J Korean Ophthalmol Soc.
2015 Feb;56(2):199-204. 10.3341/jkos.2015.56.2.199.
Clinical Analysis of the 0.3% Tosufloxacin Ophthalmic Solution Effect on Conjunctival Normal Flora
- Affiliations
-
- 1Department of Ophthalmology, Kyungpook National University School of Medicine, Daegu, Korea. okeye@hanmail.net
- KMID: 2216002
- DOI: http://doi.org/10.3341/jkos.2015.56.2.199
Abstract
- PURPOSE
To report the outcomes of clinical analysis on the negative culture rate of normal ocular surface flora and the anterior chamber penetration after the preoperative prophylactic use of 0.3% tosufloxacin ophthalmic solution.
METHODS
From July 2010 to June 2012, 38 eyes of 38 patients who were scheduled to receive intravitreal injection or cataract surgery were examined for bacterial culture positive rate using conjunctival scraping. The patients were treated with 0.3% tosufloxacin eyedrops preoperatively 5 times a day for 2 days before surgery. After the treatment, the bacterial culture negative rate based on conjunctival scraping was assessed to evaluate the drug efficacy. Of the 38 patients, 19 had cataract surgery. The concentration of tosufloxacin at anterior chamber was assessed in the 19 patients. Additionally, any side effects from the drug were monitored during the treatment.
RESULTS
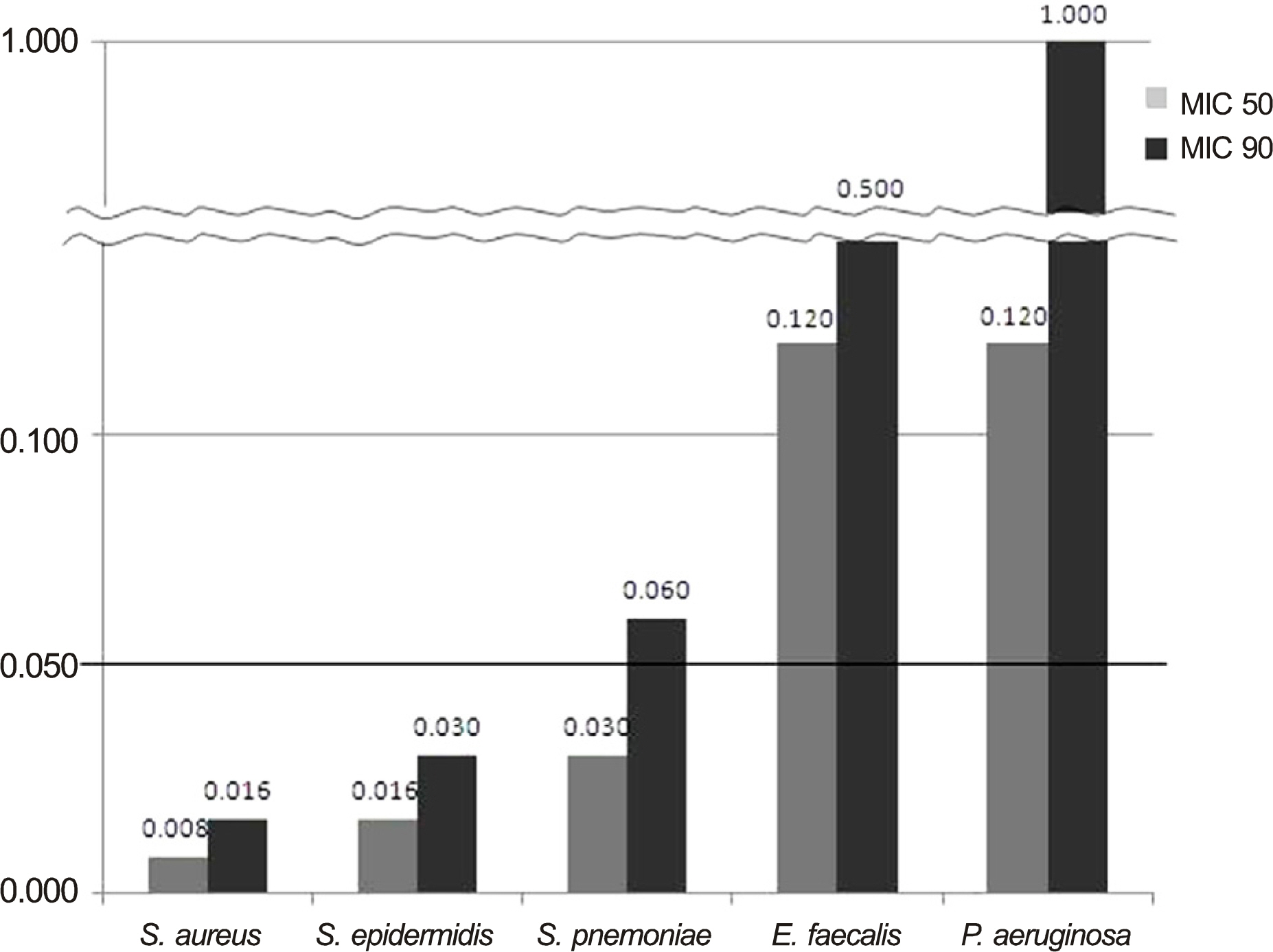
Among the 38 eyes, 21 eyes showed a bacterial culture positive rate before treatment. After the drug treatment, the bacterial culture negative rate was 57.1% (12/21). Coagulase-negative staphylococci were most frequently cultured in 15 (39%) of the 38 eyes before treatment and the negative rate of bacterial culture was 86.7% (13/15) after treatment. Average antibiotic residue concentrations in aqueous humor was 0.050 +/- 0.038 microg/mL. No side effects from the drug were reported during the experimental period.
CONCLUSIONS
Although the 0.3% tosufloxacin eyedrops were not effective in all bacterial strains and showed relatively low penetration rate into the anterior chamber, they were effective in some gram positive organisms, particularly in coagulase-negative staphylococci of normal ocular surface flora.
MeSH Terms
Figure
Reference
-
References
1. Kattan HM, Flynn HW Jr, Pflugfelder SC. . Nosocomial en-dophthalmitis survey. Current incidence of infection after intra-ocular surgery. Ophthalmology. 1991; 98:227–38.2. Erie JC, Raecker MA, Baratz KH. . Risk of retinal detachment after cataract extraction, 1980-2004: a population-based study. Ophthalmology. 2006; 113:2026–32.3. Caldwell DR, Kastl PR, Cook J, Simon J. Povidone-iodine: its efficacy as a preoperative conjunctival and periocular preparation. Ann Ophthalmol. 1984; 16:577–80.4. Peyman GA, Sathar ML, May DR. Intraocular gentamicin as intra-operative prophylaxis in South India eye camps. Br J Ophthalmol. 1977; 61:260–2.
Article5. Garat M, Moser CL, Martín-Baranera M. . Prophylactic intra-cameral cefazolin after cataract surgery: endophthalmitis risk reduction and safety results in a 6-year study. J Cataract Refract Surg. 2009; 35:637–42.6. Barkana Y, Almer Z, Segal O. . Reduction of conjunctival bacterial flora by povidone-iodine, ofloxacin and chlorhexidine in an outpatient setting. Acta Ophthalmol Scand. 2005; 83:360–3.
Article7. Seal DV, Barry P, Gettinby G. . ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: Case for a European multicenter study. J Cataract Refract Surg. 2006; 32:396–406.8. De Kaspar HM, Chang RT, Shriver EM. . Three-day application of topical ofloxacin reduces the contamination rate of micro-surgical knives in cataract surgery: a prospective randomized study. Ophthalmology. 2004; 111:1352–5.9. Kim MJ, Lee JH, Yoon YR, Kim HK. A randomized, prospective clinical comparison of the efficacy and safety of topical fluo-roquinolone antibiotics in ophthalmologic microsurgery. J Korean Ophthalmol Soc. 2011; 52:1440–7.
Article10. Yamada M, Yoshida J, Hatou S. . Mutations in the quinolone resistance determining region in Staphylococcus epidermidis recovered from conjunctiva and their association with susceptibility to various fluoroquinolones. Br J Ophthalmol. 2008; 92:848–51.
Article11. Taban M, Behrens A, Newcomb RL. . Acute endophthalmitis following cataract surgery: a systematic review of the literature. Arch Ophthalmol. 2005; 123:613–20.12. Speaker MG, Milch FA, Shah MK. . Role of external bacterial flora in the pathogenesis of acute postoperative endophthalmitis. Ophthalmology. 1991; 98:639–49. discussion 650.
Article13. Barry P, Seal DV, Gettinby G. . ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: Preliminary report of principal results from a European multicenter study. J Cataract Refract Surg. 2006; 32:407–10.14. Snyder-Perlmutter LS, Katz HR, Melia M. Effect of topical cipro-floxacin 0.3% and ofloxacin 0.3% on the reduction of bacterial flora on the human conjunctiva. J Cataract Refract Surg. 2000; 26:1620–5.
Article15. Han DP, Wisniewski SR, Wilson LA. . Spectrum and suscepti-bilities of microbiologic isolates in the Endophthalmitis Vitrectomy Study. Am J Ophthalmol. 1996; 122:1–17.
Article16. Barry AL, Fuchs PC. In vitro activities of sparfloxacin, tosufloxacin, ciprofloxacin, and fleroxacin. Antimicrob Agents Chemother. 1991; 35:955–60.
Article17. Levine JM, Noecker RJ, Lane LC. . Comparative penetration of moxifloxacin and gatifloxacin in rabbit aqueous humor after topical dosing. J Cataract Refract Surg. 2004; 30:2177–82.
Article18. Chung SE, Ham DI. Visual prognosis of culture-proven bacterial endophthalmitis. J Korean Ophthalmol Soc. 2006; 47:1292–7.19. Kowalski RP, Yates KA, Romanowski EG. . An ophthalmologist's guide to understanding antibiotic susceptibility and minimum in-hibitory concentration data. Ophthalmology. 2005; 112:1987.
Article20. Hori Y, Nakazawa T, Maeda N. . Susceptibility comparisons of normal preoperative conjunctival bacteria to fluoroquinolones. J Cataract Refract Surg. 2009; 35:475–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Normal Bacterial Flora in the Conjuntival Sac of Normal and Anophthalmic Eyes
- Olopatadine ophthalmic solution suppresses substance P release in the conjunctivitis models
- Comparative Studies of Timolol and Pilocarpine in Normal Volunteers
- Bacteriologic Study on Normal Conjunctival Flora and Change of Antibiotic Susceptability
- Bacterial Conjuntival Flora in Dry Eye Patients