J Korean Ophthalmol Soc.
2009 Apr;50(4):558-564. 10.3341/jkos.2009.50.4.558.
Analysis of Localized Retinal Nerve Fiber Layer Defects not Detected by Optical Coherence Tomography
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Pusan National University, Busan, Korea.
- 2Lee Chun Sik's Eye Clinic, Busan, Korea. Jea-sy@hanmail.net
- 3Department of Ophthalmology, Maryknoll Hospital, Busan, Korea.
- KMID: 2212257
- DOI: http://doi.org/10.3341/jkos.2009.50.4.558
Abstract
-
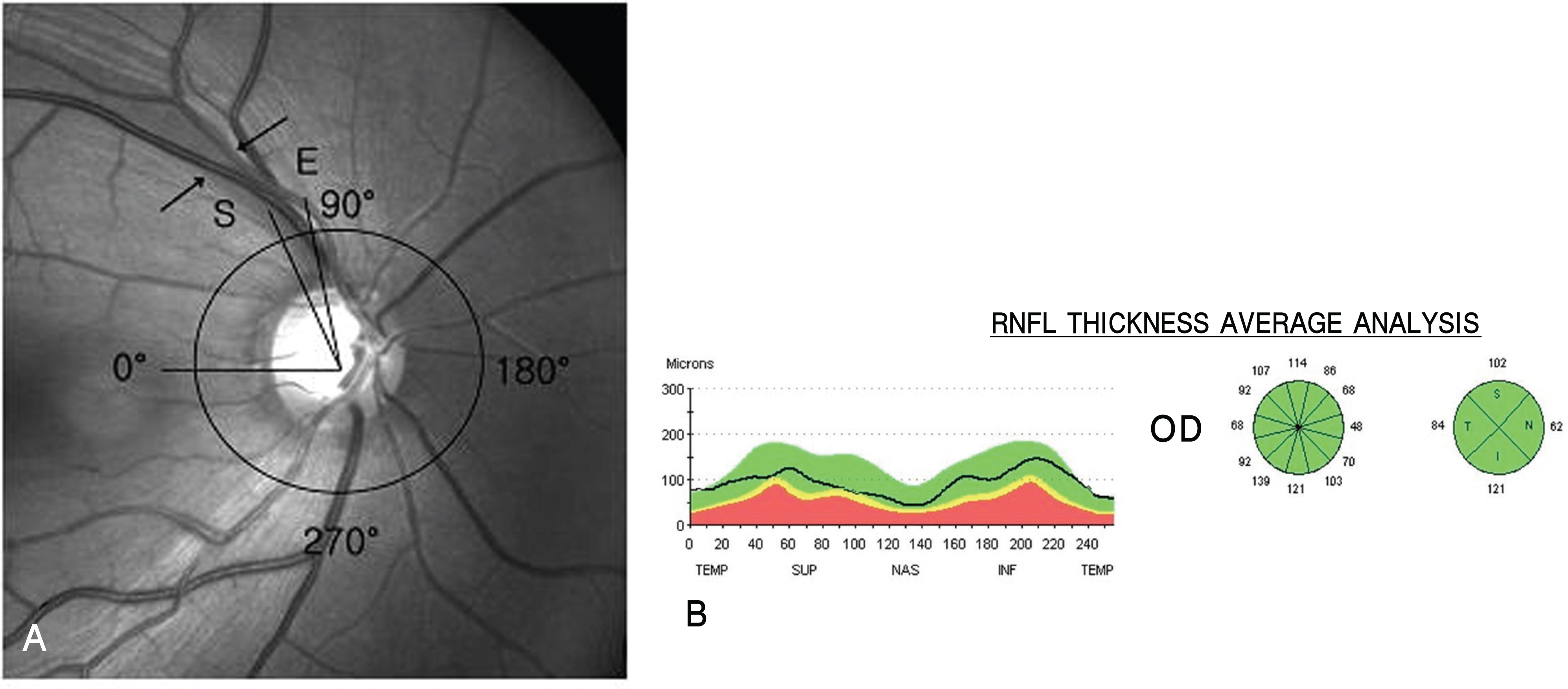
PURPOSE: To analyze localized RNFL defect cases that were identified in retinal nerve fiber layer (RNFL) fundus photographs but not in optical coherence tomography (OCT).
METHODS
Analysis of OCT scans and images was performed for 14 eyes (17 locations) that showed localized RNFL defects in RNFL fundus photographs but not in RNFL thickness average analysis.
RESULTS
With respect to the range of RNFL defects, 41.2% were less than 10degrees, 47.0% were 11 to 20degrees, and 11.8% were 21 to 30degrees. In 71.4% of the RNFL cases the defects were less than 10degrees and the decrease of RNFL thickness was not readily observable on the OCT scan images. In all cases of RNFL defects in the 11 to 30degrees range the decrease in RNFL thickness could be assessed on the OCT scan images. Nonetheless, the decrease of RNFL thickness could not be seen on the OCT analysis images in which the results of the RNFL thickness made through an automated computer algorithm were displayed.
CONCLUSIONS
The range of localized RNFL defects that were difficult to detect with OCT consisted of those cases that were almost less than 20degrees. The limitations of the OCT scan itself in patients with RNFL with an angular width defect less than 10degrees and the problems of RNFL thickness analysis processing in patients with an angular width of 11 to 30degrees may decrease the sensitivity of OCT in diagnosing RNFL defects.
Figure
Reference
-
References
1. Sommer A, Miller NR, Pollack I, et al. The nerve fiber layer in the diagnosis of glaucoma. Arch Ophthalmol. 1977; 95:2149–56.
Article2. Gupta N, Weinreb RN. New definitions of glaucoma. Curr Opin Ophthalmol. 1997; 8:38–41.
Article3. Varma R, Steinmann WC, Scott IU. Expert agreement in evaluating the optic disc for glaucoma. Ophthalmology. 1992; 99:215–21.
Article4. Quigley HA, Addicks EM, Green WR. Optic nerve damage in human glaucoma; III. Quantitative correlation of nerve fiber loss and visual field defects in glaucoma, ischemic neuropathy, papilledema and toxic neuropathy. Arch Ophthalmol. 1982; 100:135–46.5. Caprioli J, Miller JM, Sears M. Quantitative evaluation of the optic nerve head in patients with unilateral visual field loss from primary open angle glaucoma. Ophthalmology. 1987; 94:1484–7.6. Sommer A, Katz J, Quigley HA, et al. Clinically detectable nerve fiber atrophy precedes the onset of glaucomatous field loss. Arch Ophthalmol. 1991; 109:77–83.
Article7. Tuulonen A, Lehtola J, Airaksinen PJ. Nerve fiber layer defects with normal visual fields; Do normal optic disc and normal visual field indicate absence of glaucomatous abnormality? Ophthalmology. 1993; 100:587–98.8. Quigley HA, Katz J, Derick RJ, et al. An evaluation of optic disc and nerve fiber layer examinations in monitoring progression of early glaucoma damage. Ophthalmology. 1992; 99:19–28.
Article9. Schuman JS, Hee MR, Puliafito CA, et al. Quantification of nerve fiber layer thickness in normal and glaucomatous eyes using optical coherence tomography. Arch Ophthalmol. 1995; 113:586–96.
Article10. Hwang JM, Kim TW, Park KH, et al. Correlation between topographic profiles of localized retinal nerve fiber layer defects as determined by optical coherence tomography and red-free fundus photography. J Glaucoma. 2006; 15:223–8.
Article11. Jeoung JW, Park KH, Kim TW, et al. Diagnostic ability of optical coherence tomography with a normative database to detect localized retinal nerve fiber layer defects. Ophthalmology. 2005; 112:2157–63.
Article12. Budenz DL, Michael A, Chang RT, et al. Sensitivity and specificity of the stratus OCT for perimetric glaucoma. Ophthalmology. 2005; 112:3–9.13. Teesalu P, Tuulonen A, Airaksinen PJ. Optical coherence tomography and localized defects of the retinal nerve fiber layer. Acta Ophthalmol Scand. 2000; 78:49–52.
Article14. Pieroth L, Schuman JS, Hertzmark E, et al. Evaluation of focal defects of the nerve fiber layer using optical coherence tomography. Ophthalmology. 1999; 106:570–9.
Article15. Mikelberg FS, Yidegiligne HM, Shulzer M. Optic nerve axon count and axon diameter in patients with ocular hypertension and normal visual fields. Ophthalmology. 1995; 102:342–8.16. Quigley HA, Miller NR, George T. Clinical evaluation of the nerve fiber layer atrophy as an indicator of glaucomatous optic nerve damage. Arch Ophthalmol. 1980; 98:1564–71.17. Greenfield D, Knighton RW, Huang XR. Effect of corneal polari-zation axis on assessment of retinal nerve fiber layer thickness by scanning laser polarimetry. Am J Ophthalmol. 2000; 129:715–22.
Article18. Morgan JE, Waldock A. Scanning laser polarimetry of the normal human retinal nerve fiber layer: A quantitative analysis. Am J Ophthalmol. 2000; 129:76–82.
Article19. Zangwill LM, Williams J, Berry CC, et al. A comparison of optical coherence tomography and retinal nerve fiber layer photography for detection of nerve fiber layer damage in glaucoma. Ophthalmology. 2000; 107:1309–15.
Article20. Soliman MA, Van Den Berg TJ, Ismaeil AA, et al. Retinal nerve fiber layer analysis: relationship between optical coherence tomography and red-free photography. Am J Ophthalmol. 2002; 133:187–95.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of Table Parameters of Stratus OCT in Detection of Localized Retinal Nerve Fiber Layer Defects
- False Negative Findings of Optical Coherence Tomography in Eyes with Localized Nerve Fiber Layer Defects
- Usefulness of Automated Measurements of Localized Retinal Nerve Fiber Layer Defects Area Using Significance Map
- Visual Field Cluster Map Corresponding to Retinal Nerve Fiber Layer Sectors in Glaucoma
- Asymmetry Analysis of the Retinal Nerve Fiber Layer Thickness in Normal Eyes using Optical Coherence Tomography