J Korean Ophthalmol Soc.
2013 Jan;54(1):143-148. 10.3341/jkos.2013.54.1.143.
Decorin and TGF-beta Expression after Partial Myotomy of the Extraocular Muscle in Rat
- Affiliations
-
- 1Department of Ophthalmology, Gyeongsang National University School of Medicine, Jinju, Korea. YJM@gnu.ac.kr
- 2Institute of Health Science, Gyeongsang National University School of Medicine, Jinju, Korea.
- KMID: 2216463
- DOI: http://doi.org/10.3341/jkos.2013.54.1.143
Abstract
- PURPOSE
To report the expression of decorin and TGF-beta in partial myotomy of the extraocular muscle in rats.
METHODS
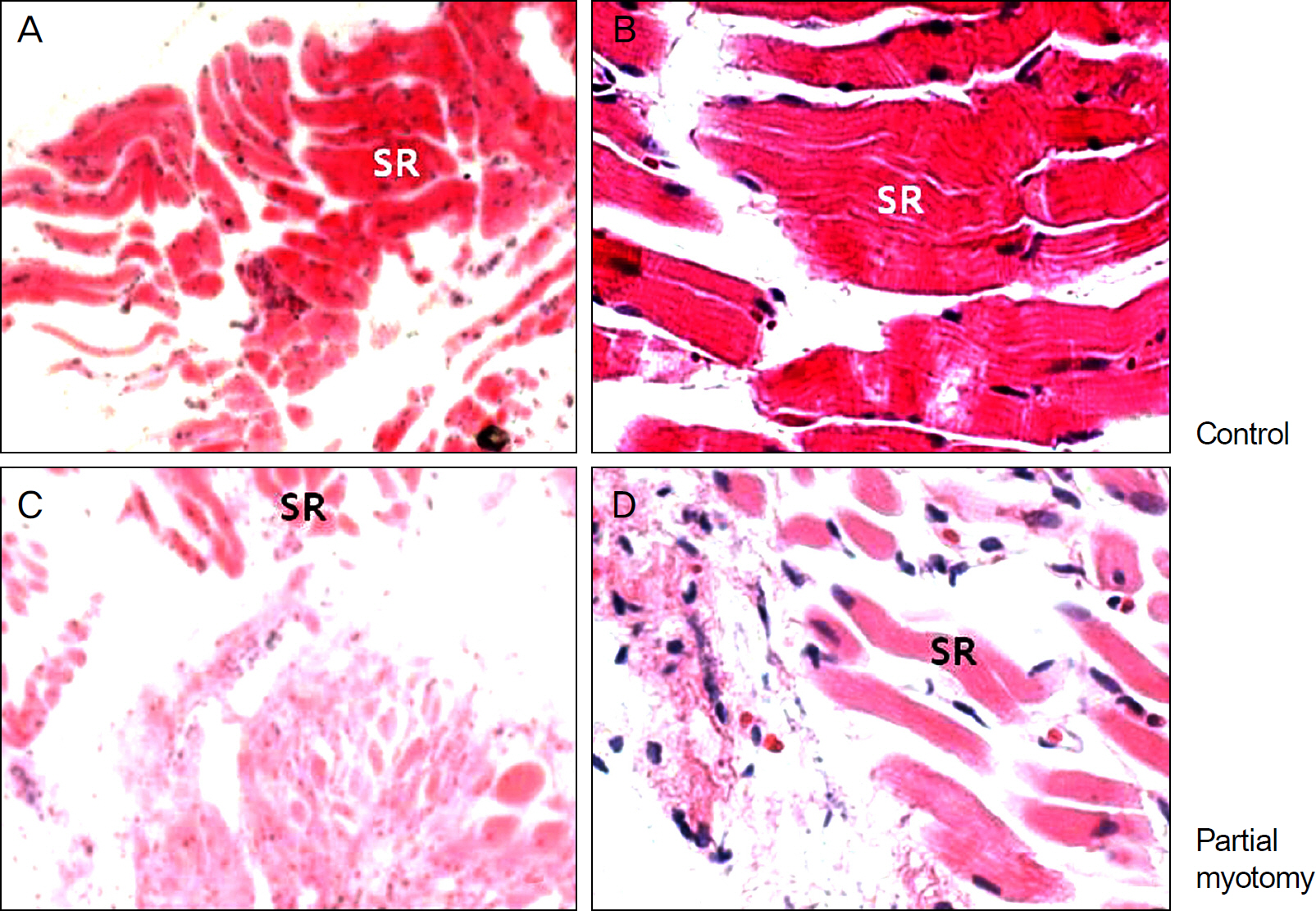
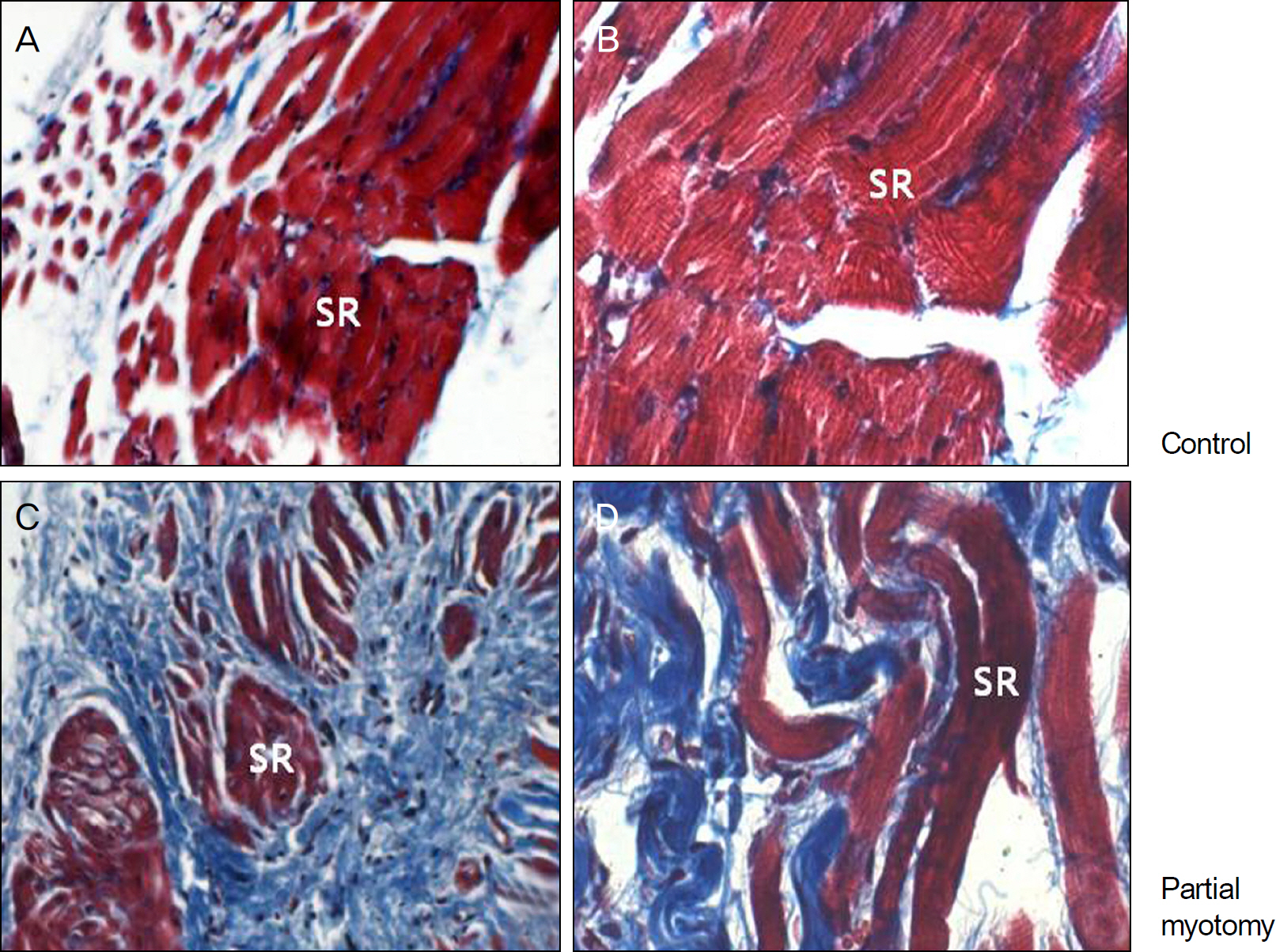
Partial myotomy of the superior rectus muscle was performed on the right eye of 10 Sprague-Dawley rats followed by exposure of the left superior rectus muscle and a simple suture of the conjunctiva. The bilateral superior rectus muscle was obtained from all rats at 2 weeks postoperatively. The tissues were observed under light microscopy with hematoxylin-eosin, Masson's trichrome staining and immunohistochemistry.
RESULTS
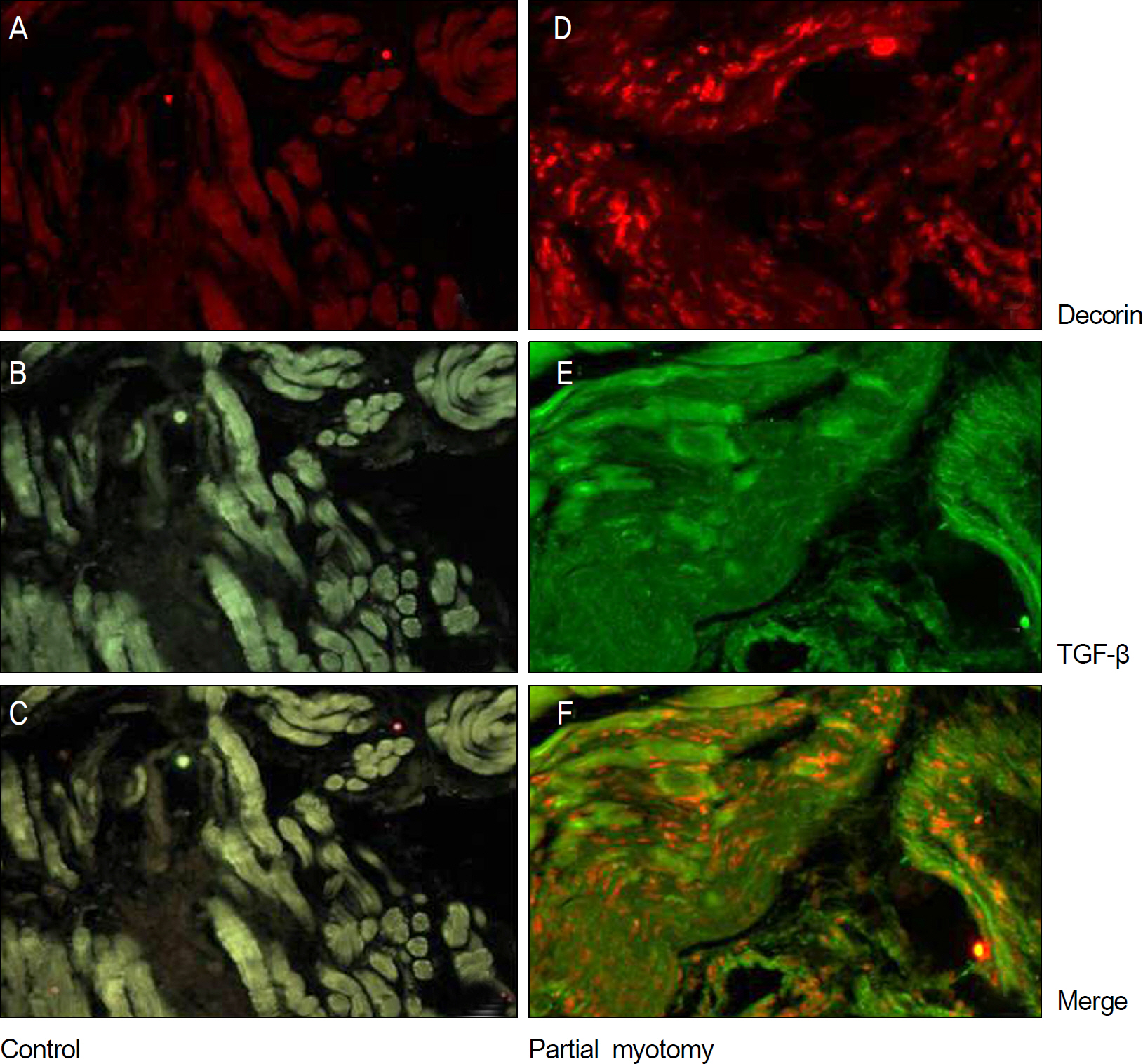
Histological examinations of the surgical area at 2 weeks after postoperatively showed irregularly concentrated fibrosis on light microscopy with hematoxylin-eosin and Masson's trichrome staining of the experimental eyes. Immnohistochemistry showed that expression of decorin was in the same location as TGF-beta in the experimental group.
CONCLUSIONS
The expression of decorin was found in the healing process after partial myotomy of the extraocular muscle in rats. Immunohistochemistry showed that expression of decorin was in the same location as with TGF-beta.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Metz HS. Restrictive factors in strabismus. Surv Ophthalmol. 1983; 28:71–83.
Article2. Dunlap EA. Surgery of muscle adhesions and effects of multiple operations. Br J Ophthalmol. 1974; 58:307–12.
Article3. Gomel V, Urman B, Gurgan T. Pathophysiology of adhesion abdominal and strategies for prevention. J Reprod Med. 1996; 41:35–41.4. Hwang JM, Chang BL. Use of Viscoat for delayed postoperative adjustable suture strabismus surgery in rabbits. Binocul Vis Strabismus Q. 1996; 11:137–42.5. Hwang JM, Chang BL. Delayed reattachment of extraocular abdominals in rabbits using thin polytetrafluoroethylene. Ophthalmic Surg Lasers. 1997; 28:59–64.6. Oh SO, Chang BL, Lee J. Effect of mitomycin C on delayed abdominal in experimental strabismus surgery. Korean J Ophthalmol. 1995; 9:51–8.7. Kim JH, Jeong SY, Jung MH, Hwang JM. Use of polyurethane with sustained release dexamethasone in delayed adjustable abdominal surgery. Br J Ophthalmol. 2004; 88:1450–4.8. Hwang JM, Chang BL. Combined effect of Interceed and 5-fluo-rouracil on delayed adjustable strabismus surgery. Br J Ophthalmol. 1999; 83:788–91.
Article9. Siriwardena D, Khaw PT, King AJ, et al. Human antitransforming growth factor beta(2) monoclonal antibody–a new modulator of wound healing in trabeculectomy:a randomized placebo controlled clinical study. Ophthalmolgy. 2002; 109:427–31.10. Border WA, Noble NA, Yamamoto T, et al. Natural inhibitor of transforming growth factor-beta protects against scarring in abdominal kidney disease. Nature. 1992; 360(6402):361–4.11. He F, Zhang Q, Kuruba R, et al. Upregulation of decorin by FXR in vascular smooth muscle cells. Biochem Biophys Res Commun. 2008; 372:746–51.
Article12. Zanotti S, Negri T, Cappelletti C, et al. Decorin and biglycan abdominal is defferentially altered in several muscular dystrophies. Brain. 2005; 128(Pt 11):2546–55.13. Hocking AM, Shinomura T, McQuillan DJ. Leucine-rich repeat glycoproteins of the extracellular matrix. Matrix Biol. 1998; 17:1–19.
Article14. Thieszen SL, Rosenquist TH. Expression of collagens and decorin during aortic arch artery development: implications for matrix abdominal formation. Matrix Biol. 1995; 14:573–82.15. Merle B, Malaval L, Lawler J, et al. Decorin inhibits cell attachment to thrombospondin-1 by binding to a KKTR-dependent cell adhesive site present within the N-terminal domain of thrombo-spondin-1. J Cell Biochem. 1997; 67:75–83.
Article16. Merle B, Durussel L, Delmas PD, Clézardin P. Decorin inhibits cell migration through a process requiring its glycosaminoglycan side chain. J Cell Biochem. 1999; 75:538–46.
Article17. De Luca A, Santra M, Baldi A, et al. Decorin-induced growth abdominal is associated with abdominal of p21, an inhibitor of cy-clin-dependent kinases. J Biol Chem. 1996; 271:18961–5.18. Fischer JW, Kinsella MG, Levkau B, et al. Retroviral abdominal of decorin differentially affects the response of arterial smooth muscle cells to growth factors. Arterioscler Thromb Vasc Biol. 2001; 21:777–84.19. Hildebrand A, Romarís M, Rasmussen LM, et al. Interaction of the small interstitial proteoglycans biglycan, decorin and fi-bromodulin with transforming growth factor beta. Biochem J. 1994; 302(Pt 2):527–34.20. Kaname S, Ruoslahti E. Betaglycan has multiple binding sites for transforming growth factor-beta 1. Biochem J. 1996; 315(Pt 3):815–20.21. Honardoust D, Varkey M, Hori K, et al. Small leucine-rich abdominal, decorin and fibromodulin, are reduced in postburn hypertrophic scar. Wound Repair Regen. 2011; 19:368–78.22. Reich-Schupke S, Mumme A, Altmeyer P, Stuecker M. Decorin expression with stump recurrence and neovascularization after varicose vein surgery–a pilot study. Dermatol Surg. 2011; 37:480–5.
Article23. Grefte S, Kuijpers-Jagtman AM, Torensma R, Von den Hoff JW. Model for muscle regeneration around fibrotic lesions in recurrent strain injuries. Med Sci Sports Exerc. 2010; 42:813–9.
Article24. Aärimaa V, Kääriäinen M, Vaittinen S, et al. Restroration of my-ofiber continuity after transection injury in the rat soleus. Neuromuscul Disord. 2004; 14:421–8.25. Woo KJ, Lee KS, Choi DG, Choi MY. The effect of subabdominal injection of bevacizumab after resection of muscle in abdominal models. J Korean Ophthalmol Soc. 2010; 51:423–9.26. Border WA, Noble NA, Yamamoto T, et al. Natural inhibitor of transforming growth factor-beta protects against scarring in abdominal kidney disease. Nature. 1992; 360:361–4.27. Mohan RR, Tovey JC, Gupta R, et al. Decorin biology, expression, function and therapy in the cornea. Curr Mol Med. 2011; 11:110–28.28. Isaka Y, Brees DK, Ikegaya K, et al. Gene therapy by skeletal abdominal expression of decorin prevents fibrotic disease in rat kidney. Nat Med. 1996; 2:418–23.29. Giri SN, Hyde DM, Braun RK, et al. Antifibrotic effect of decorin in a bleomycin hamster model of lung fibrosis. Biochem Pharmacol. 1997; 54:1205–16.
Article30. Fukushima K, Badlani N, Usas A, et al. The use of an antifibrosis agent to improve muscle recovery after laceration. Am J Sports Med. 2001; 29:394–402.
Article31. Grisanti S, Szurman P, Warga M, et al. Decorin modulates wound healing in experimental glaucoma filtration surgery: a pilot study. Invest Ophthalmol Vis Sci. 2005; 46:191–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of decorin, TGF-beta antagonist on wound healing of rats
- The effect of decorinas an antagonist of tgf-betain fetal rat wound healing
- The effect of Decorin, TGF-beta antagonist, on wound healing in rabbits
- Effect of decorin on tensile strength of healing flexor tendon
- Effect of Transforming Growth Factor-Induced Gene Product, beta ig-h3 on Proliferation, Migration, and Adhesion of Aortic Smooth Muscle Cells Cultured in High Glucose