J Korean Ophthalmol Soc.
2010 Apr;51(4):631-635. 10.3341/jkos.2010.51.4.631.
Fibrous Encapsulation of Biodegradable Collagen Matrix After Trabeculectomy: A Case Report
- Affiliations
-
- 1Department of Ophthalmology, Han Gil Eye Hospital, Incheon, Korea. deskshot@naver.com
- KMID: 2213411
- DOI: http://doi.org/10.3341/jkos.2010.51.4.631
Abstract
- PURPOSE
Recently, biodegradable collagen matrix has been used as a possible substitute for anti-metabolite in trabeculectomy in order to control the responsiveness of the wound healing process. This paper reports a case of encapsulation of the biodegradable collagen matrix after trabeculectomy.
CASE SUMMARY
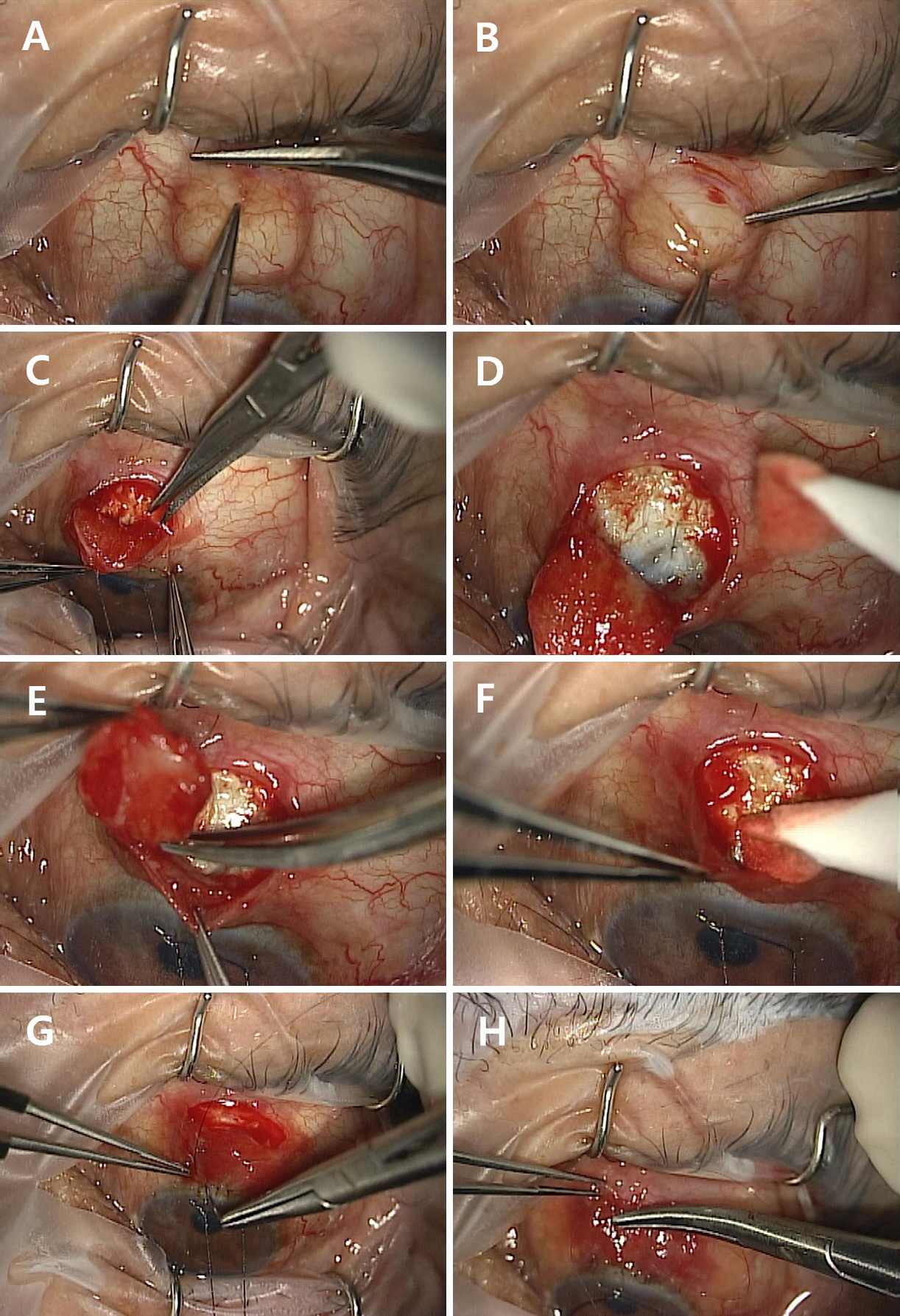
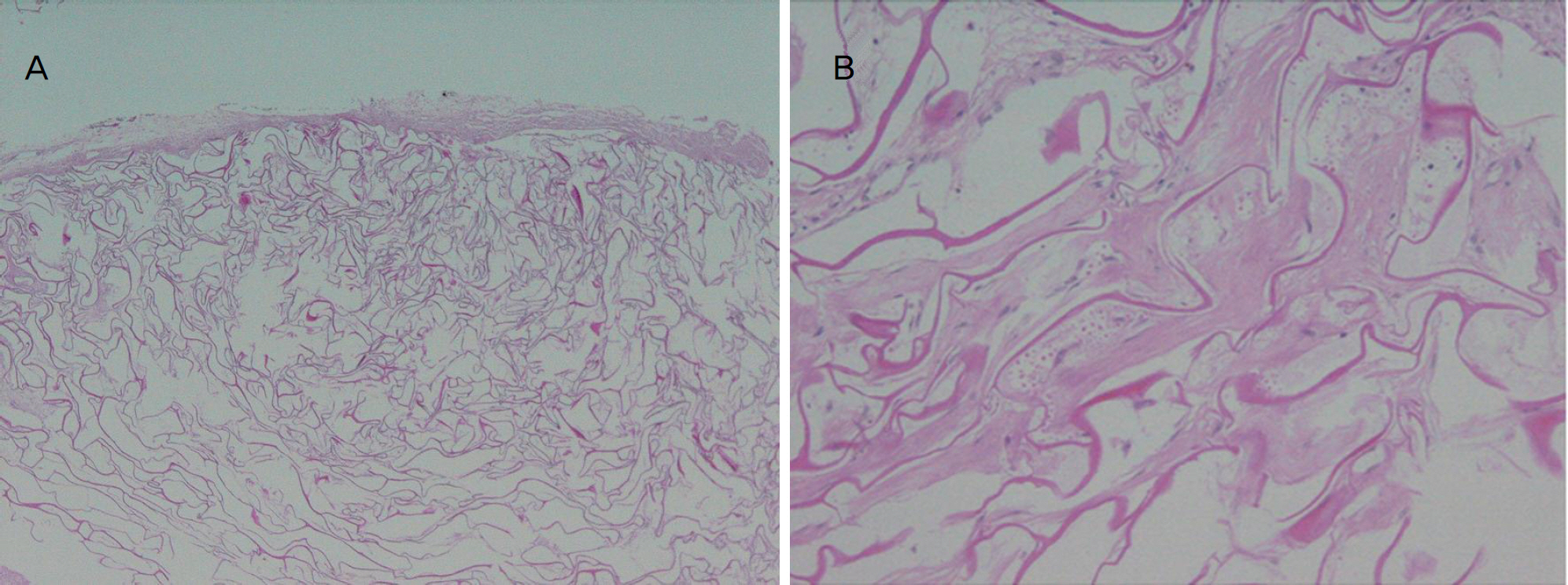
We conducted a fornix-based trabeculectomy on a 58-year-old man with medically uncontrollable steroid-induced glaucoma. We implanted biodegradable collagen matrix onto the sclera flap beneath the conjunctiva. Immediately after the surgery, we observed a localized bleb with high elevation. In the three months of follow-up, the bleb became encapsulated, and an increase in intraocular pressure was noted. During the wound revision, encapsulated material surrounded by thick fibrous membrane was found and removed from the subconjunctival space, followed by biopsy. Biopsy results demonstrated that amorphous collagenous material was surrounded by spindle and inflammatory cells.
CONCLUSIONS
It is important to note that the fibrous encapsulation of collagen material is a possible complication of biodegradable collagen matrix-augmented trabeculectomy.
MeSH Terms
Figure
Reference
-
References
1. Teng CC, Chi HH, Katzin HM. Histology and mechanism of abdominal operations. Am J Ophthalmol. 1959; 47:16–34.2. Addicks EM, Quigley HA, Green WR, Robin AL. Histologic characteristics of filtering blebs in glaucomatous eyes. Arch Ophthalmol. 1983; 101:795–8.
Article3. Azuara-blanco A, Katz LJ. Dysfunctional filtering blebs. Surv Ophthalmol. 1998; 43:93–126.
Article4. Kitazawa Y, Kawase K, Matsuhita H, Minobe M. Trabeculectomy with Mitomycin. Arch Ophthalmol. 1991; 109:1693–8.
Article5. Skuta GL, Beeson CC, Higginbotham EJ, et al. Intraoperative abdominal versus postoperative 5-fluorouracil in high risk glaucoma filtering surgery. Ophthalmology. 1992; 99:438–44.6. Cairns JE. Trabeculectomy-preliminary report of a new method. Am J Ophthalmol. 1968; 66:673–9.7. DeBry PW, Perkins TW, Heatley G, et al. Incidence of late-onset bleb-related complications following trabeculectomy with mitomycin. Arch Ophthalmol. 2002; 120:297–300.
Article8. Hsu WC, Ritch R, Krupin T, Chen HS. Tissue bioenginnering for surgical bleb defects: an animal study. Graefes Arch Clin Exp Ophthalmol. 2008; 246:709–17.9. Panek WC, Holland GN, Lee DA, Christensen RE. Glaucoma in patients with uveitis. Br J Ophthalmol. 1990; 74:223–7.
Article10. Shigeeda T, Tomidokoro A, Chen YN, et al. abdominal follow-up of initial trabeculectomy with mitomycin C for primary openangle glaucoma in Japanese patients. J Glaucoma. 2006; 15:195–9.11. Yaldo MK, Stamper RL. Long term effects of mitomycin on abdominal bleb, Lack of fibrovascular response following severe inflammation. Arch Ophthalmol. 1993; 111:824–6.12. Young MJ, Borras T, Walter M, Ritch R. Potential applications of tissue engineering to glaucoma. Arch Ophthalmol. 2005; 123:1725–31.13. Chen HS, Ritch R, Krupin T, Hsu WC. Control of filtering bleb structure through tissue bioengineering: An animal model. Invest Ophthalmol Vis Sci. 2006; 47:5310–4.
Article14. Aptel F, Dumas S, Denis P. Ultrasound biomicroscopy and abdominal coherence tomography imaging of filtering blebs after deep sclerectomy with new collagen implant. Eur J Ophthalmol. 2009; 19:223–30.15. Castner DG, Ratner BD. Biomedical surface science: Foundations to frontiers. Surface Science. 2002; 500:28–60.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trabeculectomy With Biodegradable Collagen Material: A Report of Two Cases
- The Analysis of the Clinical Findings and Effects of Biodegradable Collagen Matrix in Trabeculectomy
- Fibrous Hamartoma of Infancy : Report of A Case
- Comparison of Effects and Complications between Conventional Trabeculectomy and Trabeculectomy with a Collagen Matrix Insertion
- The Components of the Proliferative Membranes in Retinopathy of Prematurity