J Korean Ophthalmol Soc.
2014 Mar;55(3):325-332. 10.3341/jkos.2014.55.3.325.
The Clinical Features of Ocular Myasthenia Gravis in Thyroid-Associated Ophthalmopathy
- Affiliations
-
- 1Department of Ophthalmology, Dong-A University College of Medicine, Busan, Korea. hbahn@dau.ac.kr
- KMID: 2218257
- DOI: http://doi.org/10.3341/jkos.2014.55.3.325
Abstract
- PURPOSE
There are some challenges to accurate diagnosis of ocular myasthenia gravis (MG) in thyroid-associated ophthalmopathy (TAO) patients because the clinical features of these diseases are similar. The aim of this study was to discuss the clinical features and treatment options that may help differentiate these 2 diseases.
METHODS
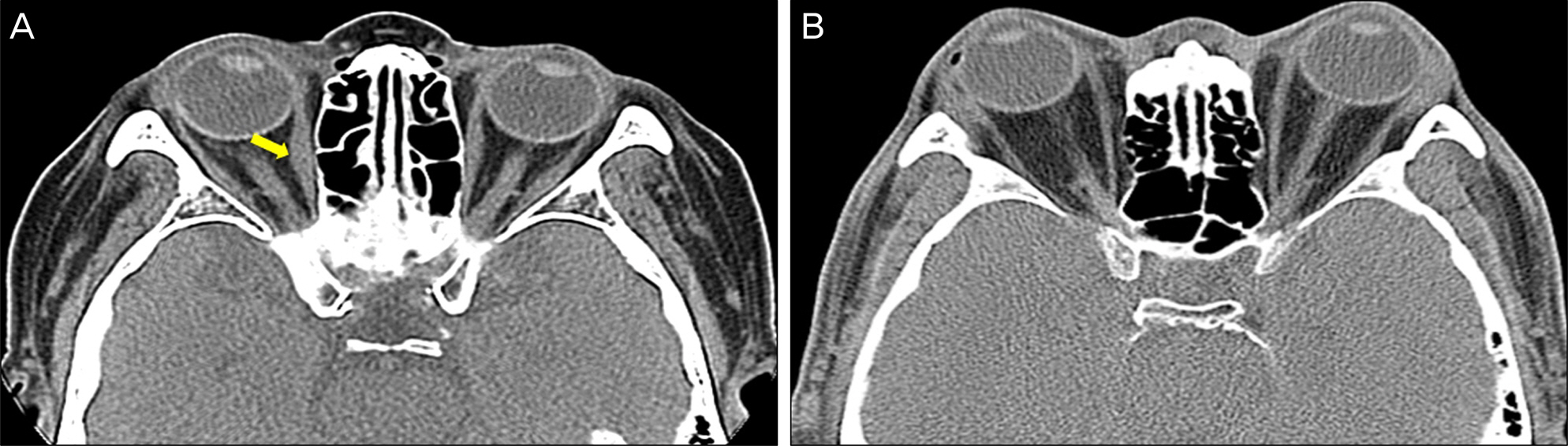
We performed a retrospective analysis using the medical records of patients who visited our clinic and were diagnosed with ocular MG and TAO, from January 2002 to December 2012. The diagnosis of Ocular MG was made on the basis of clinical symptoms and signs with laboratory evaluation, including assays for antithyroid and antiacetylcholine receptor (AchRAb) antibodies, and the Ice, neostigmine, and electromyography tests.
RESULTS
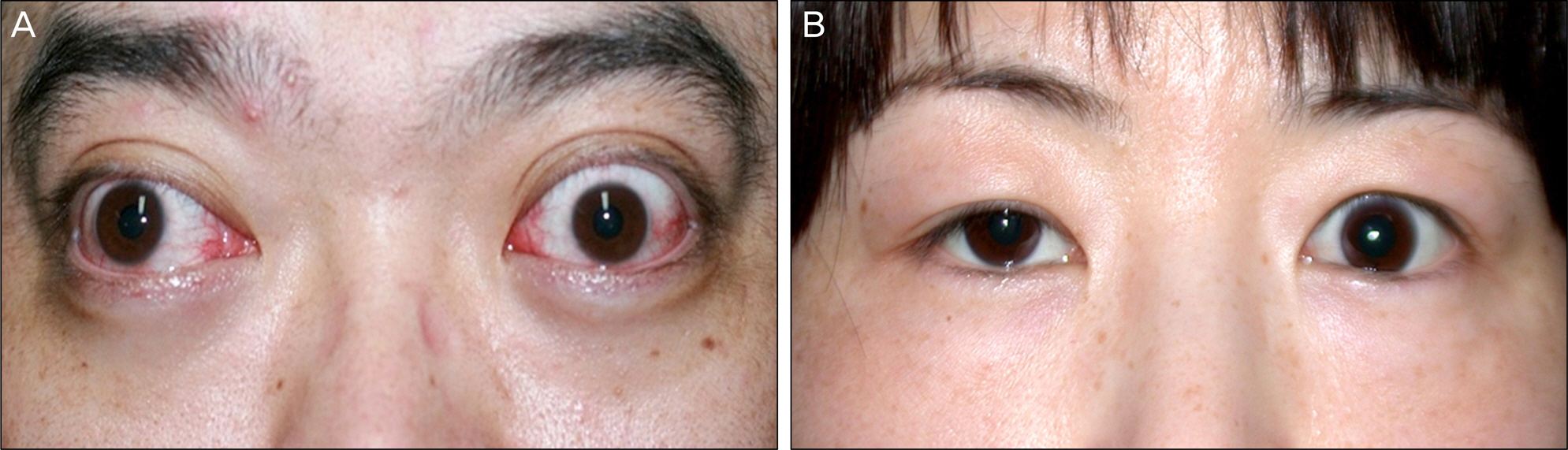
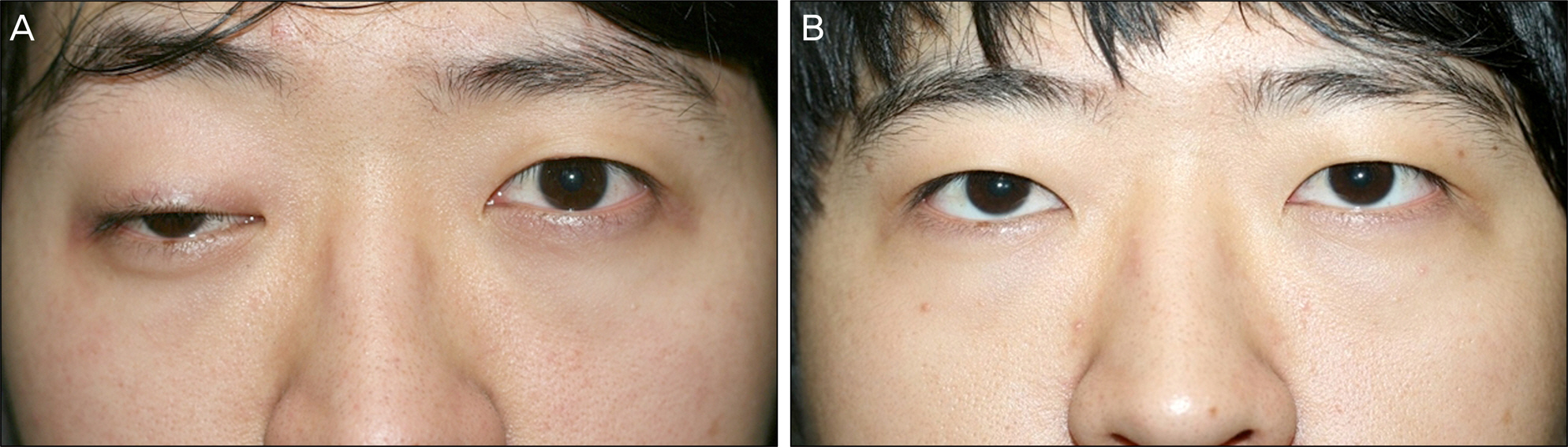
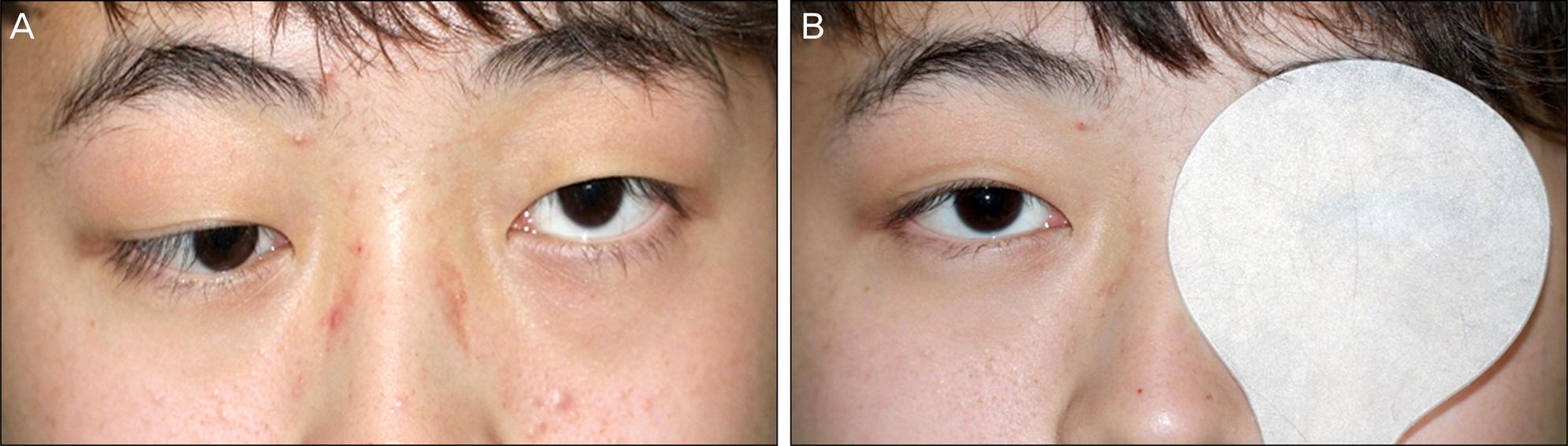
Of the 9 ocular MG patients with associated ophthalmopathy, 5 were male and 4 were female. The mean age was 36 +/- 16.0 years and the follow-up period was 45.6 +/- 36.6 months. Graves' disease (8 patients) was predominant and all patients showed abnormal thyroid function. Atypical symptoms and/or mild clinical features were predominant in ocular MG patients with TAO. Positive test results were obtained as follows: Neostigmine test 33.3%, electromyography 44.4%, ice test 77.8% and anti-AchR titer test 77.8%. Thyroid function test results were abnormal in all patients. In 3 patients who were first diagnosed with TAO, symptoms remained persistent despite steroid therapy then improved dramatically by administration of an anti-acetylcholinesterase agent. These patients were diagnosed with ocular MG in conjunction with TAO.
CONCLUSIONS
Patients with thyroid disease who show atypical features, symptomatic changes with fatigue, odd appearing ptosis, and who, do not exhibit good response to treatment of TAO need to be examined for ocular MG with additional tests and treatment.
MeSH Terms
Figure
Reference
-
References
1. Engel AG, Tsujihata M, Lindstrom JM, Lennon VA. The motor end plate in myasthenia gravis and in experimental autoimmune myasthenia gravis. A quantitative ultrastructural study. Ann N Y Acad Sci. 1976; 274:60–79.
Article2. Drachman DB, Angus CW, Adams RN, et al. Myasthenic antibodies cross-link acetylcholine receptors to accelerate degradation. N Engl J Med. 1978; 298:1116–22.
Article3. Thorlacius S, Aarli JA, Riise T, et al. Associated disorders in myasthenia gravis: autoimmune diseases and their relation to thymectomy. Acta Neurol Scand. 1989; 80:290–5.
Article4. Peacey SR, Belchetz PE. Graves' disease: associated ocular myasthenia gravis and a thymic cyst. J R Soc Med. 1993; 85:297–8.5. Raef H, Ladinsky M, Arem R. Concomitant euthyroid Graves' ophthalmopathy and isolated ocular myasthenia gravis. Postgrad Med J. 1990; 66:849–52.
Article6. Drachman DB. Myasthenia gravis. N Engl J Med. 1994; 330:1797–810.
Article7. Dolman PJ, Rootman J. VISA Classification for Graves orbitopathy. Ophthal Plast Reconstr Surg. 2006; 22:319–24.
Article8. Ohno M, Hamada N, Yamakawa J, et al. Myasthenia gravis associated with Graves' disease in Japan. Jpn J Med. 1987; 26:2–6.9. Ludgate M, Swillens S, Mercken L, Vassart G. Homology between thyroglobulin and acetylcholinesterase: an explanation for pathogenesis of Graves’ ophthalmopathy? Lancet. 1986; 2:219–20.
Article10. Mappouras DG, Philippou G, Haralambous S, et al. Antibodies to acetylcholinesterase cross-reacting with thyroglobulin in myasthenia gravis and Graves's disease. Clin Exp Immunol. 1995; 100:336–43.11. Maclean B, Wilson JA. See-saw relationship between hyper-thyroidism and myasthenia gravis. Lancet. 1954; 266:950–3.
Article12. COHEN B. Thyrotoxicosis by myasthenia gravis. S Afr Med J. 1946; 20:408–10.13. Kuroda Y, Endo C, Neshige R, Kakigi R. Exacerbation of myasthenia gravis shortly after administration of methimazole for hyperthyroidism. Jpn J Med. 1991; 30:578–81.14. Chen CS, Lee AW, Miller NR, Lee AG. Double vision in a patient with thyroid disease: what's the big deal? Surv Ophthalmol. 2007; 52:434–9.
Article15. Kusuhara T, Nakajima M, Imamura A. Ocular myasthenia gravis associated with euthyroid ophthalmopathy. Muscle Nerve. 2003; 28:764–6.
Article16. Daniel MA, Frederick AJ. Principle and practice of ophthalmology. 2nd ed.Vol. 5. Philadelphia: WB Sunders;2000. p. 4051–65.17. Weetman AP. Graves’ disease. N Engl J Med. 2000; 343:1236–48.
Article18. Marinó M, Ricciardi R, Pinchera A, et al. Mild clinical expression of myasthenia gravis associated with autoimmune thyroid diseases. J Clin Endocrinol Metabol. 1997; 82:438–43.19. Vincent A, Palace J, Hilton-Jones D. Myasthenia gravis. Lancet. 2001; 357:2122–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ocular Myasthenia Gravis in Conjunction with Thyroid-Associated Ophthalmopathy: A Case Report
- A case of Graves' disease associated with ocular myasthenia gravis
- The Clinical Characteristics of Hyperthyroidism Combined with Ocular Myasthenia Gravis: Report of Six cases
- A Case of Severe Ocular Myasthenia Gravis that Developed Total External Ophthalmoplegia
- Fecal Incontinence as a Symptom of Myasthenia Gravis