J Korean Soc Spine Surg.
2008 Dec;15(4):257-264. 10.4184/jkss.2008.15.4.257.
Entry Point and Approaching Angle of Working Cannula in Endoscopic Lumbar Disecectomy
- Affiliations
-
- 1Department of Orthopedic Surgery, National Police Hospital, Seoul, Korea. bky@nph.go.kr
- KMID: 2209629
- DOI: http://doi.org/10.4184/jkss.2008.15.4.257
Abstract
- STUDY DESIGN: A retrospective study.
OBJECTIVES
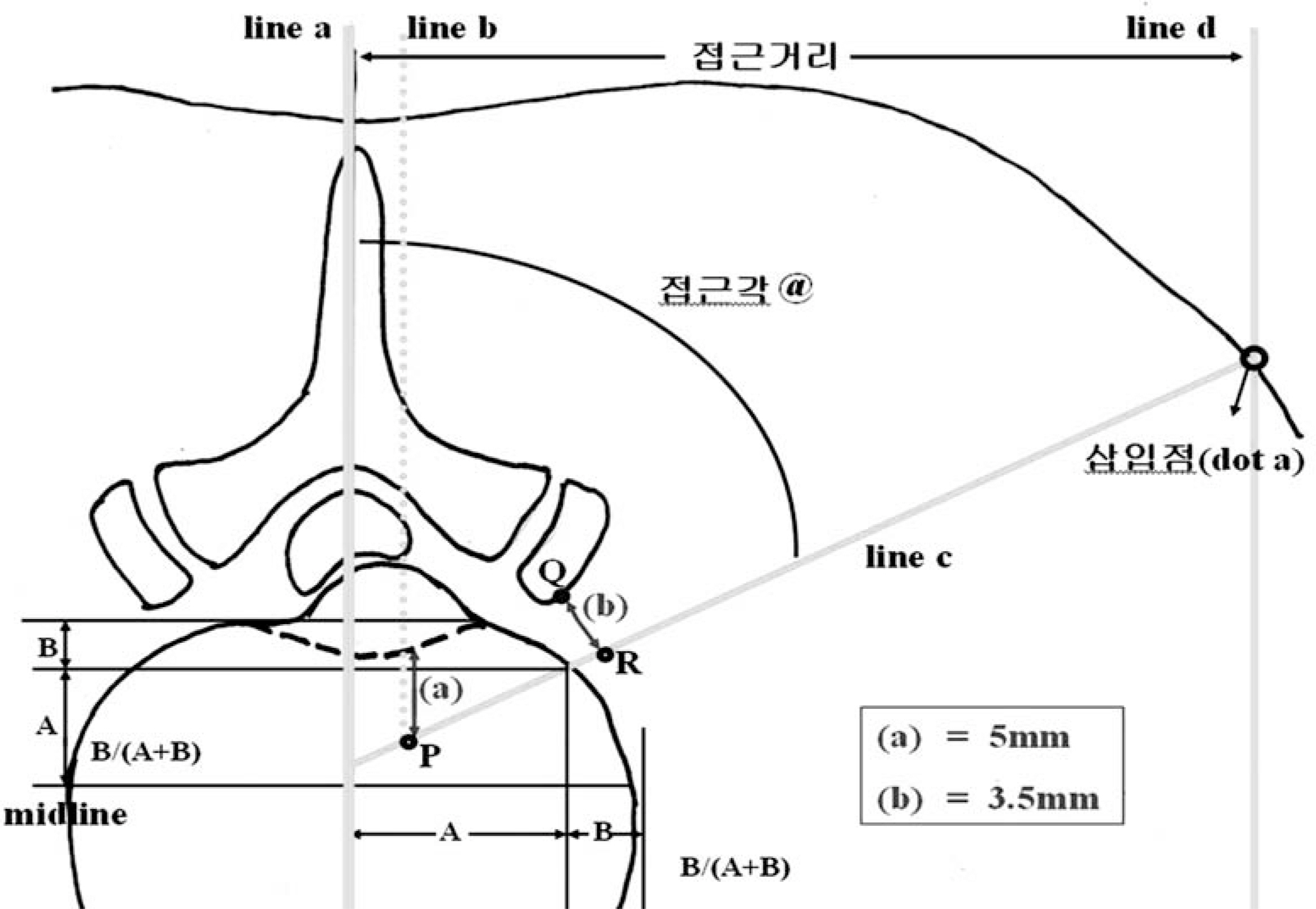
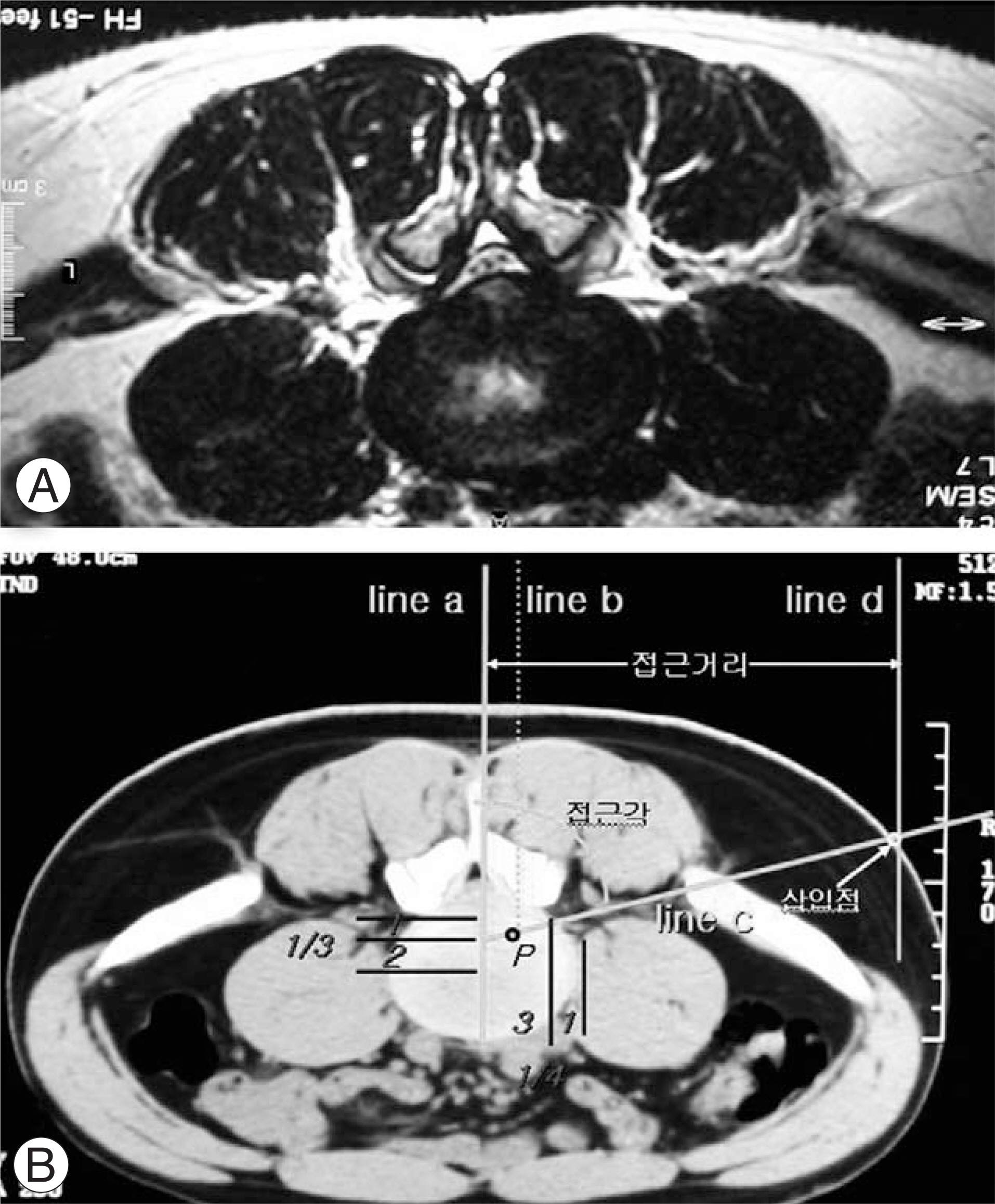
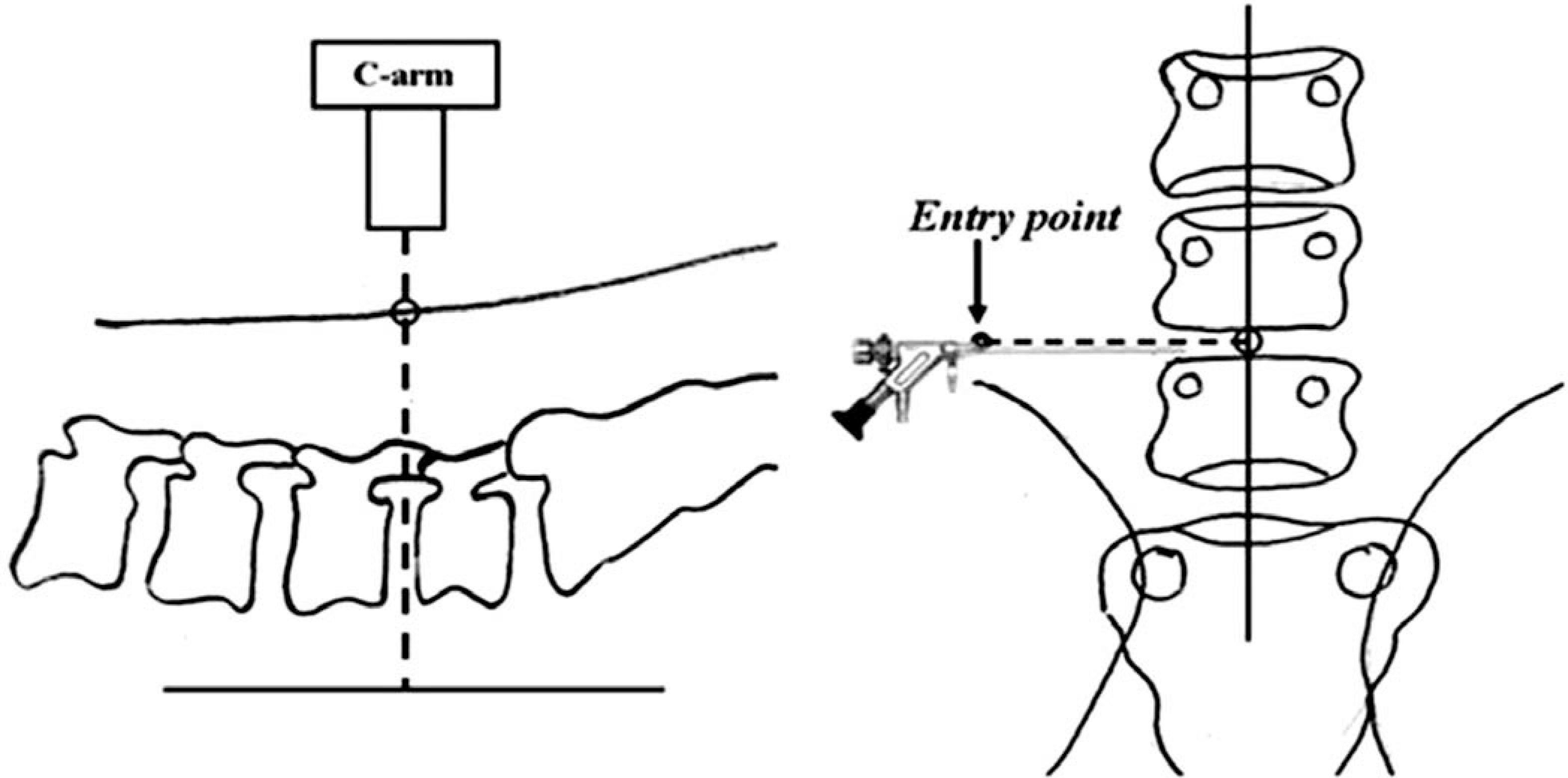
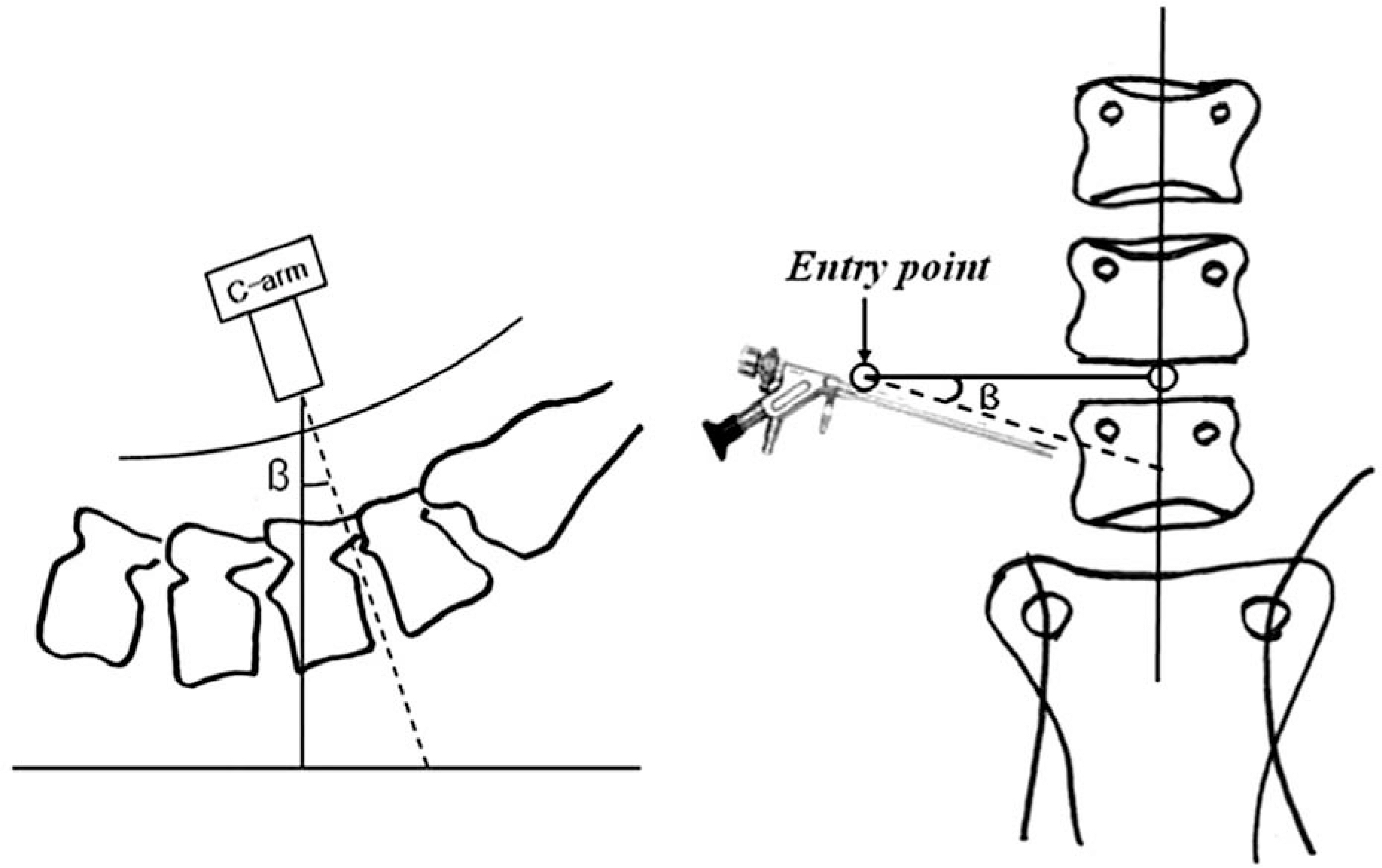
We report the efficacy of the entry point and approach angle of a working cannula using preoperative prone abdominal computer tomography (PACT). SUMMARY OF LITERATURE REVIEW: To date, there are no reports on the entry point and approach angle of a working cannula when performing transforaminal percutaneous endoscopic lumbar discectomy (TPELD) with consideration of the individual anatomic variations and characteristics of herniated disc and surgical instruments.
MATERIALS AND METHODS
Cases of herniated intervertebral discs from L4-5, who have previously undergone PACT before TPELD, were included. A total of 25 patients were observed over a 1 year period. The entry point and approaching angle of the working cannula with PACT were calculated, and the results were applied to the TPELD. The clinical results were assessed 1 month after surgery using the VAS, ODI and MacNab criteria, and were confirmed by a radiology and MRI examination.
RESULTS
The preoperative measured data using PACT showed that the mean approaching distance and mean approaching angle of the working cannula were 12.4 cm and 75.4 degree, respectively. The VAS improved from a mean of 8.1 preoperatively to a mean of 2.3 12 months after surgery. The ODI improved from a mean of 59 preoperatively to a mean of 24 at 12 months after surgery. According to the MacNab criteria, all patients were classified as either excellent and good during the follow up periods. The extruded disc of all patients had been well removed according to the MRI scan performed 1 month after surgery.
CONCLUSIONS
The scientific approach method using PACT based on the characteristics of patients and surgical instruments can be performed easily and accurately, and access and decompress the extruded disc directly.
Keyword
MeSH Terms
Figure
Reference
-
01). Hijikata S., Yamagishi M., Nakayama T., Oomori K. Percutaneous nuclectomy: A new treatment method for lumbar disc herniation. J. Tokyo Den-ryoku Hosp. 1975. 5:39–44.02). Hijikata S. Percutaneous nucleotomy: A new concept technique and 12 years experience. Clin Orthop Relat Res. 1989. 238:9–23.03). Mathews HH. Transforaminal endoscopic microdiscectomy. Neurosurg Clin N Am. 1996. 7:59–63.
Article04). Mayer HM. Spine update. Percutaneous lumbar disc surgery. Spine. 1994. 19:2719–2723.05). Stucker R. The transforaminal endoscopic approach. In Mayer HM (ed). Minimally invasive spinal surgery. Berlin: Springer-Verlag;2000. p. 202–205.06). Yeung AT., Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complication in 307 consecutive cases. Spine. 2002. 27:722–731.07). Ruetten S., Komp M., Godolias G. An extreme lateral access for the surgery of lumbar disc herniations inside the spinal canal using the full-endoscopic uniportal transforaminal approach-Technique and prospective results of 463 patients. Spine. 2005. 30:2570–2578.
Article08). Kambin P., Gellman H. Percutaneous lateral discectomy of the lumbar spine: A preliminary report. Clin Orthop Relat Res. 1983. 174:127–132.09). Mayer HM., Brock M. Percutaneous endoscopic discectomy: surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg. 1993. 78:216–225.
Article10). Yeung AT. The evolution of percutaneous spinal endoscopy and discectomy: state of the art. Mt Sinai J Med. 2000. 67:327–332.11). Yeung AT., Yeung CA. Advances in endoscopic disc and spine surgery: foraminal approach. Surg Tech Int. 2003. 11:255–263.12). Kambin P., Savitz MH. Arthroscopic microdiscectomy: An alternative to open disc surgery. Mt Sinai J Med. 2000. 67:283–287.13). Schreiber A., Suezawa Y., Leu H. Does percutaneous nucleotomy with discoscopy replace conventional discectomy? Eight years of experience and results in treatment of herniated lumbar disc. Clin Orthop Relat Res. 1989. 238:35–42.14). Yeung AT., Yeung CA. In-vivo endoscopic visualization of patho-anatomy in painful degenerative conditions of the lumbar spine. Surg Technol Int. 2006. 15:243–256.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Determination of Adequate Entry Angle of Lumbar Sympathetic Ganglion Block in Korean
- Percutaneous Endoscopic Discectomy for Lumbar Disc Herniation
- Safe Approaching Angle and Distance in Percutaneous Endoscopic Discectomy
- What Is the Ideal Entry Point for Transforaminal Endoscopic Lumbar Discectomy?
- Radiological Analysis of the Triangular Working Zone during Transforaminal Endoscopic Lumbar Discectomy