J Korean Soc Transplant.
2012 Dec;26(4):261-268. 10.4285/jkstn.2012.26.4.261.
A Single Center Experience of ABO Incompatible Kidney Transplantation
- Affiliations
-
- 1Department of Surgery, Maryknoll Medical Center, Busan, Korea. mkhjeong@hotmail.com
- 2Division of Nephrology, Department of Medicine, Maryknoll Medical Center, Busan, Korea.
- 3Department of Laboratory Medicine, Maryknoll Medical Center, Busan, Korea.
- KMID: 2202429
- DOI: http://doi.org/10.4285/jkstn.2012.26.4.261
Abstract
- BACKGROUND
Kidney transplantation (KT) is the optimal treatment for end stage renal disease. However, the relative shortage of organs for transplantation (from human leukocyte antigen- or ABO incompatible [ABOi] living donors) has led to ABOi KT as an accepted method to expand the pool of living kidney donors. To date, reports of the outcomes of ABOi KT are limited; therefore this study aims to evaluate the outcomes of ABOi KT in recipients.
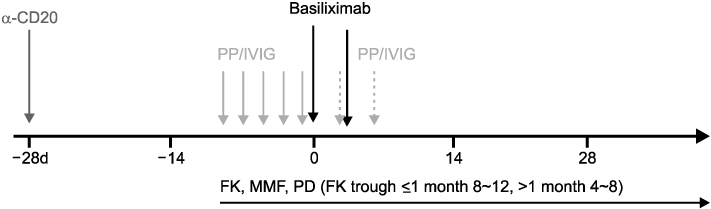
METHODS
We identified 45 patients who underwent live-donor ABOi KT between February 2007 and November 2011 at Maryknoll Medical Center. All of them were treated according to the scheduled protocol of plasmapheresis with low dose intravenous immunoglobulin, and low dose rituximab- or tacrolimus-based triple immunosuppressant regimens. Clinical parameters and the incidence of rejections in these patients were analyzed.
RESULTS
We had three cases (6.6%) of biopsy-proven acute antibody-mediated rejections and one case (2.2%) of acute cellular rejection, all of which were successfully treated. The median follow-up duration was 20 months (range, 2~59). Antibody depletion was scheduled according to baseline anti-ABO antibody titer (tube method: median immunoglobulin G titer/immunoglobulin M titer 64 [range, 8~4,096]/16 [range, 2~256], respectively). Although there was no patient death, one patient lost his graft due to nonadherence to immunosuppressants.
CONCLUSIONS
Our analysis of ABOi KT has shown excellent and promising outcomes. These practices may therefore represent an acceptable option for expanding the pool of living kidney donors.
MeSH Terms
Figure
Cited by 1 articles
-
Standardization of ABO Antibody Titer Measurement at Laboratories in Korea
Young Ae Lim, Seon Joo Kang
Ann Lab Med. 2014;34(6):456-462. doi: 10.3343/alm.2014.34.6.456.
Reference
-
1. Korean Network for Organ Sharing (KONOS). Annual report of the transplant [Internet]. 2011. cited 2011 Dec 6. Seoul: KONOS;Available from: http://www.konos.go.kr/konosis/common/bizlogic.jsp.2. Hume DM, Merrill JP, Miller BF, Thorn GW. Experiences with renal homotransplantation in the human: report of nine cases. J Clin Invest. 1955. 34:327–382.
Article3. Alexandre GP, Squifflet JP, Debruyere M, Latinne D, Moriau M, Ikabu N, et al. Splenectomy as a prerequisite for successful human ABO-incompatible renal-transplantation. Transplant Proc. 1985. 17:138–143.4. Ichimaru N, Takahara S. Japan's experience with living-donor kidney transplantation across ABO barriers. Nat Clin Pract Nephrol. 2008. 4:682–692.
Article5. Tydén G, Kumlien G, Fehrman I. Successful ABO-incompatible kidney transplantations without splenectomy using antigen-specific immunoadsorption and rituximab. Transplantation. 2003. 76:730–731.
Article6. Tanabe K, Takahashi K, Sonda K, Tokumoto T, Ishikawa N, Kawai T, et al. Long-term results of ABO-incompatible living kidney transplantation: a single-center experience. Transplantation. 1998. 65:224–228.
Article7. Nelson PW, Helling TS, Shield CF, Beck M, Bryan CF. Current experience with renal transplantation across the ABO barrier. Am J Surg. 1992. 164:541–544.
Article8. Tanabe K, Ishida H, Shimizu T, Omoto K, Shirakawa H, Tokumoto T. Evaluation of two different preconditioning regimens for ABO-incompatible living kidney donor transplantation. A comparison of splenectomy vs. rituximab-treated non-splenectomy preconditioning regimens. Contrib Nephrol. 2009. 162:61–74.9. Kong JM, Lee DR, Jeong JH, Choi JH, Lee JO, Lee WR, et al. ABO blood group incompatible living donor kidney transplantation without splenectomy. J Korean Soc Transplant. 2009. 23:71–76.10. Shirakawa H, Ishida H, Shimizu T, Omoto K, Iida S, Toki D, et al. The low dose of rituximab in ABO-incompatible kidney transplantation without a splenectomy: a single-center experience. Clin Transplant. 2011. 25:878–884.
Article11. Toki D, Ishida H, Horita S, Setoguchi K, Yamaguchi Y, Tanabe K. Impact of low-dose rituximab on splenic B cells in ABO-incompatible renal transplant recipients. Transpl Int. 2009. 22:447–454.
Article12. Walsh RC, Everly JJ, Brailey P, Rike AH, Arend LJ, Mogilishetty G, et al. Proteasome inhibitor-based primary therapy for antibody-mediated renal allograft rejection. Transplantation. 2010. 89:277–284.
Article13. Locke JE, Magro CM, Singer AL, Segev DL, Haas M, Hillel AT, et al. The use of antibody to complement protein C5 for salvage treatment of severe antibody-mediated rejection. Am J Transplant. 2009. 9:231–235.
Article14. Yang J. ABO incompatible kidney transplantation. Korean J Nephrol. 2011. 30:355–358.15. Reinsmoen NL, Lai CH, Vo A, Cao K, Ong G, Naim M, et al. Acceptable donor-specific antibody levels allowing for successful deceased and living donor kidney transplantation after desensitization therapy. Transplantation. 2008. 86:820–825.
Article16. Toki D, Ishida H, Setoguchi K, Shimizu T, Omoto K, Shirakawa H, et al. Acute antibody-mediated rejection in living ABO-incompatible kidney transplantation: long-term impact and risk factors. Am J Transplant. 2009. 9:567–577.
Article17. Tanabe K. Interinstitutional variation in the measurement of anti-A/B antibodies: the Japanese ABO-Incompatible Transplantation Committee survey. Transplantation. 2007. 84:12 Suppl. S13–S16.
Article18. Kang MG, Lee SJ, Oh JS, Lim YA. Comparison of ABO isoagglutinin titers by different tube hemagglutination techniques. Korean J Blood Transfus. 2009. 20:227–234.19. Ellis D, Shapiro R, Jordan ML, Scantlebury VP, Gilboa N, Hopp L, et al. Comparison of FK-506 and cyclosporine regimens in pediatric renal transplantation. Pediatr Nephrol. 1994. 8:193–200.
Article20. Cacciarelli TV, Green M, Jaffe R, Mazariegos GV, Jain A, Fung JJ, et al. Management of posttransplant lymphoproliferative disease in pediatric liver transplant recipients receiving primary tacrolimus (FK506) therapy. Transplantation. 1998. 66:1047–1052.
Article21. Kim JS. Tacrolimus versus cyclosporine immunosuppression in pediatric renal transplantation: pharmacokinetic consideration. Korean J Pediatr. 2005. 48:476–480.22. Vidhun JR, Sarwal MM. Corticosteroid avoidance in pediatric renal transplantation. Pediatr Nephrol. 2005. 20:418–426.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- ABO-Incompatible Kidney Transplantation
- Analysis of the Results of ABO-Incompatible Kidney Transplantation: In Comparison with ABO-Compatible Kidney Transplantation
- Successful Pediatric ABO-Incompatible Kidney Transplantation without Pretransplant Plasmapheresis: Report of a Case
- An Experience of ABO-incompatible Kidney Transplantation Using Plasmapheresis and Anti-CD20 Monoclonal Antibody
- Case of ABO-Incompatible Living Donor Kidney Transplantation without Blood Products in a Jehovah's Witness