J Korean Ophthalmol Soc.
2015 Sep;56(9):1439-1445. 10.3341/jkos.2015.56.9.1439.
Analysis of Visual Field Defect in Patient with Brain Lesion
- Affiliations
-
- 1Department of Ophthalmology, Dankook University Medical College, Cheonan, Korea. kseeye@hanmail.net
- KMID: 2214561
- DOI: http://doi.org/10.3341/jkos.2015.56.9.1439
Abstract
- PURPOSE
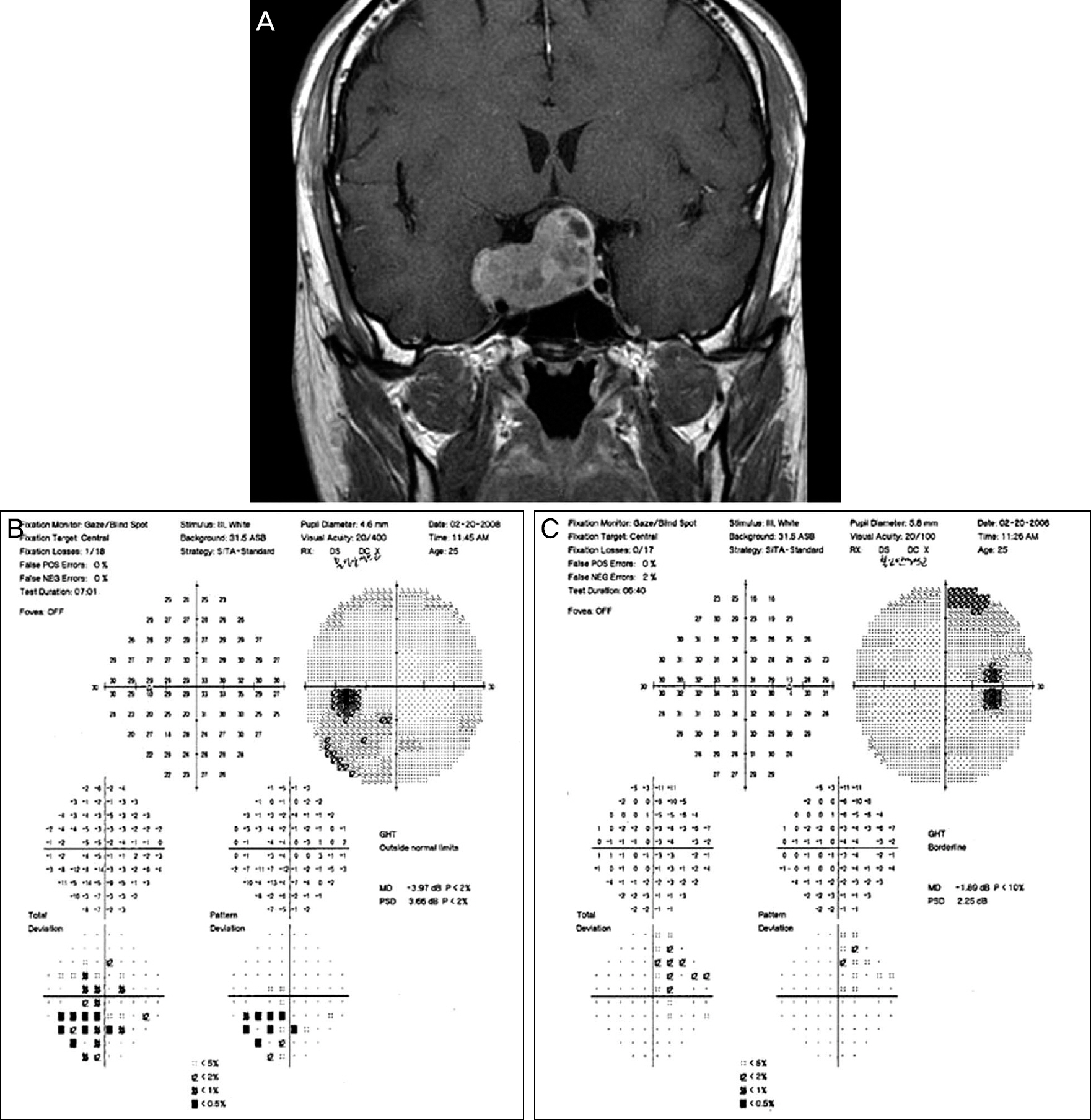
In this study we analyzed the results of visual field tests in patients diagnosed with a brain lesion in an ophthalmology clinic.
METHODS
The medical records of 55 patients who underwent visual field examinations and diagnosed with brain pathology using magnetic resonance imaging (MRI) from January 1, 2005 to June 30, 2014 were retrospectively investigated.
RESULTS
Of the 55 patients (M:F = 30:25), 31 displayed symmetrical hemianopsia, a typical visual field defect associated with brain lesions. Twenty-four patients showed atypical visual field defect (20 showed normal visual field despite the brain lesion, 3 had bilateral narrowing of the peripheral visual field in 2 cerebral infarctions and 1 multiple sclerosis, and 1 had horizontal inferior visual field defect in 1 eye from nasopharyngeal cancer).
CONCLUSIONS
Patients having a brain lesion with the optic tract invasion may present with atypical visual field defects. The peripheral visual field constriction and horizontal inferior visual field defect in 1 eye could be the visual field defect in patients with a brain lesion.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Bilateral Occipital Lobe Infarction Presenting as Bilateral Inferior Altitudinal Defects
Seong Wook Han, Seung Ah Chung
J Korean Ophthalmol Soc. 2019;60(3):298-302. doi: 10.3341/jkos.2019.60.3.298.
Reference
-
References
1. Kim MS, Jin KH, Kim JM. A clinical study of ocular symptoms in brain tumors. J Korean Ophthalmol Soc. 1990; 31:971–7.2. Kim WJ, Kim YD, Han MH. Carotid-cavernous fistula. J Korean Ophthalmol Soc. 1991; 32:223–31.3. Min IS, Jung HS, Kim MW. A clinical case report of right occipital lobe infarction. J Korean Ophthalmol Soc. 1982; 23:841–5.4. Kim HS, Lee JB, Han SH. Nontraumatic acquired paralytic strabismus. J Korean Ophthalmol Soc. 1994; 35:1127–31.5. Kang SM, Kim JH, Cheong JH. Relationship between location and size of pituitary adenoma and visual field change. J Korean Ophthalmol Soc. 2005; 46:1690–6.6. Yu DK, Choi MY. Clinical assessment of the patients diagnosed with intracranial lesion at an ophthalmology clinic. J Korean Ophthalmol Soc. 2004; 45:803–10.7. Anderson D, Faber P, Marcovitz S. . Pituitary tumors and the ophthalmologist. Ophthalmology. 1983; 90:1265–70.
Article8. Wray SH. Neuro-ophthalmologic manifestations of pituitary and parasellar lesions. Clin Neurosurg. 1977; 24:86–117.
Article9. Mejico LJ, Miller NR, Dong LM. Clinical features associated with lesions other than pituitary adenoma in patients with an optic chias-mal syndrome. Am J Ophthalmol. 2004; 137:908–13.
Article10. Zhang X, Kedar S, Lynn MJ. . Homonymous hemianopias: clinical-anatomic correlations in 904 cases. Neurology. 2006; 66:906–10.
Article11. Zihl J. Visual scanning behavior in patients with homonymous hemianopia. Neuropsychologia. 1995; 33:287–303.
Article12. Han SW, Sohn YH, Lee PH. . Pure homonymous hemianopia due to anterior choroidal artery territory infarction. Eur Neurol. 2000; 43:35–8.
Article13. Holt LJ, Anderson SF. Bilateral occipital lobe stroke with inferior altitudinal defects. Optometry. 2000; 71:690–702.14. Wein F, Miller NR. An unusual homonymous visual field defect. Surv Ophthalmol. 2000; 44:324–8.
Article15. Isa K, Miyashita K, Yanagimoto S. . Homonymous defect of macular vision in ischemic stroke. Eur Neurol. 2001; 46:126–30.
Article16. Gu XZ, Tsai JC, Wurdeman A. . Pattern of axonal loss in long standing papilledema due to idiopathic intracranial hypertension. Curr Eye Res. 1995; 14:173–80.17. Vidović T, Cerovski B, Vidović DH. . Inapparent visual field defects in multiple sclerosis patients. Coll Antropol. 2005; 29:Suppl 1. 67–73.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Prolonged Bilateral Inferior Altitudinal Visual Field Defect in a Young Migraineur
- Temporary amaurosis with persistent visual field defect following acute blood loss
- Clinical Application of Optokinetic Nystagmus
- The Differences of Visual Field Defects in Three Types of Primary Glaucoma
- Junctional scotoma in giant cerebral aneurysm