant. Am J Transplant. 2008; 8:1567–1569.
Article10. Gupta A, Bembea M, Brown A, Robertson C, Romer L, Cohn RD. Respiratory failure secondary to human metapneumovirus requiring extracorporeal membrane oxygenation in a 32-month-old child. Case Rep Pediatr. 2012; 2012:268074.
Article11. Schmidt M, Bailey M, Sheldrake J, Hodgson C, Aubron C, Rycus PT, et al. Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure. The Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score. Am J Respir Crit Care Med. 2014; 189:1374–1382.
Article12. van Rijckevorsel K. Cognitive problems related to epilepsy syndromes, especially malignant epilepsies. Seizure. 2006; 15:227–234.
Article13. Brogan TV, Thiagarajan RR, Rycus PT, Bartlett RH, Bratton SL. Extracorporeal membrane oxygenation in adults with severe respiratory failure: a multi-center database. Intensive Care Med. 2009; 35:2105–2114.
Article14. Dalton HJ, Macrae DJ. Pediatric Acute Lung Injury Consensus Conference Group. Extracorporeal support in children with pediatric acute respiratory distress syndrome: proceedings from the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med. 2015; 16:5 Suppl 1. S111–S117.15. Chen H, Yu RG, Yin NN, Zhou JX. Combination of extracorporeal membrane oxygenation and continuous renal replacement therapy in critically ill patients: a systematic review. Crit Care. 2014; 18:675.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- 2009 H1N1 influenza virus infection and necrotizing pneumonia treated with extracorporeal membrane oxygenation
- A 35-month-old boy who ingested laundry detergent pods and underwent veno-pulmonary extracorporeal membrane oxygenation support
- Emergency Bilobectomy under the Extracorporeal Membrane Oxygenation Support for Pediatric Patient with Blunt Traumatic Bronchial Transection: A case report
- Extracorporeal Membrane Oxygenation for Complicated Scrub Typhus
- Extracorporeal Membrane Oxygenation Therapy for Aspiration Pneumonia in a Patient following Left Pneumonectomy for Lung Cancer