J Korean Ophthalmol Soc.
2010 Apr;51(4):552-557. 10.3341/jkos.2010.51.4.552.
An Analysis of Metamorphopsia Using Preferential Hyperacuity Perimeter Following Macular-off RRD Surgical Repair
- Affiliations
-
- 1Department of Ophthalmology, Pusan National University College of Medicine, Busan, Korea. jlee@pusan.ac.kr
- 2Medical Research Institute, Pusan National University, Busan, Korea.
- KMID: 2213398
- DOI: http://doi.org/10.3341/jkos.2010.51.4.552
Abstract
- PURPOSE
To determine the efficacy of using the preferential hyperacuity perimeter (PHP) for the analysis of metamorphopsia following macular-off rhegmatogenous retinal detachment (RRD) surgical repair.
METHODS
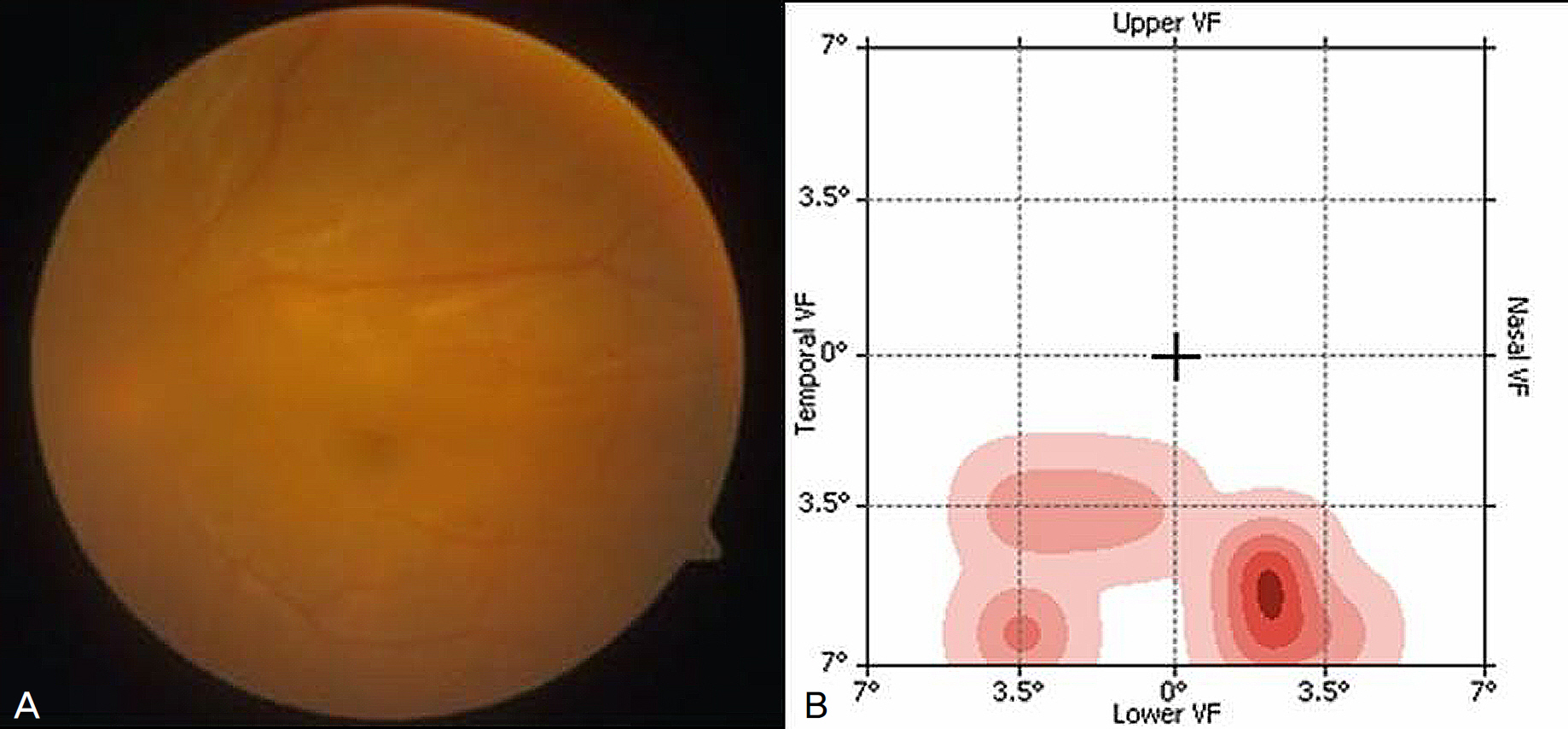
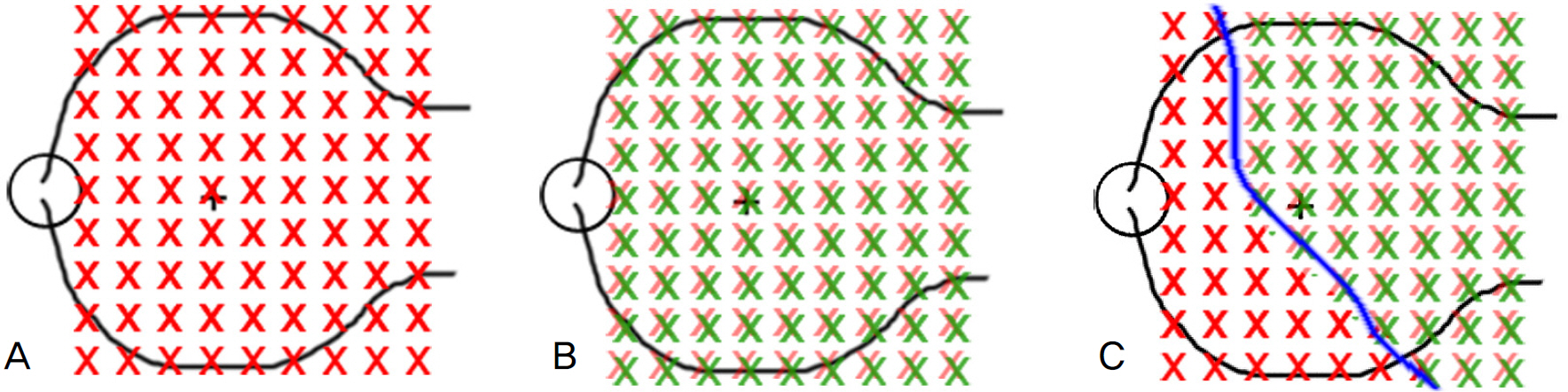
PHP examination was performed in those who complained of metamorphopsia after successful surgical reattachment of RRD. The subjective symptoms were evaluated based on a scale, ranging from 0 to 10, and were compared with the results of PHP examination. Patients age, duration of retinal detachment, pre and post-operative visual acuity, postoperative presence of subretinal fluid (SRF), surgical methods, presence of epiretinal membrane, and time from operation to PHP test were analyzed to find the correlation with the PHP results.
RESULTS
Of the 19 eyes included in this study, nine eyes were found to have a hyperacuity defect upon PHP examination. In this group, the subjective level of metamorphopsia was significantly worse (p<0.01), the age was significantly higher (p=0.02), and SRF persisted in the macula more frequently at two months postoperatively (p=0.04), as compared to those without the defect. There were no significant differences in the other factors.
CONCLUSIONS
Subjectively severe metamorphopsia after surgery for RRD could be confirmed objectively using PHP. In the case of older patients and persistent submacular fluid, metamorphopsia would develop more frequently due to displacement of the photoreceptors in the process of reattachment.
MeSH Terms
Figure
Reference
-
References
1. Wang Y, Li SY, Zhu M, Chen SJ, et al. Metamorphopsia after abdominalful retinal detachment surgery: an optical coherence abdominal study. Acta Ophthalmol Scand. 2005; 83:168–71.2. Amemiya T, Idia Y, Yoshida H. Subjective and objective ocular disturbance in reattached retina after surgery for retinal abdominal, with special reference to visual acuity and metamorphopsia. Ophthalmologica. 1983; 186:25–30.3. Framme C, Roider J, Hoerauf H, Laqua H. Complications after external retinal surgery in pseudophakic retinal detachment – are scleral buckling operations still current? Klin Monastbl Augenheilkd. 2000; 216:25–32.4. Kang JH, Yoon HS. Foveal retinal detachment diagnosed by abdominal coherence tomography after successful retinal detachment surgery. J Korean Ophthalmol Soc. 2005; 46:1637–41.5. Ahn JH, Chang MH, Kyung SE. Multifocal electroretinography after reattachment of macula-off retinal detachment. J Korean Ophthalmol Soc. 2008; 49:479–86.
Article6. Loewenstein A, Malach R, Goldstein M, et al. Replacing the ams-ler grid: A new method for monitoring patients with age-related macular degeneration. Ophthalmology. 2003; 110:996–70.7. Lee SC, Nam WH, Yu SY, Kwak HW. Correlation of OCT and preferential hyperacuity perimeter in exudative age-related abdominal degeneration. J Korean Ophthalmol Soc. 2006; 47:388–95.8. Kim ES, Nam WH, Yu SY, et al. Analysis of preferential Hyperacuity perimeter results in maculopathy caused by various retinal disease. J Korean Ophthalmol Soc. 2006; 47:381–87.9. Anderson DH, Stern WH, Fisher SK, et al. Retinal detachment in the cat: the pigment epithelial-photoreceptor interface. Invest Ophthalmol Vis Sci. 1983; 24:906–26.10. Anderson DH, Stern WH, Fisher SK, et al. The onset of pigment epithelial proliferation after retinal detachment. Invest Ophthalmol Vis Sci. 1981; 21:10–6.11. Anderson DH, Guerin CJ, Erickson PA, et al. Morphological abdominal in the reattached retina. Invest Ophthalmol Vis Sci. 1986; 27:168–83.12. Barr CC. The histopathology of successful retina reattachment. Retina. 1990; 10:189–94.13. Wilson DJ, Green WR. Histopathologic study of the effect of abdominall detachment surgery on 49 eyes obtained post mortem. Am J Ophthalmol. 1987; 103:167–79.14. Schocket LS, Witkin AJ, Fujimoto JG, et al. Ultrahigh-resolution optical coherence tomography in patients with decreased visual acuity after retinal detachment repair. Ophthalmology. 2006; 113:666–72.
Article15. Smith AJ, Telander DG, Zawadzki RJ, et al. High-resolution Fourier-domain optical coherence tomography and micro-perimetric findings after macula-off retinal detachment repair. Ophthalmology. 2008; 115:1923–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correlation of OCT and Preferential Hyperacuity Perimeter in Exudative Age-related Macular Degeneration
- Preferential Hyperacuity Perimeter (PHP) in Myopic CNV
- Preferential Hyperacuity Perimeter in Exudative AMD With Pigment Epithelial Detachment
- Analysis of Preferential Hyperacuity Perimeter Results in Maculopathy Caused by Various Retinal Diseases
- Characteristics and Surgical Outcome of Macular Holes Developing after Rhegmatogenous Retinal Detachment Repair