J Korean Surg Soc.
2011 May;80(5):342-347. 10.4174/jkss.2011.80.5.342.
Characteristic clinical and pathologic features for preoperative diagnosed groove pancreatitis
- Affiliations
-
- 1Department of Surgery, Catholic University of Daegu School of Medicine, Deagu, Korea. hyskhk@cu.ac.kr
- KMID: 2212159
- DOI: http://doi.org/10.4174/jkss.2011.80.5.342
Abstract
- PURPOSE
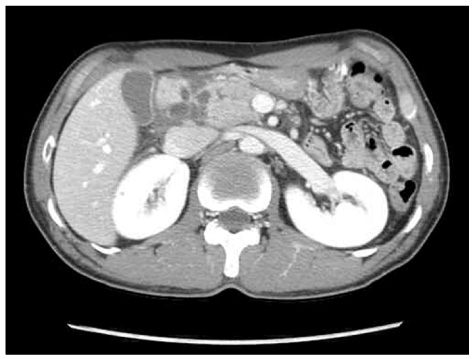
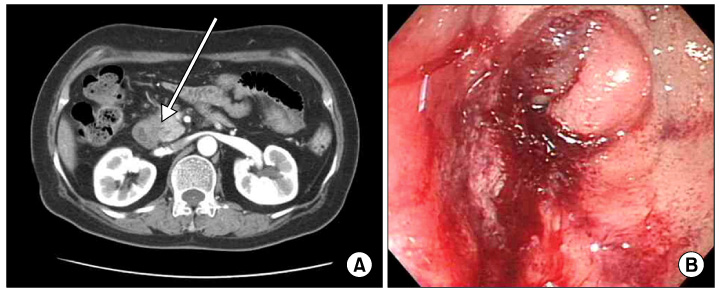
Groove pancreatitis is a rare specific form of chronic pancreatitis that extends into the anatomical area between the pancreatic head, the duodenum, and the common bile duct, which are referred to as the groove areas. We present the diagnostic modalities, pathological features and clinical outcomes of a series of symptomatic patients with groove pancreatitis who underwent pancreaticoduodenectomy.
METHODS
Six patients undergoing pancreaticoduodenectomy between May 2006 and May 2009 due to a clinical diagnosis of symptomatic groove pancreatitis were retrospectively included in the study.
RESULTS
Five cases were male and one case was female, with a median age at diagnosis of 50 years. Their chief complaints were abdominal pain and vomiting. Abdominal computed tomography, endoscopic ultrasound and endoscopic retrograde cholangiopancreatography were performed. Preoperative diagnosis of all patients was groove pancreatitis. Histological finding was compatible with clinically diagnosed groove pancreatitis in five patients and the pathologic diagnosis of the remaining patient was adenocarcinoma of distal common bile duct. Following pancreaticoduodenectomy, four living patients experienced significant pain alleviation.
CONCLUSION
The diagnostic imaging modalities of choice for groove pancreatitis are computed tomography and endoscopic ultrasonography. If symptomatic groove pancreatitis is suspected, careful follow-up of patients is necessary and pancreaticoduodenectomy seems to be a reasonable treatment option.
Keyword
MeSH Terms
Figure
Reference
-
1. Stolte M, Weiss W, Volkholz H, Rösch W. A special form of segmental pancreatitis: "groove pancreatitis". Hepatogastroenterology. 1982. 29:198–208.2. Hwang JY, Park KS, Cho KB, Hwang JS, Ahn SH, Park SK, et al. Segmental groove pancreatitis: report of one case. Korean J Intern Med. 2003. 18:234–237.3. Lee TH, Park SH, Lee CK, Chung IK, Kim SJ. Ectopic opening of the common bile duct accompanied by groove pancreatitis: diagnosis with magnetic resonance cholangiopancreatography. Gastrointest Endosc. 2010. 71:1301–1302.4. Park KH, Yoo KS, Chung YW, Kim KO, Park CH, Kim JH, et al. A case of groove pancreatitis with a characteristic pathologic feature. Korean J Gastroenterol. 2007. 49:187–191.5. Becker V, Mischke U. Groove pancreatitis. Int J Pancreatol. 1991. 10:173–182.6. Zamboni G, Capelli P, Scarpa A, Bogina G, Pesci A, Brunello E, et al. Nonneoplastic mimickers of pancreatic neoplasms. Arch Pathol Lab Med. 2009. 133:439–453.7. Adsay NV, Zamboni G. Paraduodenal pancreatitis: a clinico-pathologically distinct entity unifying "cystic dystrophy of heterotopic pancreas", "para-duodenal wall cyst", and "groove pancreatitis". Semin Diagn Pathol. 2004. 21:247–254.8. Shudo R, Obara T, Tanno S, Fujii T, Nishino N, Sagawa M, et al. Segmental groove pancreatitis accompanied by protein plugs in Santorini's duct. J Gastroenterol. 1998. 33:289–294.9. Balakrishnan V, Chatni S, Radhakrishnan L, Narayanan VA, Nair P. Groove pancreatitis: a case report and review of literature. JOP. 2007. 8:592–597.10. Mohl W, Hero-Gross R, Feifel G, Kramann B, Püschel W, Menges M, et al. Groove pancreatitis: an important differential diagnosis to malignant stenosis of the duodenum. Dig Dis Sci. 2001. 46:1034–1038.11. Itoh S, Yamakawa K, Shimamoto K, Endo T, Ishigaki T. CT findings in groove pancreatitis: correlation with histopathological findings. J Comput Assist Tomogr. 1994. 18:911–915.12. Blasbalg R, Baroni RH, Costa DN, Machado MC. MRI features of groove pancreatitis. AJR Am J Roentgenol. 2007. 189:73–80.13. Yamaguchi K, Tanaka M. Groove pancreatitis masquerading as pancreatic carcinoma. Am J Surg. 1992. 163:312–316.14. Levenick JM, Gordon SR, Sutton JE, Suriawinata A, Gardner TB. A comprehensive, case-based review of groove pancreatitis. Pancreas. 2009. 38:e169–e175.15. Isayama H, Kawabe T, Komatsu Y, Sasahira N, Toda N, Tada M, et al. Successful treatment for groove pancreatitis by endoscopic drainage via the minor papilla. Gastrointest Endosc. 2005. 61:175–178.16. Rahman SH, Verbeke CS, Gomez D, McMahon MJ, Menon KV. Pancreatico-duodenectomy for complicated groove pancreatitis. HPB (Oxford). 2007. 9:229–234.17. Casetti L, Bassi C, Salvia R, Butturini G, Graziani R, Falconi M, et al. "Paraduodenal" pancreatitis: results of surgery on 58 consecutives patients from a single institution. World J Surg. 2009. 33:2664–2669.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Groove Pancreatitis with a Characteristic Pathologic Feature
- Groove Pancreatitis Masquerading as Pancreatic Carcinoma—Detected on 18F-FDG PET/CT
- Segmental Groove Pancreatitis: Report of One Case
- Endoscopic Ultrasound in the Diagnosis of Pancreatoduodenal Groove Pathology: Report of Three Cases and Brief Review of the Literature
- A Case of Non-alcoholic Chronic Pancreatitis Showing Characteristic Imaging Features