J Korean Ophthalmol Soc.
2011 Jun;52(6):734-737. 10.3341/jkos.2011.52.6.734.
Spontaneous Eyeball Rupture in a 94-Year-Old Patient
- Affiliations
-
- 1Department of Ophthalmology, Bundang CHA Hospital, CHA University, Seongnam, Korea. eye@cha.ac.kr
- 2Department of Pathology, Bundang CHA Hospital, CHA University, Seongnam, Korea.
- KMID: 2214647
- DOI: http://doi.org/10.3341/jkos.2011.52.6.734
Abstract
- PURPOSE
To report a case of spontaneous eye ball rupture without trauma in a 94-year-old patient.
CASE SUMMARY
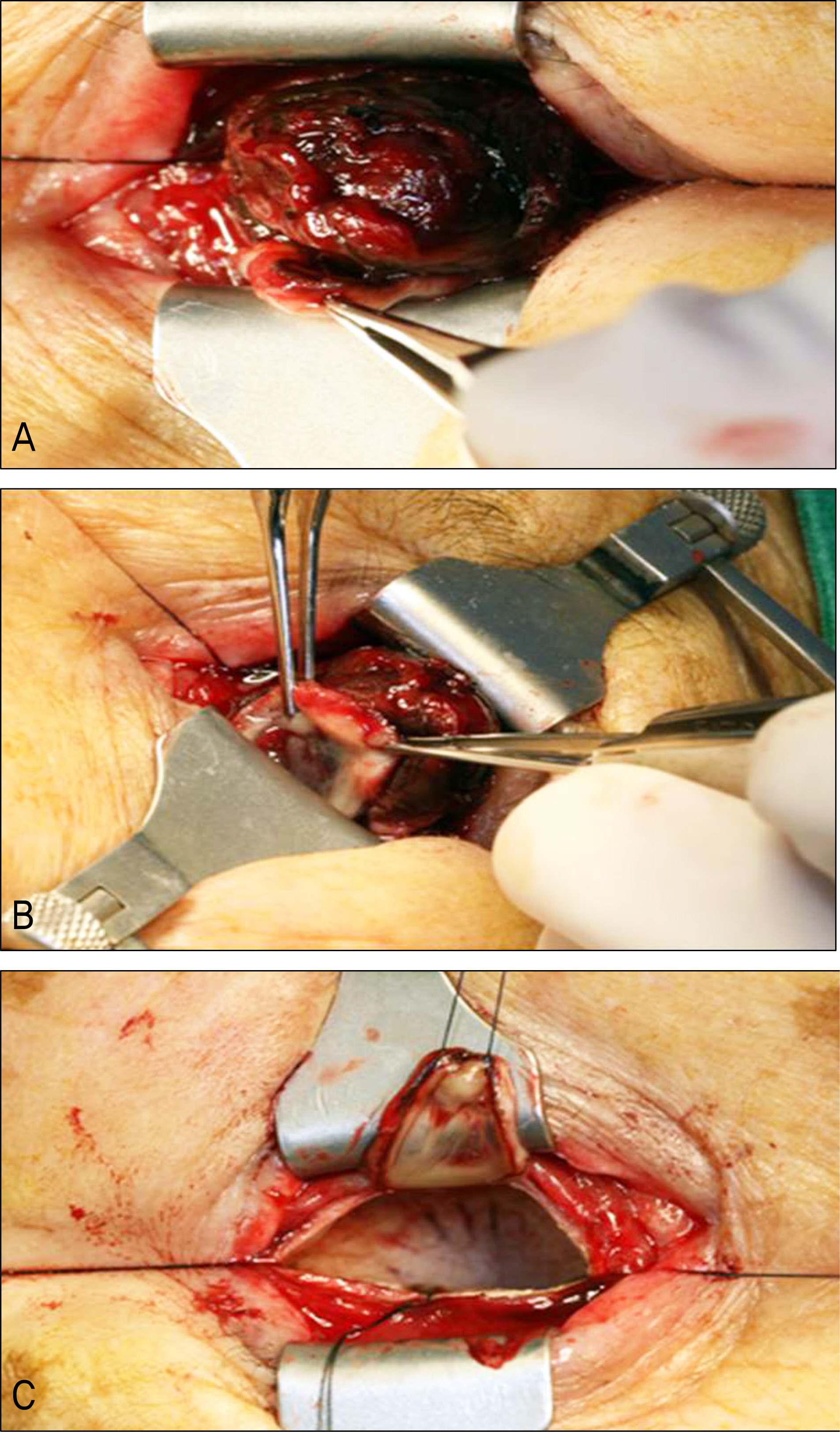
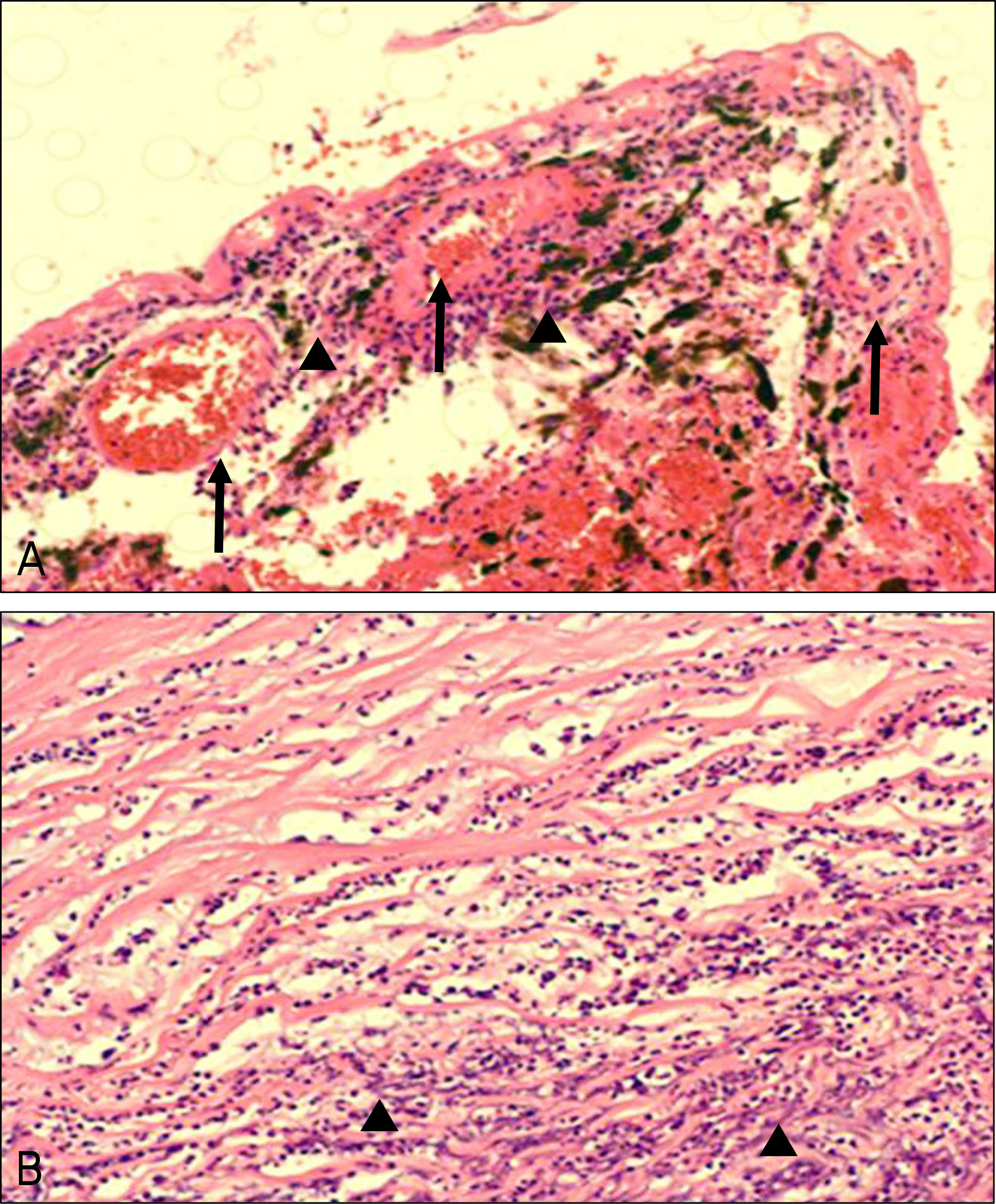
A 94-year-old female patient diagnosed with cataract in both eyes 20 years was referred to this ophthalmologic department for treatment consultation of a painful left eye with spontaneous bleeding. She has used anti-cataract eye drops and artificial tears three times a day for several years without consulting a doctor. Fifteen days prior to presentation, the patient suffered severe left eyeball pain and headache and was diagnosed with acute angle-closure glaucoma secondary to hypermature cataract. She underwnet eviceration after ocular examination and systemic evaluation. Surgical findings included a thin cornea at the inferior limbus and protruding intraocular tissues. Additionally, the eyeball was filled with a blood clot from a choroidal hemorrhage. Morganella morganii were grown in a bacterial swap culture, and a corneal biopsy revealed suppurative inflammation.
CONCLUSIONS
In old age, a thin corneal limbus due to infection and complicated acute angle-closure glaucoma can cause massive suprachoroidal hemorrhage with spontaneous eyeball rupture.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Rutherford WJ. Spontaneous rupture of the glaucomatous eye: an illustrative case. Br J Ophthalmol. 1920; 4:282–4.
Article2. Winslow RL, Stevenson W 3rd, Yanoff M. Spontaneous expulsive choroidal hemorrhage. Arch Ophthalmol. 1974; 92:33–6.
Article3. Goldsmith C, Rene C. Massive spontaneous expulsive suprachoroidal haemorrhage in a blind glaucomatous eye treated with chronic topical steroid. Eye (Lond). 2003; 17:439–40.
Article4. Ophir A, Pikkel J, Groisman G. Spontaneous expulsive suprachoroidal hemorrhage. Cornea. 2001; 20:893–6.
Article5. Haugen OH, Kjeka O. Localized, extreme scleral thinning causing globe rupture during strabismus surgery. J AAPOS. 2005; 9:595–6.
Article6. Ung T, Williams CP, Canning CR. Globe rupture as a complication of intravitreal injection of triamcinolone. Eye (Lond). 2007; 21:423–4.
Article7. Tabandeh H, Flaxel C, Sullivan PM, et al. Scleral rupture during retinal detachment surgery: risk factors, management options, and outcomes. Ophthalmology. 2000; 107:848–52.8. Awad AH, Mullaney PB, Al-Hazmi A, et al. Recognized globe perforation during strabismus surgery: incidence, risk factors, and sequelae. J AAPOS. 2000; 4:150–3.
Article9. Dang Y, Racu C, Isenberg SJ. Scleral penetrations and perforations in strabismus surgery and associated risk factors. J AAPOS. 2004; 8:325–31.
Article10. Warwick R. Eugene Wolff's Anatomy of the Eye and Orbit. 7th ed.London: HK Lewis & Co;1976. p. 48–51.11. Fleming A, Dodman S, Crown JM, Corbett M. Extra-articular features in early rheumatoid disease. Br Med J. 1976; 1:1241–3.
Article12. Sipperley JO, Shore JW. Septic retinal cyst in endogenous Klebsiella endophthalmitis. Am J Ophthalmol. 1982; 94:124–5.
Article13. Tae KS, Kim TH, Moon YS, Chin HS. A case of klebsiella endogenous endophthalmitis accompanied by necrotizing scleral perforation. J Korean Ophthalmol Soc. 2003; 11:2680–6.14. Equi RA, Green WR. Endogenous Serratia marcescens endophthalmitis with dark hypopyon: case report and review. Surv Ophthalmol. 2001; 46:259–68.15. Taherian K, Sharma P, Prakash P, Azad R. Scleral perforations in strabismus surgery: incidence and role of prophylactic cryotherapy–a clinical and experimental study. Strabismus. 2004; 12:17–25.16. Yu YS, Chang BL. Scleral perforation after scleral buckling surgery for retinopathy of prematurity. Korean J Ophthalmol. 1999; 13:49–51.
Article17. Kwon JD, Kim SW, Park DH, Lee CH. A case of a traumatic eye-ball rupture in terrien's marginal degeneration and it's surgical repair. J Korean Ophthalmol Soc. 2006; 47:1166–70.18. Cunningham ET Jr, Whitcher JP, Kim RY. Morganella morganii postoperative endophthalmitis. Br J Ophthalmol. 1997; 81:170–1.
Article19. Tsanaktsidis G, Agarwal SA, Maloof AJ, et al. Postoperative Morganella morganii endophthalmitis associated with subclinical urinary tract infection. J Cataract Refract Surg. 2003; 29:1011–3.
Article20. Burstein NL. Preservative cytotoxic threshold for benzalkonium chloride and chlorhexidine digluconate in cat and rabbit corneas. Invest Ophthalmol Vis Sci. 1980; 19:308–13.22. Tripathi BJ, Tripathi RC. Cytotoxic effects of benzalkonium chloride and chlorobutanol on human corneal epithelial cells in vitro. Lens Eye Toxic Res. 1989; 6:395–403.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Splenic Rupture
- A Case of Spontaneous Rupture of Renal Pelvis without Identifiable Cause Treated Conservatively
- A Case of Spontaneous Rupture of the Kidney
- Spontaneous rupture of the esophagus associated with intramural rupture caused by ingestion of weedi...
- Two Cases of Spontaneous Rupture of the Kidney