J Korean Surg Soc.
2013 Apr;84(4):209-215. 10.4174/jkss.2013.84.4.209.
Cancer cells with p53 deletion detected by fluorescent in situ hybridization in peritoneal drainage fluid is correlated with early peritoneal seeding in resectable pancreatic cancer
- Affiliations
-
- 1Department of Surgery, Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea. sunkim@plaza.snu.ac.kr, jangjy4@snu.ac.kr
- KMID: 2212465
- DOI: http://doi.org/10.4174/jkss.2013.84.4.209
Abstract
- PURPOSE
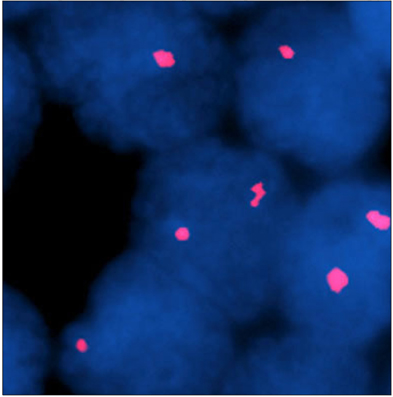
Free tumor cells in peritoneal fluid in patients with pancreatic cancer may have prognostic significance but there are few reports on methods for the effective detection of free tumor cells. The aims of this study were to identify free cancer cells in peritoneal fluid with fluorescent in situ hybridization (FISH) technique and to investigate its prognostic significance.
METHODS
Twenty-eight patients with resectable pancreatic cancer who underwent surgical resection were included. Peritoneal washing and peritoneal drainage fluid were examined by FISH for p53 deletion.
RESULTS
Among the study subjects, the R0 resection rate was 75%. None of the patients had positive cytology with Papanicolaou's method. p53 deletion was detected in 9 peritoneal washings (32.1%) and in 5 peritoneal drainage fluids (17.9%). After a median of 18 months of follow-up, 25 patients (89.3%) experienced recurrence and 14 patients (50.0%) had peritoneal seeding. Patients with p53 deletion detected in the peritoneal drainage fluid had positive radial margin (60.0% vs. 17.4%, P = 0.046) more frequently and a lower peritoneal metastasis free survival (median, 11.1 months vs. 30.3 months; P = 0.030). Curative resection (P < 0.001) and p53 deletion in peritoneal drainage fluid (P = 0.030) were independent risk factors of peritoneal metastasis free survival after multivariate analysis.
CONCLUSION
FISH technique detects free cancer cells with higher sensitivity compared to Papanicolaou's method. p53 deletion detected in peritoneal drainage fluid is correlated with positive radial resection margin and results in early peritoneal seeding. Patients with p53 deletion in peritoneal drainage fluid need more aggressive adjuvant treatment.
MeSH Terms
Figure
Reference
-
1. Kang MJ, Jang JY, Lee SE, Lim CS, Lee KU, Kim SW. Comparison of the long-term outcomes of uncinate process cancer and non-uncinate process pancreas head cancer: poor prognosis accompanied by early locoregional recurrence. Langenbecks Arch Surg. 2010. 395:697–706.2. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011. 14:101–112.3. American Joint Committee on Cancer. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. Ovary and primary peritoneal carcinoma. AJCC cancer staging manual. 2010. 7th ed. New York: Springer;493–506.4. Leach SD, Rose JA, Lowy AM, Lee JE, Charnsangavej C, Abbruzzese JL, et al. Significance of peritoneal cytology in patients with potentially resectable adenocarcinoma of the pancreatic head. Surgery. 1995. 118:472–478.5. Merchant NB, Conlon KC, Saigo P, Dougherty E, Brennan MF. Positive peritoneal cytology predicts unresectability of pancreatic adenocarcinoma. J Am Coll Surg. 1999. 188:421–426.6. Konishi M, Kinoshita T, Nakagohri T, Inoue K, Oda T, Takahashi S. Prognostic value of cytologic examination of peritoneal washings in pancreatic cancer. Arch Surg. 2002. 137:475–480.7. Ferrone CR, Haas B, Tang L, Coit DG, Fong Y, Brennan MF, et al. The influence of positive peritoneal cytology on survival in patients with pancreatic adenocarcinoma. J Gastrointest Surg. 2006. 10:1347–1353.8. Yamada S, Takeda S, Fujii T, Nomoto S, Kanazumi N, Sugimoto H, et al. Clinical implications of peritoneal cytology in potentially resectable pancreatic cancer: positive peritoneal cytology may not confer an adverse prognosis. Ann Surg. 2007. 246:254–258.9. Jimenez RE, Warshaw AL, Fernandez-Del Castillo C. Laparoscopy and peritoneal cytology in the staging of pancreatic cancer. J Hepatobiliary Pancreat Surg. 2000. 7:15–20.10. Martin JK Jr, Goellner JR. Abdominal fluid cytology in patients with gastrointestinal malignant lesions. Mayo Clin Proc. 1986. 61:467–471.11. Kelly KJ, Wong J, Gladdy R, Moore-Dalal K, Woo Y, Gonen M, et al. Prognostic impact of RT-PCR-based detection of peritoneal micrometastases in patients with pancreatic cancer undergoing curative resection. Ann Surg Oncol. 2009. 16:3333–3339.12. Barr Fritcher EG, Caudill JL, Blue JE, Djuric K, Feipel L, Maritim BK, et al. Identification of malignant cytologic criteria in pancreatobiliary brushings with corresponding positive fluorescence in situ hybridization results. Am J Clin Pathol. 2011. 136:442–449.13. Yoon YS, Lee DS, Min HC, Jang JY, Lee SE, Hwang DW, et al. Analysis of molecular cytogenetic alteration of pancreatic cancer identified by fluorescent in situ hybridization (FISH) and its clinical significance. Korean J Hepatobiliary Pancreat Surg. 2008. 12:75–85.14. Yachida S, Fukushima N, Sakamoto M, Matsuno Y, Kosuge T, Hirohashi S. Implications of peritoneal washing cytology in patients with potentially resectable pancreatic cancer. Br J Surg. 2002. 89:573–578.15. Meszoely IM, Lee JS, Watson JC, Meyers M, Wang H, Hoffman JP. Peritoneal cytology in patients with potentially resectable adenocarcinoma of the pancreas. Am Surg. 2004. 70:208–213.16. Vogel P, Ruschoff J, Kummel S, Zirngibl H, Hofstadter F, Hohenberger W, et al. Prognostic value of microscopic peritoneal dissemination: comparison between colon and gastric cancer. Dis Colon Rectum. 2000. 43:92–100.17. National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: ovarian cancer. Version 3. 2012 [Internet]. c2012. cited 2012 Aug 27. Fort Wathington: NCCN;Available from: http://www.nccn.org/professionals/physician_gls/pdf/ovarian.pdf.18. Higashiyama M, Doi O, Kodama K, Yokouchi H, Tateishi R, Horai T, et al. Pleural lavage cytology immediately after thoracotomy and before closure of the thoracic cavity for lung cancer without pleural effusion and dissemination: clinicopathologic and prognostic analysis. Ann Surg Oncol. 1997. 4:409–415.19. Doki Y, Kabuto T, Ishikawa O, Ohigashi H, Sasaki Y, Yamada T, et al. Does pleural lavage cytology before thoracic closure predict both patient's prognosis and site of cancer recurrence after resection of esophageal cancer? Surgery. 2001. 130:792–797.20. Ishikawa O, Wada H, Ohigashi H, Doki Y, Yokoyama S, Noura S, et al. Postoperative cytology for drained fluid from the pancreatic bed after "curative" resection of pancreatic cancers: does it predict both the patient's prognosis and the site of cancer recurrence? Ann Surg. 2003. 238:103–110.21. Ohigashi H, Ishikawa O, Sasaki Y, Yamada T, Furukawa H, Imaoka S, et al. K-ras point mutation in the nerve plexuses around the superior mesenteric artery in resectable adenocarcinoma of the pancreatic head: distribution pattern and related factors. Arch Surg. 2000. 135:1450–1455.22. Demeure MJ, Doffek KM, Komorowski RA, Wilson SD. Adenocarcinoma of the pancreas: detection of occult metastases in regional lymph nodes by a polymerase chain reaction-based assay. Cancer. 1998. 83:1328–1334.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of Molecular Cytogenetic Alteration of Pancreatic Cancer Identified by Fluorescent In Situ Hybridization (FISH) and its Clinical Significance
- Free Cancer Cell Detection in Peritoneal Cavitr of Gastric Cancer Patients by RT-PCR for CEA
- Clinical Outcomes according to Primary Treatment in Gastric Cancer Patients with Peritoneal Seeding
- Significance of Postoperative Peritoneal Drainage and Peritoneal Dialys is in Infants with congenital Heart Disease Who Underwent Open Heart Srugery
- Clinical Significance of Detection of Carcinoembryonic Antigen in Peritoneal Fluid by Reverse Transcription-Polymerase Chain Reaction in Patients with Gastric Cancer