J Korean Ophthalmol Soc.
2012 Aug;53(8):1157-1162. 10.3341/jkos.2012.53.8.1157.
Scleral Window Surgery with Mitomycin C for Nanophthalmic Uveal Effusion: Case Report
- Affiliations
-
- 1Department of Ophthalmology, Gyeongsang National University School of Medicine, Jinju, Korea. parkjm@gnu.ac.kr
- 2Gyeongsang Institute of Health Science, Gyeongsang National University, Jinju, Korea.
- KMID: 2215960
- DOI: http://doi.org/10.3341/jkos.2012.53.8.1157
Abstract
- PURPOSE
To report the case of a 36-year-old patient with nanophthalmic uveal effusion was treated with scleral window surgery and topical administration of mitomycin C (MMC).
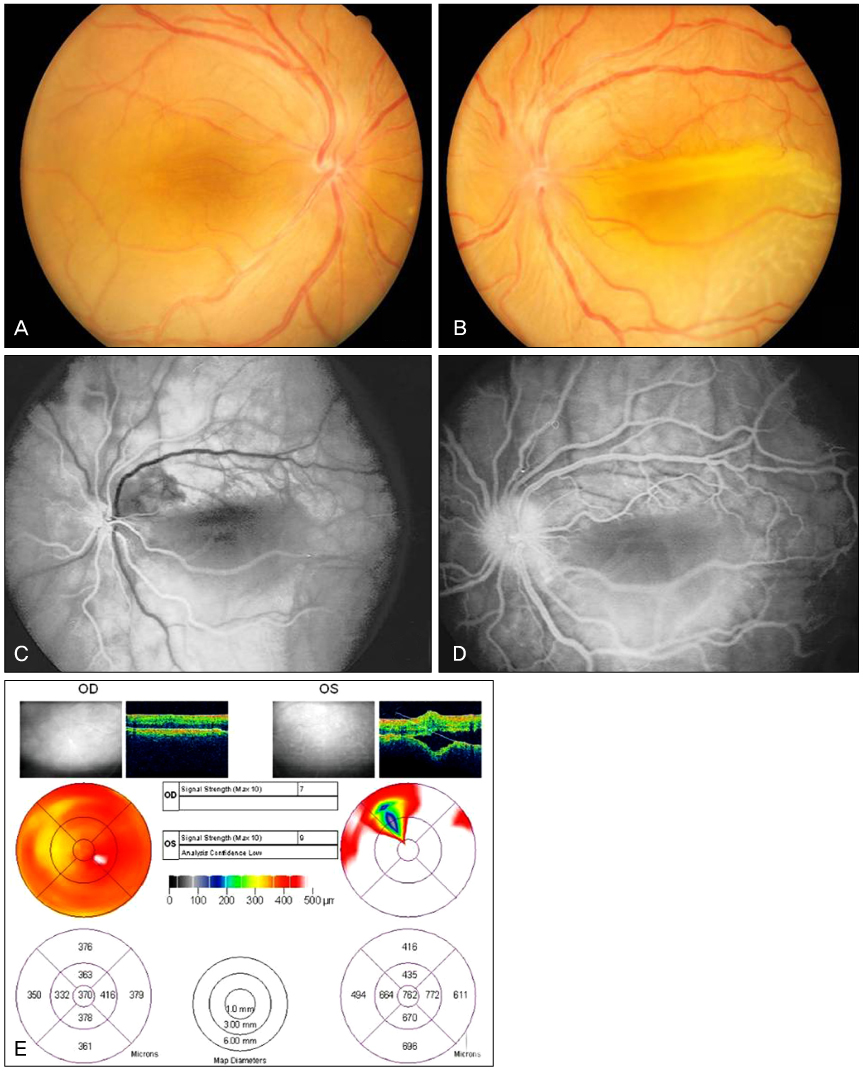
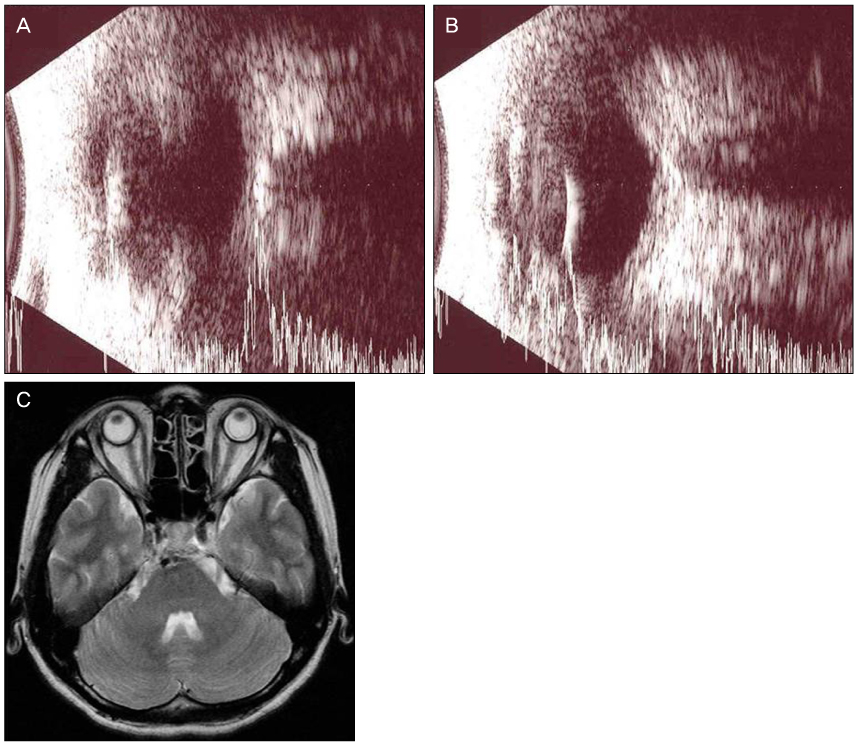
CASE SUMMARY
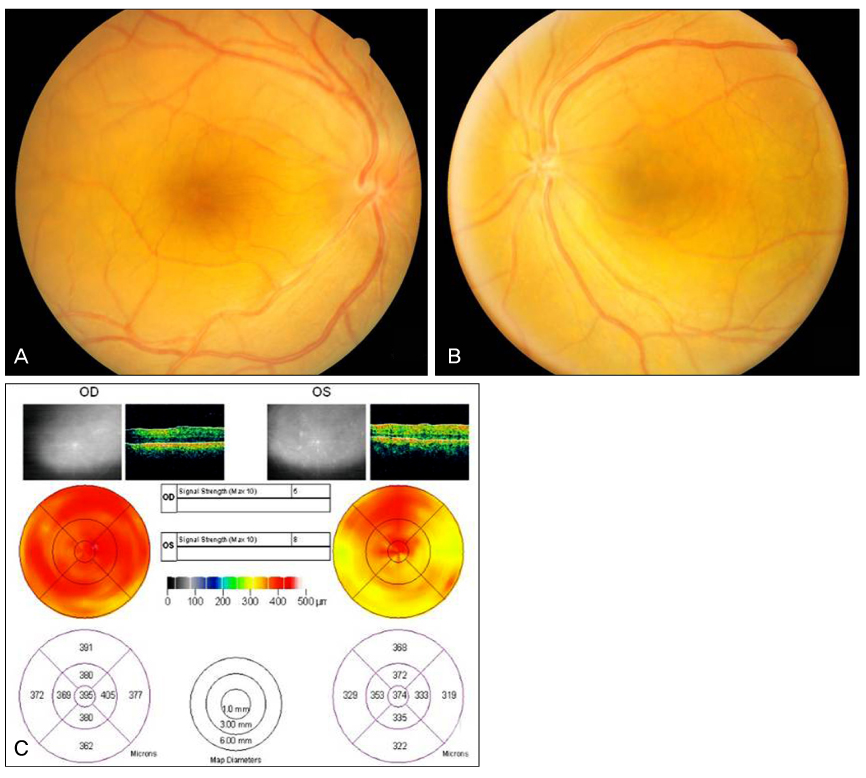
A 36-year-old woman presented with decreased visual acuity and blurred vision in the both eyes during 3 months. Fundus examination revealed choroidal effusion and retinal detachment with thickend sclera wall and short axial lengh. Partial-thickness sclera flap with deep sclerostomy was performed and topical MMC was administered to one quadrant of the equatorial sclera. The subretinal fluid resorbed gradually and visual acuity improved.
CONCLUSIONS
Scleral window surgery and topical mitomycin C might relieve the blocked transscleral outflow of intraocular fluid in the small area of a sclerostomy in young patient with nanophthlamos.
MeSH Terms
Figure
Reference
-
1. Singh OS, Sofinski SJ. Duke-Elder S, editor. Anomalies in the size of the eye. System of Ophthalmology. 1963. Vol 3. St. Louis: CV Mosby;488–495.2. Serrano JC, Hodgkins PR, Taylor DS, et al. The nanophthalmic macula. Br J Ophthalmol. 1998. 82:276–279.3. Cross HE, Yoder F. Familial nanophthalmos. Am J Ophthalmol. 1976. 81:300–306.4. Hirsch SE, Waltman SR, LaPiana FG. Bilateral nanophthalmos. Arch Ophthalmol. 1973. 89:353.5. Vingolo EM, Steindl K, Forte R, et al. Autosomal dominant simple microphthalmos. J Med Genet. 1994. 31:721–725.6. Singh OS, Simmons RJ, Brockhurst RJ, Trempe CL. Nanophthalmos: a perspective on identification and therapy. Ophthalmology. 1982. 89:1006–1012.7. Kimbrough RL, Trempe CS, Brockhurst RJ, Simmons RJ. Angle-closure glaucoma in nanophthalmos. Am J Ophthalmol. 1979. 88(3 Pt 2):572–579.8. Brockhurst RJ. Nanophthalmos with uveal effusion. A new clinical entity. Arch Ophthalmol. 1975. 93:1989–1999.9. Yue BY, Duvall J, Goldberg MF, et al. Nanophthalmic sclera. Morphologic and tissue culture studies. Ophthalmology. 1986. 93:534–541.10. Brockhurst RJ. Vortex vein decompression for nanophthalmic uveal effusion. Arch Ophthalmol. 1980. 98:1987–1990.11. Song SW, Kwak NH, Huh W. A case of nanophthalmos. J Korean Ophthalmol Soc. 1996. 37:692–696.12. Lee JH, Choi JY, Kim SS. Two cases of uveal effusion syndrome. Korean J Ophthalmol. 2006. 20:124–127.13. Sabrosa NA, Smith HB, MacLaren RE. Scleral punch method with topical mitomycin C for safe revision of failed deep sclerectomy in nanophthalmic uveal effusion syndrome. Graefes Arch Clin Exp Ophthalmol. 2009. 247:999–1001.14. Warburg M. Microphthalmos and colobomata among mentally retarded individuals. Acta Ophthalmol (Copenh). 1981. 59:665–673.15. Khairallah M, Messaoud R, Zaouali S, et al. Posterior segment changes associated with posterior microphthalmos. Ophthalmology. 2002. 109:569–574.16. Auffarth GU, Blum M, Faller U, et al. Relative anterior microphthalmos: morphometric analysis and its implications for cataract surgery. Ophthalmology. 2000. 107:1555–1560.17. Burgoyne C, Tello C, Katz LJ. Nanophthalmia and chronic angle-closure glaucoma. J Glaucoma. 2002. 11:525–528.18. Calhoun FP Jr. The management of glaucoma in nanophthalmos. Trans Am Ophthalmol Soc. 1975. 73:97–122.19. Neelakantan A, Venkataramakrishnan P, Rao BS, et al. Familial nanophthalmos: management and complications. Indian J Ophthalmol. 1994. 42:139–143.20. Johnson MW, Gass JD. Surgical management of the idiopathic uveal effusion syndrome. Ophthalmology. 1990. 97:778–785.21. Morita H, Funata M, Kusakari T, et al. Recurrence of nanophthalmic uveal effusion. Ophthalmologica. 1993. 207:30–36.22. Suzuki Y, Nishina S, Azuma N. Scleral window surgery and topical mitomycin C for nanophthalmic uveal effusion complicated by renal failure: case report. Graefes Arch Clin Exp Ophthalmol. 2007. 245:755–757.23. Akduman L, Adelberg DA, Del Priore LV. Nanophthalmic uveal effusion managed with scleral windows and topical mitomycin-C. Ophthalmic Surg Lasers. 1997. 28:325–327.