J Korean Soc Spine Surg.
2006 Sep;13(3):170-176. 10.4184/jkss.2006.13.3.170.
Finite Element Model of A-P Instrimentation in Thoracolumbar Burst Fracture
- Affiliations
-
- 1Department of Orthoapedic Surgery, Guri Hospital, Hanyang University College of Medicine, Korea.
- 2School of Advanced Technology, Kyung Hee University, Korea. yoonhkim@khu.ac.kr
- 3East-West Neo Medical Center, Kyung Hee University, Korea.
- KMID: 2209638
- DOI: http://doi.org/10.4184/jkss.2006.13.3.170
Abstract
-
STUDY DESIGN: Finite element models of the thoracolumbar spine with various techniques used in spinal fractures were developed to investigate the effects of fixation techniques on spinal stiffness.
OBJECTIVES
To develop finite element models of the thoracolumbar spine with various fixation techniques to compare their spinal stiffness characteristics. SUMMARY OF LITERATURE REVIEW: Various anterior and posterior instrumentation options have been applied to stabilize unstable burst fractures of the thoracolumbar spines. The biomechanical effects of different instrumentation options on spinal stability are still unknown.
MATERIALS AND METHODS
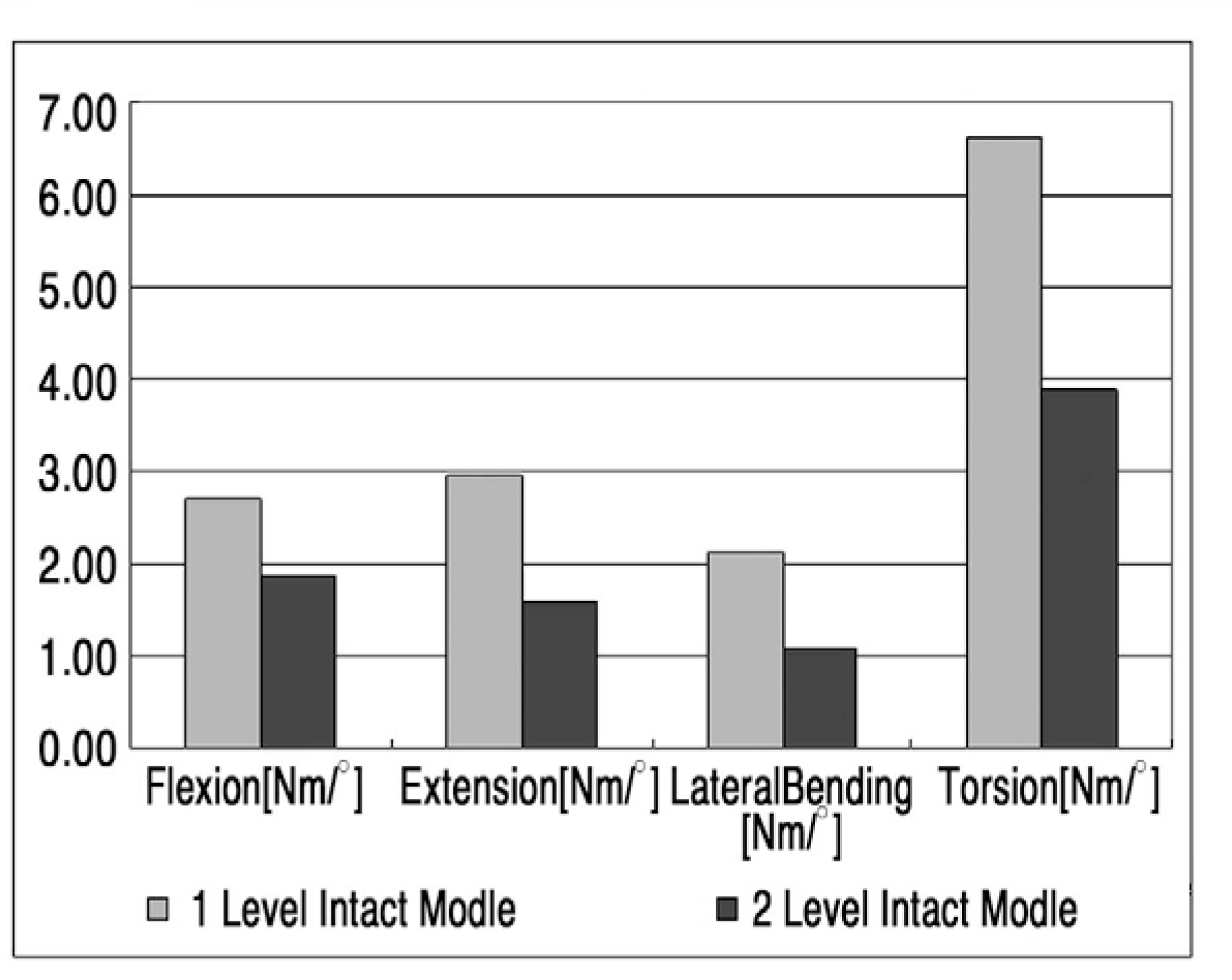
The 3-D finite element model of the human thoracolumbar spine (T12-L2) was reconstructed from CT images. Various anterior and posterior instrumentation techniques, 1-rod and 2-rod anterior fixations, anterior fixations with posterior fixation, and posterior fixation only, were virtually performed in the developed model with a long cage after corpectomy. Five loading cases, axial compression, flexion, extension, lateral bending, and torsion, were applied up to 1000 N and 10 Nm, respectively. The axial displacement and the rotations of T12 with respect to L2 were measured to analyze the stiffness of the spinal segments.
RESULTS
The posterior fixation technique increased the stiffness of the spine the most. The addition of an anterior rod from 1 to 2 increased the stiffness significantly without posterior fixation, but little effect was found with posterior fixation. Among all fixation techniques, the inter-segmental stiffnesses were similar to those of the intact model in torsion cases. In the other loading cases, the inter-segmental stiffnesses were much greater than those of the intact models.
CONCLUSIONS
Finite element models of the thoracolumbar spine were developed with various fixation methods. The intact models were validated with in-vitro experimental tests. The posterior fixation technique had a more significant effect on spine stability than did anterior fixation. And anteroposterior fixation techniques provided increased spinal stiffness
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Lumbar Spine Fracture
Seung-Wook Back, Hyun-Joong Cho, Ye-Soo Park
J Korean Fract Soc. 2011;24(3):277-287. doi: 10.12671/jkfs.2011.24.3.277.
Reference
-
01). Wood KB., Bohn D., Mehbod A. Anterior versus posteri- or treatment of stable thoracolumbar burst fractures without neurologic deficit. J Spinal Disord Tech. 2005. 18:S15–S23.02). Goto K., Tajima N., Chosa E., Totoribe K., Kubo S., Kuroki H, et al. Effects of lumbar spinal fusion on the other lumbar intervertebral levels. J Orthop Sci. 2003. 8:577–584.03). Natarajan RN., Garretson RB., Biyani A., Lim TH., Andersson GBJ., An HS. Effects of slip severity and loading direction on the stability of isthmic spondyloisthesis: A finite element model study. Spine. 2003. 28:1103–1112.04). Natarajan RN., Andersson GBJ. The influence of lumbar disc height and cross-sectional area on the mechanical response of the disc to physiologic loading. Spine. 1999. 24:1973–1881.
Article05). Argoubi M., Shirazi-Adl A. Poroelastic creep response analysis of a lumbar motion segment in compression. J. Biomechanics. 1996. 29:1331–1339.06). Lu YM., Hutton WC., Gharpuray VM. Do bending, twisting and diurnal fluid changes in the disc affect the propensity to prolapse? A viscoelastic finite element model. Spine. 1996. 21:2570–2579.
Article07). Campbell-Kyureghyan N., Jorgensen M., Burr D., Mar-ras W. The prediction of lumbar spine geometry: method development and validation. Clinical Biomechanics. 2005. 20:455–464.
Article08). Polikeit A., Ferguson SJ., Nolte LP., Orr TE. Factors influ-encing stresses in the lumbar spine after the insertion of intervertebral gages: finite element analysis. Eur Spine J. 2003. 12:413–420.09). Zhong ZC., Wei SH., Wang JP., Feng CK., Chen CS., Yu CH. Finite element analysis of the lumbar spine with a new cage using a topology optimization method. Medical Engineering & Physics. 2006. 28:90–98.
Article10). Goel VK., Ramirez SA., Kong W., Gilbertson LG. Can-cellous bone young' s modulus variation within the vertebral body of a ligamentous lumbar spine- Application of bone adaptive remodeling concepts. J Biomechanical Engineering. 1995. 117:226–271.11). Qiu TX., Teo EC., Lee KK., Ng HW., Yang K. Validation of T10-T11 finite element model and determination of instantaneous axes of rotations in three anatomical planes. Spine. 2003. 28:2694–2699.
Article12). Wang JL., Parnianpour M., Shirazi-Adl A., Engin AE. Rate effect on sharing of passive lumbar motion segment under load-controlled sagittal flexion: viscoelastic finite element analysis. Theoretical and Applied Fracture Mechanics. 1999. 32:119–128.
Article13). White AA., Panjabi MM. Clinical Biomechanics of the Spine. 2nd ed.Lippincott Williams & Wilkins Co.;p. 47. 1990.14). Panjabi MM., Oxland TR., Yamamoto I., Crisco JJ. Mechanical behavior of the human lumbar and lum-bosacral spine as shown by three-dimensional load-dis-placement curves. J Bone Joint Surg. 1994. 76:413–424.
Article15). Knop C., Lange U., Bastian L., Blauth M. Three-dimensional motion analysis wit Synex. Eur Spine J. 2000. 9:472–485.16). Kanayama M., Ng JTW., Cunningham BW., Abumi K., Kaneda K., McAfee PC. Biomechanical analysis of anterior versus circumferential spinal reconstruction for various anatomic stages of tumor lesions. Spine. 1999. 24:445–450.
Article17). Bastian L., Knop C., Lange U., Blauth M. Einfluβ eines Querverbinders oder einer Cerclage auf die mechanische Sta-bilit?t des Fixateur interne. Orthop?de. 1999. 28:714–722.
Article18). Wood KB., Bohn D., Mehbod A. Anterior versus posterior treatment of stable thoracolumbar burst fractures with-out neurologic deficit. Journal of spinal disord tech. 2005. 18:S15–S23.
Article19). Carl AL., Tranmer BI., Sachs BL. Anterolateral dynamized instrumentation and fusion for unstable thoracolumbar and lumbar burst fracutres. Spine. 1997. 22:686–690.20). McDonough PW., Davis R., Tribus C., Zdeblick TA. The management of acute thoracolumbar burst fractures with anterior corpectomy and Z-plate fixation. Spine. 2004. 29:1901–1909.
Article21). Payer M. Unstable burst fractures of the thoracolumbar junction: treatment by posterior bisegmental correction/fixation and staged anterior corpectomy and titanium cage implatation. Acta Neurochirurgica. 2006. 148:299–306.22). Pflugmacher R., Schleicher P., Schaefer J., Scholz M., Ludwig K., Khodadadyan-Klostermann C, et al. Biomechanical comparison of expandable cages for vertebral body replacement in thoracolumbar spine. Spine. 2004. 29:1413–1419.23). Schreiber U., Bence T., Grupp T., Steinhauser E., Muck-ley T., Mittelmeier W, et al. Is a single anterolateral screw-plate fixation sufficient for the treatment of spinal fractures in the thoracolumbar junction? A biomechanical in vitro investigation. Eur Spine J. 2005. 14:197–204.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative Study of Radiologic Changes after Conservative Treatment in Compression fracture and Stable Bursting Fracture of Thoracolumbar Spine
- Comparision of Classifications in the Thoracolumbar Burst Fractures
- Crush-Cleavage Fracture in Thoracolumbar and Lumbar Spine: Comparative Study with Type B Burst Fracture
- Biomechanical Efficacy of Various Anterior Spinal Fixation in Treatment of Thoraco-lumbar Spine Fracture
- Simple and Economical Method to Create Thoracolumbar Burst Fracture in a Calf Spine Model