J Pathol Transl Med.
2016 Jan;50(1):67-70. 10.4132/jptm.2015.07.28.
IgG4-Related Disease Presented as a Mural Mass in the Stomach
- Affiliations
-
- 1Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jihunkim@amc.seoul.kr
- 2Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 4Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2211405
- DOI: http://doi.org/10.4132/jptm.2015.07.28
Abstract
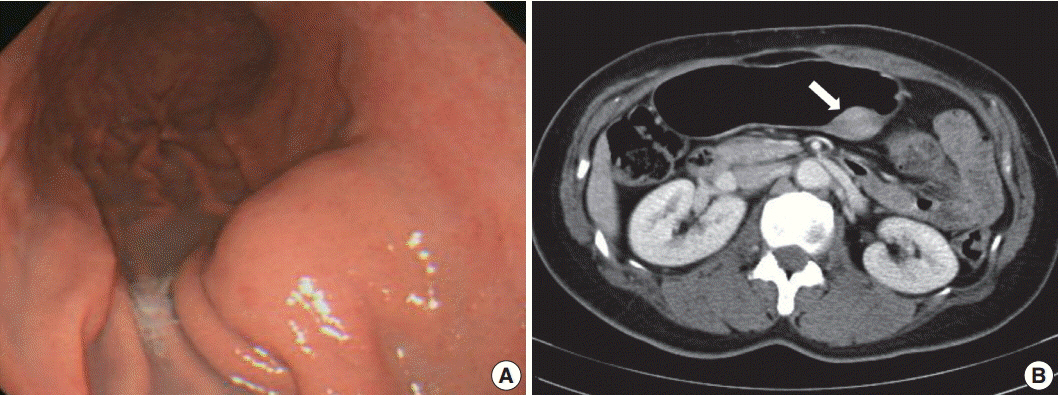
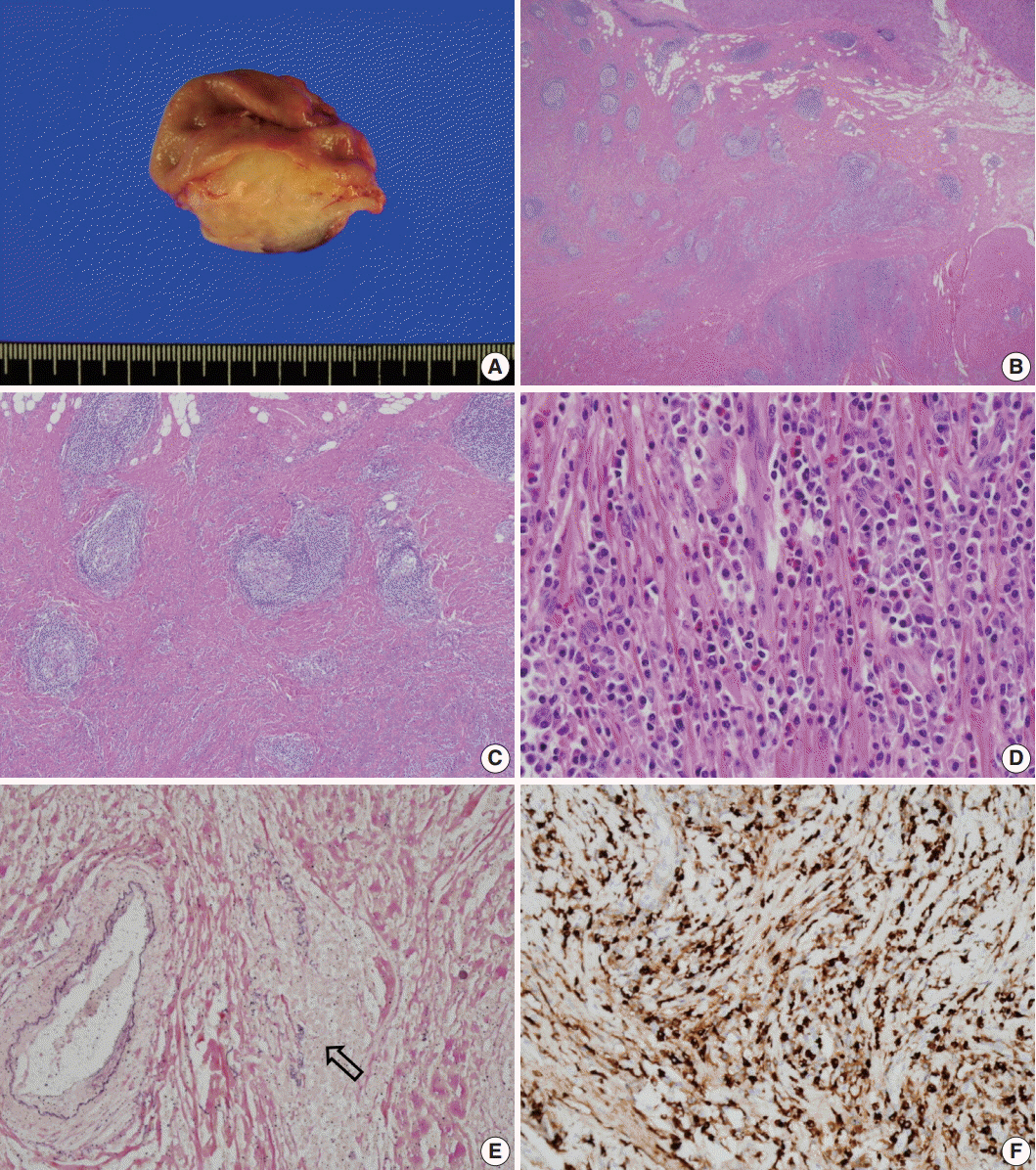
- Isolated gastric IgG4-related disease (IgG4-RD) is a very rare tumefactive inflammatory condition, with only a few cases reported to date. A 48-year-old woman was incidentally found to have a subepithelial tumor in the stomach. Given a presumptive diagnosis of gastrointestinal stromal tumor or neuroendocrine tumor, she underwent wedge resection. The lesion was vaguely nodular and mainly involved the submucosa and proper muscle layer. Microscopically, all classical features of type I autoimmune pancreatitis including lymphoplasmacytic infiltration, storiform fibrosis, obliterative phlebitis, and numerous IgG4-positive plasma cells were seen. She had no evidence of IgG4-RD in other organs. Although very rare, IgG4-RD should be considered one of the differential diagnoses in the setting of gastric wall thickening or subepithelial mass-like lesion. Deep biopsy with awareness of this entity might avoid unnecessary surgical intervention.
MeSH Terms
Figure
Cited by 2 articles
-
IgG4-related Disease in the Stomach which Was Confused with Gastrointestinal Stromal Tumor (GIST): Two Case Reports and Review of the Literature
Ho Seok Seo, Yoon Ju Jung, Cho Hyun Park, Kyo Young Song, Eun Sun Jung
J Gastric Cancer. 2018;18(1):99-107. doi: 10.5230/jgc.2018.18.e8.Gastric IgG4-related disease presenting as a mass lesion and masquerading as a gastrointestinal stromal tumor
Banumathi Ramakrishna, Rohan Yewale, Kavita Vijayakumar, Patta Radhakrishna, Balakrishnan Siddartha Ramakrishna
J Pathol Transl Med. 2020;54(3):258-262. doi: 10.4132/jptm.2020.02.10.
Reference
-
1. Hamano H, Kawa S, Horiuchi A, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001; 344:732–8.
Article2. Kamisawa T, Funata N, Hayashi Y, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003; 38:982–4.
Article3. Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012; 366:539–51.
Article4. Deshpande V, Zen Y, Chan JK, et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012; 25:1181–92.5. Koizumi S, Kamisawa T, Kuruma S, et al. Immunoglobulin G4-related gastrointestinal diseases, are they immunoglobulin G4-related diseases? World J Gastroenterol. 2013; 19:5769–74.
Article6. Strehl JD, Hartmann A, Agaimy A. Numerous IgG4-positive plasma cells are ubiquitous in diverse localised non-specific chronic inflammatory conditions and need to be distinguished from IgG4-related systemic disorders. J Clin Pathol. 2011; 64:237–43.
Article7. Zhang L, Notohara K, Levy MJ, Chari ST, Smyrk TC. IgG4-positive plasma cell infiltration in the diagnosis of autoimmune pancreatitis. Mod Pathol. 2007; 20:23–8.
Article8. Witkiewicz AK, Kennedy EP, Kennyon L, Yeo CJ, Hruban RH. Synchronous autoimmune pancreatitis and infiltrating pancreatic ductal adenocarcinoma: case report and review of the literature. Hum Pathol. 2008; 39:1548–51.
Article9. Na KY, Sung JY, Jang JY, et al. Gastric nodular lesion caused by IgG4-related disease. Pathol Int. 2012; 62:716–8.
Article10. Baez JC, Hamilton MJ, Bellizzi A, Mortelé KJ. Gastric involvement in autoimmune pancreatitis: MDCT and histopathologic features. JOP. 2010; 11:610–3.11. Kaji R, Okabe Y, Ishida Y, et al. Autoimmune pancreatitis presenting with IgG4-positive multiple gastric polyps. Gastrointest Endosc. 2010; 71:420–2.
Article12. Chetty R, Serra S, Gauchotte G, Märkl B, Agaimy A. Sclerosing nodular lesions of the gastrointestinal tract containing large numbers of IgG4 plasma cells. Pathology. 2011; 43:31–5.
Article13. Rollins KE, Mehta SP, O’Donovan M, Safranek PM. Gastric IgG4-related autoimmune fibrosclerosing pseudotumour: a novel location. ISRN Gastroenterol. 2011; 2011:873087.
Article14. Kim DH, Kim J, Park DH, et al. Immunoglobulin G4-related inflammatory pseudotumor of the stomach. Gastrointest Endosc. 2012; 76:451–2.
Article15. Bateman AC, Sommerlad M, Underwood TJ. Chronic gastric ulceration: a novel manifestation of IgG4-related disease? J Clin Pathol. 2012; 65:569–70.
Article16. Fujita T, Ando T, Sakakibara M, Hosoda W, Goto H. Refractory gastric ulcer with abundant IgG4-positive plasma cell infiltration: a case report. World J Gastroenterol. 2010; 16:2183–6.
Article17. Kamisawa T, Okazaki K, Kawa S, Shimosegawa T, Tanaka M; Research Committee for Intractable Pancreatic Disease and Japan Pancreas Society. Japanese consensus guidelines for management of autoimmune pancreatitis: III. Treatment and prognosis of AIP. J Gastroenterol. 2010; 45:471–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Gastric IgG4-related disease presenting as a mass lesion and masquerading as a gastrointestinal stromal tumor
- MRI Findings for IgG4-Related Disease Involving the Liver and Gallbladder
- Immunoglobulin G4-Related Inflammatory Pseudotumor Presenting as a Solitary Mass in the Stomach
- Immunoglobulin G4-Related Lung Disease Mimicking Lung Cancer: Two Case Reports
- Unusual Manifestation of Immunoglobulin G4-Related Disease Involving the Upper Arm: A Case Report