J Korean Soc Radiol.
2016 Apr;74(4):236-244. 10.3348/jksr.2016.74.4.236.
Embolization of Trauma-Associated Pelvic Hemorrhage: Feasibility of Super-Selective Catheterization in Heavily Injured Patients as a Damage Control for Life-Threatening Pelvic Bleeding
- Affiliations
-
- 1Department of Radiology, Chonnam National University Hospital, Gwangju, Korea. apleseed@chonnam.ac.kr
- KMID: 2208781
- DOI: http://doi.org/10.3348/jksr.2016.74.4.236
Abstract
- PURPOSE
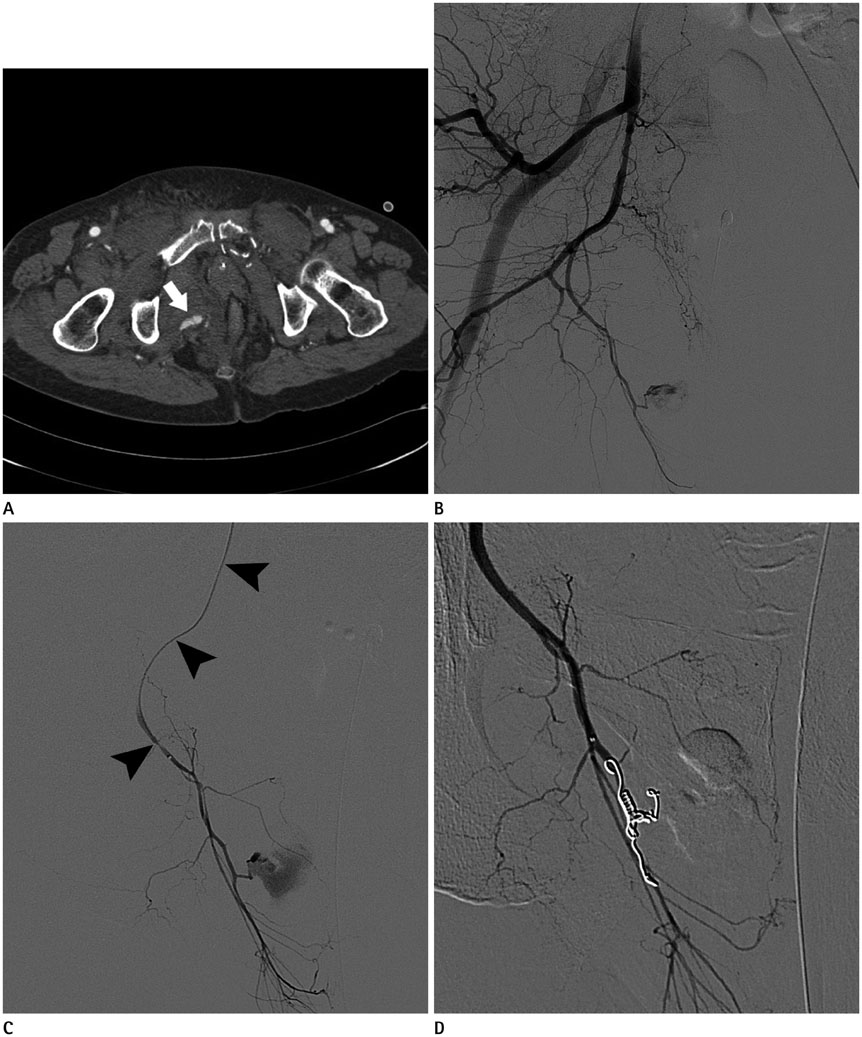
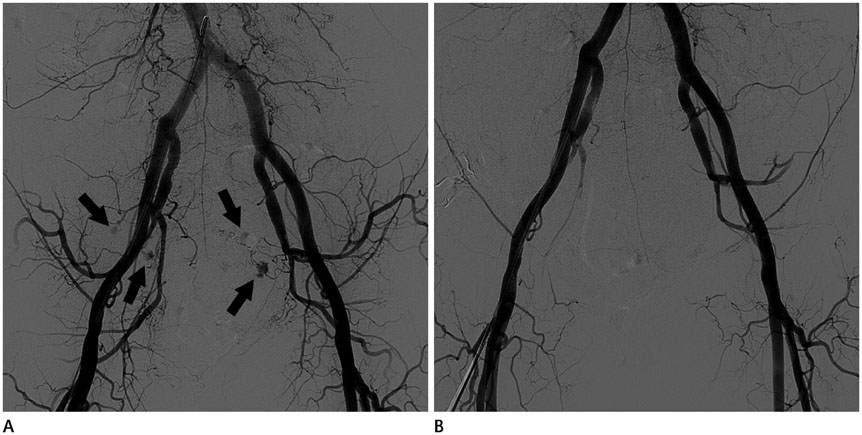
To determine the efficacy of embolization with super-selective catheterization of the internal iliac arterial branches to treat heavily injured trauma patients with pelvic arterial bleeding.
MATERIALS AND METHODS
A retrospective analysis was performed using the medical records of 37 patients who underwent trans-arterial embolization for trauma-associated pelvic arterial hemorrhage in a regional trauma center between July 2010 and July 2013. In each patient, hemodynamic stability, embolization level, elapsed time for trans-arterial embolization, clinical outcome and embolization-related complications were evaluated. Comparison of elapsed time, and presence of complication was done according to embolization level.
RESULTS
Transarterial embolization was conducted in 37 patients. Hemodynamic stability of each patient was classified into hemodynamic stable (n = 9), and unstable (n = 28). Twenty-nine of 37 patients underwent embolization after super-selective catheterization of more than 2nd order branch of internal iliac artery with a microcatheter, and 8 patients underwent proximal internal iliac artery embolization without super-selective catheterization. The mean elapsed procedure time for super-selective embolization (34.76 ± 20.0 minutes) was not significantly longer than proximal internal iliac artery embolization (33.87 ± 16.73 minutes, p = 0.215).
CONCLUSION
Pelvic arterial embolization with super-selective catheterization is a safe and feasible treatment for heavily injured patients with trauma-associated pelvic arterial bleeding.
MeSH Terms
Figure
Cited by 1 articles
-
Transcatheter Arterial Embolization for Acute Arterial Extravasation with Hematoma Formation: Classified the Group as Cause and Their Clinical Outcomes
Boram Kim, Young Min Han, Gong Yong Jin
J Korean Soc Radiol. 2018;78(2):120-129. doi: 10.3348/jksr.2018.78.2.120.
Reference
-
1. Bize PE, Duran R, Madoff DC, Golliet-Mercier N, Heim C, Pilleul F, et al. Embolization for multicompartmental bleeding in patients in hemodynamically unstable condition: prognostic factors and outcome. J Vasc Interv Radiol. 2012; 23:751–760.e4.2. Suzuki T, Smith WR, Moore EE. Pelvic packing or angiography: competitive or complementary? Injury. 2009; 40:343–353.3. Marzi I, Lustenberger T. Management of Bleeding Pelvic Fractures. Scand J Surg. 2014; 103:104–111.4. Fu CY, Wang YC, Wu SC, Chen RJ, Hsieh CH, Huang HC, et al. Angioembolization provides benefits in patients with concomitant unstable pelvic fracture and unstable hemodynamics. Am J Emerg Med. 2012; 30:207–213.5. Cullinane DC, Schiller HJ, Zielinski MD, Bilaniuk JW, Collier BR, Como J, et al. Eastern Association for the Surgery of Trauma practice management guidelines for hemorrhage in pelvic fracture--update and systematic review. J Trauma. 2011; 71:1850–1868.6. Frevert S, Dahl B, Lönn L. Update on the roles of angiography and embolisation in pelvic fracture. Injury. 2008; 39:1290–1294.7. Suzuki T, Kataoka Y, Minehara H, Nakamura K, Uchino M, Kawai K, et al. Transcatheter arterial embolization for pelvic fractures may potentially cause a triad of sequela: gluteal necrosis, rectal necrosis, and lower limb paresis. J Trauma. 2008; 65:1547–1550.8. Takahira N, Shindo M, Tanaka K, Nishimaki H, Ohwada T, Itoman M. Gluteal muscle necrosis following transcatheter angiographic embolisation for retroperitoneal haemorrhage associated with pelvic fracture. Injury. 2001; 32:27–32.9. Perez JV, Hughes TM, Bowers K. Angiographic embolisation in pelvic fracture. Injury. 1998; 29:187–191.10. Suzuki T, Shindo M, Kataoka Y, Kobayashi I, Nishimaki H, Yamamoto S, et al. Clinical characteristics of pelvic fracture patients with gluteal necrosis resulting from transcatheter arterial embolization. Arch Orthop Trauma Surg. 2005; 125:448–452.11. Gilleard O, Stammers J, Ali F. Gluteal necrosis following pelvic fracture and bilateral internal iliac embolization: reconstruction using a transposition flap based on the lumbar artery perforators. Int J Surg Case Rep. 2012; 3:86–88.12. Matityahu A, Marmor M, Elson JK, Lieber C, Rogalski G, Lin C, et al. Acute complications of patients with pelvic fractures after pelvic angiographic embolization. Clin Orthop Relat Res. 2013; 471:2906–2911.13. Yasumura K, Ikegami K, Kamohara T, Nohara Y. High incidence of ischemic necrosis of the gluteal muscle after transcatheter angiographic embolization for severe pelvic fracture. J Trauma. 2005; 58:985–990.14. Moore FA, Davis JW, Moore EE Jr, Cocanour CS, West MA, McIntyre RC Jr. Western Trauma Association (WTA) critical decisions in trauma: management of adult blunt splenic trauma. J Trauma. 2008; 65:1007–1011.15. Moore FA, McKinley BA, Moore EE, Nathens AB, West M, Shapiro MB, et al. Inflammation and the Host Response to Injury, a large-scale collaborative project: patient-oriented research core--standard operating procedures for clinical care. III. Guidelines for shock resuscitation. J Trauma. 2006; 61:82–89.16. Tanizaki S, Maeda S, Hayashi H, Matano H, Ishida H, Yoshikawa J, et al. Early embolization without external fixation in pelvic trauma. Am J Emerg Med. 2012; 30:342–346.17. Velmahos GC, Toutouzas KG, Vassiliu P, Sarkisyan G, Chan LS, Hanks SH, et al. A prospective study on the safety and efficacy of angiographic embolization for pelvic and visceral injuries. J Trauma. 2002; 53:303–308. discussion 30818. Pinto A, Niola R, Tortora G, Ponticiello G, Russo G, Di Nuzzo L, et al. Role of multidetector-row CT in assessing the source of arterial haemorrhage in patients with pelvic vascular trauma. Comparison with angiography. Radiol Med. 2010; 115:648–667.19. Nicholson AA. Vascular radiology in trauma. Cardiovasc Intervent Radiol. 2004; 27:105–120.20. Salazar GM, Walker TG. Evaluation and management of acute vascular trauma. Tech Vasc Interv Radiol. 2009; 12:102–116.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Interventional Management for Pelvic Trauma
- Preperitoneal Pelvic Packing Prior to Pelvic Angiography in Patients with Hemodynamic Instability due to Severe Pelvic Fracture: Two Cases
- Treatment of Ongoing Bleeding after a Damage Control Laparotomy for a Pelvic Bone Fracture: Arterial Embolization: A Case Report
- External iliac artery injury with posterior pelvic ring injury in Korea: a report of two cases
- Correlation between Young and Burgess Classification and Transcatheter Angiographic Embolization in Severe Trauma Patients