J Korean Ophthalmol Soc.
2011 Aug;52(8):979-983. 10.3341/jkos.2011.52.8.979.
A Case of Chronic Dacryocystitis Caused by Achromobacter Xylosoxidans
- Affiliations
-
- 1Department of Ophthalmology, Gyeongsang National University School of Medicine, Jinju, Korea. stramast@naver.com
- 2Institute of Health Science, Gyeongsang National University, Jinju, Korea.
- KMID: 2214777
- DOI: http://doi.org/10.3341/jkos.2011.52.8.979
Abstract
- PURPOSE
To report a case of chronic dacryocystitis caused by Achromobacter xylosoxidans.
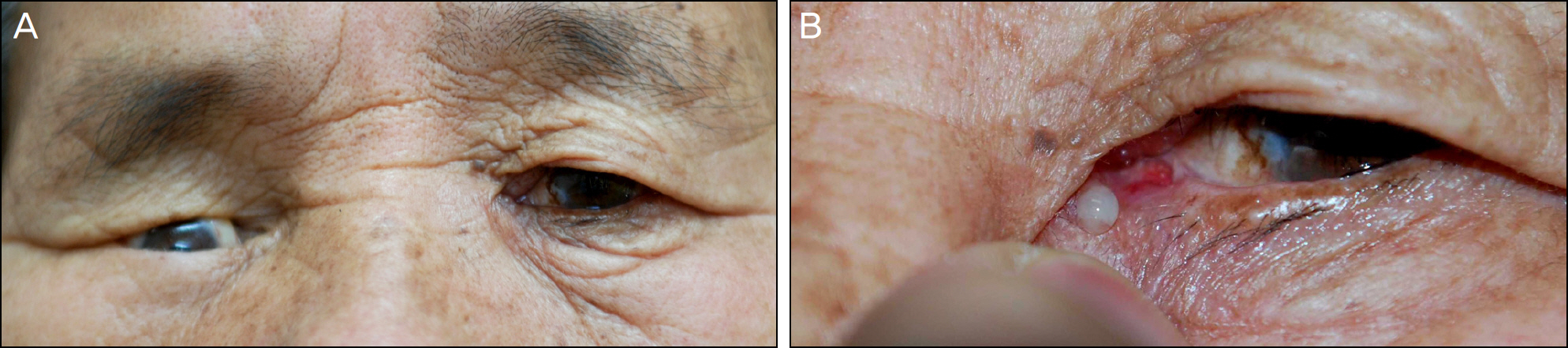
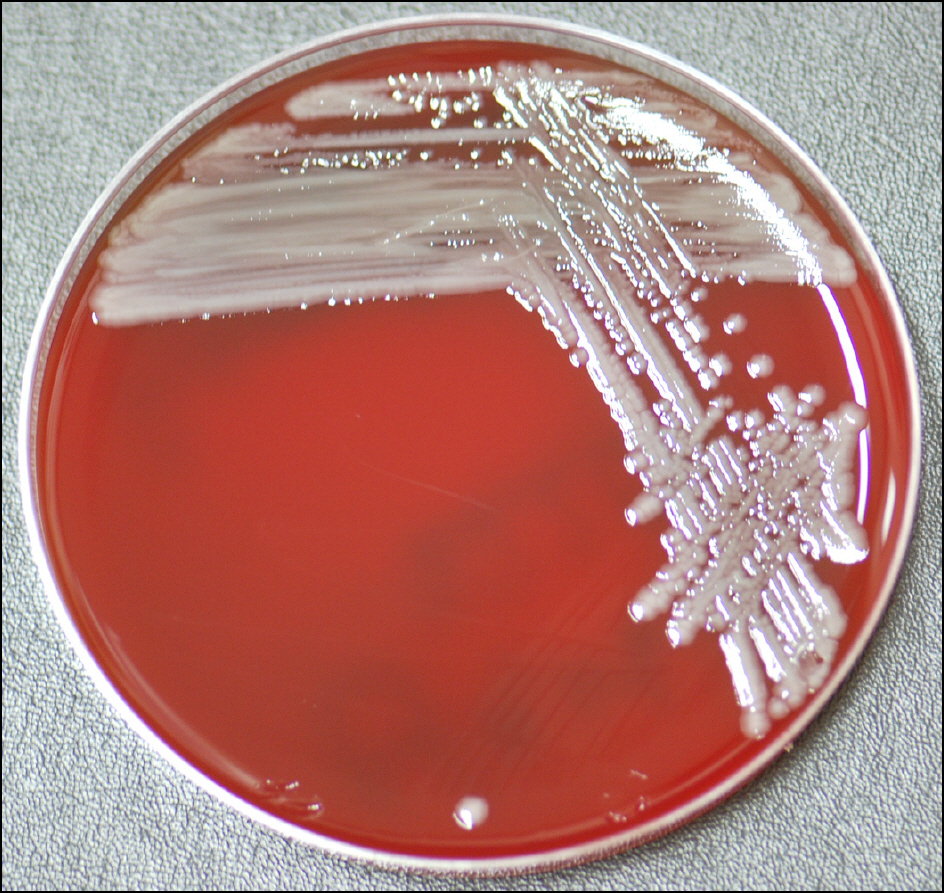
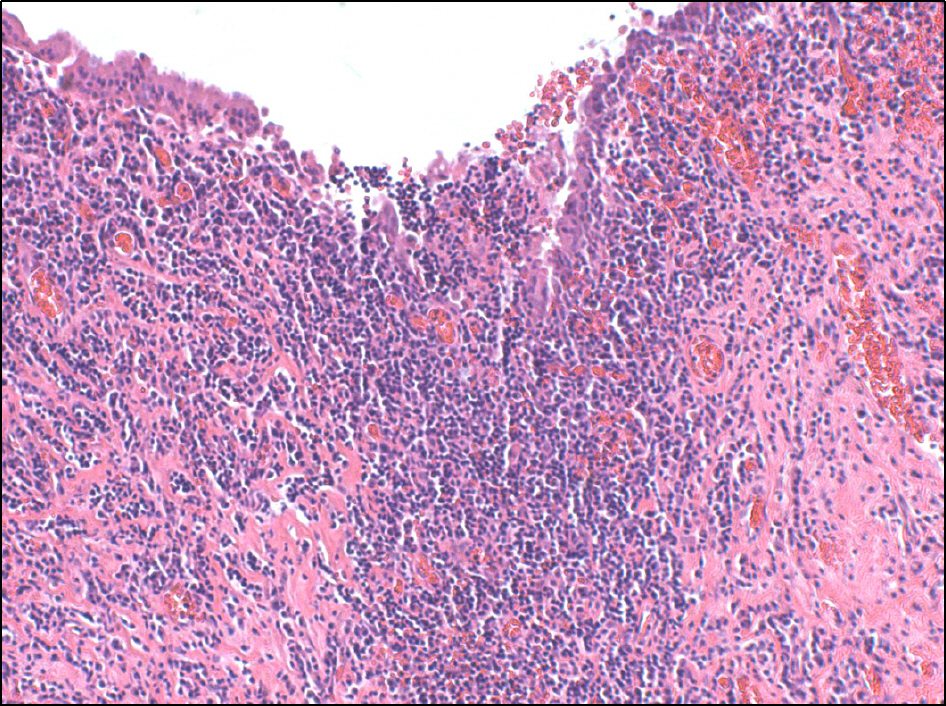
CASE SUMMARY
A 73-year-old female was referred to our clinic for management of chronic dacryosyctitis from which she did not to recover despite empirical therapy. A. xylosoxidans was isolated from purulent discharge. Based on the results of susceptibility testing, therapy was changed to fortified ceftazidime eye-drop 6 times a day and intravenous tazocin 4.5 g/20 ml (piperacillin 2 g/tazobactam 0.25 g) 3 times a day. All symptoms were resolved after treatment with sensitive antibiotics and external dacryocystorhinostomy.
CONCLUSIONS
To our knowledge, this is the first report of A. xylosoxidans dacryocystitis. A. xylosoxidans are rare but potential pathogens which cause dacryocystitis. The cultures and sensitivity test were collected and processed to detect the presence of unusual pathogens in a case with persistent infection despite conventional treatment.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Huber-Spitzy V, Steinkogler FJ, Huber E, et al. Acquired dacryocystitis: microbiology and conservative therapy. Acta Ophthalmol (Copenh). 1992; 70:745–9.
Article2. Blicker JA, Buffam FV. Lacrimal sac, conjunctival, and nasal culture results in dacryocystorhinostomy patients. Ophthal Plast Reconstr Surg. 1993; 9:43–6.
Article3. Coden DJ, Hornblass A, Haas BD. Clinical bacteriology of dacryocystitis in adults. Ophthal Plast Reconstr Surg. 1993; 9:125–31.
Article4. Brook I, Frazier EH. Aerobic and anaerobic microbiology of dacryocystitis. Am J Ophthalmol. 1998; 125:552–4.
Article5. Hartikainen J, Lehtonen OP, Saari KM. Bacteriology of lacrimal duct obstruction in adults. Br J Ophthalmol. 1997; 81:37–40.
Article6. DeAngelis D, Hurwitz J, Mazzulli T. The role of bacteriologic infection in the etiology of nasolacrimal duct obstruction. Can J Ophthalmol. 2001; 36:134–9.
Article7. Chaudhry IA, Shamsi FA, Al-Rashed W. Bacteriology of chronic dacryocystitis in a tertiary eye care center. Ophthal Plast Reconstr Surg. 2005; 21:207–10.
Article8. Briscoe D, Rubowitz A, Assia E. Changing bacterial isolates and antibiotic sensitivities of purulent dacryocystitis. Orbit. 2005; 24:95–8.
Article9. Sun X, Liang Q, Luo S, et al. Microbiological analysis of chronic dacryocystitis. Ophthalmic Physiol Opt. 2005; 25:261–3.
Article10. Purgason PA, Hornblass A, Loeffler M. Atypical presentation of fungal dacryocystitis. A report of two cases. Ophthalmology. 1992; 99:1430–2.11. Pastor-Pascual F, España-Gregori E, Aviñó-Martínez J, Gallego- Pinazo R. Dacryocystitis caused by Candida lusitaniae. Arch Soc Esp Oftalmol. 2007; 82:365–7.12. Kubo M, Sakuraba T, Arai Y, Nakazawa M. aberrations for dacryocystitis caused by aberrations Staphylococcus aureus: report of four cases. Jpn J Ophthalmol. 2002; 46:177–82.13. Kotlus BS, Rodgers IR, Udell IJ. Dacryocystitis caused by com-munity-onset methicillin-resistant Staphylococcus aureus. Ophthal Plast Reconstr Surg. 2005; 21:371–5.
Article14. Mills DM, Bodman MG, Meyer DR, Morton AD 3rd. ASOPRS Dacryocystitis Study Group. The microbiologic spectrum of dacryocystitis: a national study of acute versus chronic infection. Ophthal Plast Reconstr Surg. 2007; 23:302–6.
Article15. Ma YR, Jong SK. The study of chronic dacryocystitis: aberrations of pathogenic organism and histopathological findings. J Korean Ophthalmol Soc. 1999; 40:652–6.16. Krzewinski JW, Nguyen CD, Foster JM, Burns JL. Use of random amplified polymorphic DNA PCR to examine epidemiology of Stenotrophomonas maltophilia and Achromobacter (Alcaligenes) xylosoxidans from patients with cystic fibrosis. J Clin Microbiol. 2001; 39:3597–602.17. Igra-Siegman Y, Chmel H, Cobbs C. Clinical and laboratory characteristics of Achromobacter xylosoxidans infection. J Clin Microbiol. 1980; 11:141–5.
Article18. Holmes B, Snell JJ, Lapage SP. Strains of Achromobacter xylosoxidans from clinical material. Strains of Achromobacter xylosoxidans from clinical material. J Clin Pathol. 1977; 30:595–601.19. Yabuuchi E, Oyama A. Achromobacter xylosoxidans n. sp. from human ear discharge. Jpn J Microbiol. 1971; 15:471–81.20. Shigeta S, Higa K, Ikeda M, Endo S. A purulent meningitis caused by Achromobacter xylosoxidans. Igaku No Ayumi. 1974; 88:336–7.21. Reddy AK, Garg P, Shah V, Gopinathan U. Clinical, microbiological profile and treatment outcome of ocular infections caused by Achromobacter xylosoxidans. Cornea. 2009; 28:1100–3.
Article22. Mandell WF, Garvey GJ, Neu HC. Achromobacter xylosoxidans bacteremia. Rev Infect Dis. 1987; 5:1001–5.
Article23. Spear JB, Fuhrer J, Kirby BD. Achromobacter xylosoxidans (Alcaligenes xylosoxidans subsp. xylosoxidans) bacteremia associated with a well-water source: case report and review of the literature. J Clin Microbiol. 1988; 26:589–9.
Article24. Newman PE, Hider P, Waring GO 3rd, et al. Corneal ulcer due to Achromobacter xylosoxidans. Br J Ophthalmol. 1984; 68:472–4.
Article25. Fiscella R, Noth J. Achromobacter xylosoxidans corneal ulcer in a therapeutic soft contact lens wearer. Cornea. 1989; 8:267–9.
Article26. Uy HS, Matias R, de la Cruz F, Natividad F. Achromobacter xylosoxidans endophthalmitis diagnosed by polymerase chain reaction and gene sequencing. Ocul Immunol Inflamm. 2005; 13:463–7.27. Oh J-Y, Shin YJ, Wee WR. A case of epidemic keratoconjunctivitis complicated by alcaligenes xylosoxidans infection. Korean J Ophthalmol. 2005; 19:233–4.
Article28. Srinivasan S, McAllum P, Poutanen SM, Slomovic AR. Bilateral simultaneous Achromobacter xylosoxidans keratitis following penetrating keratoplasty. J Cataract Refract Surg. 2006; 32:2149–52.
Article29. Weissgold DJ, Kirkpatrick B, Iverson M. Acute postoperative Alcaligenes xylosoxidans endophthalmitis. Retina. 2003; 23:578–80.
Article30. Linke SJ, Skevas C, Richard G, Katz T. Bilateral Achromobacter xylosoxidans keratitis after laser in situ keratomileusis. J Cataract Refract Surg. 2010; 36:1045–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of scalp abscess caused by Achromobacter xylosoxidans after vacuum delivery
- A Case of Peritonitis Due to Achromobacter xylosoxidans subsp. xylosoxidans in a Patient Undergoing Continuous Ambulatory Peritoneal Dialysis (CAPD)
- Continuous Ambulatory Peritoneal Dialysis-Associated Peritonitis Caused by Achromobacter xylosoxidans: A Case Report and Comprehensive Literature Review
- Achromobacter xylosoxidans Infection Following Total Knee Arthroplasty
- A Case of Septic Shock caused by Achromobacter xylosoxidans in an Immunocompetent Female Patient after Extracorporeal Shock Wave Lithotripsy for a Ureteral Stone