J Lipid Atheroscler.
2012 Jun;1(1):21-28. 10.12997/jla.2012.1.1.21.
Effect of Statins on C-reactive Protein, Lipoprotein(a) and Fibrinogen in Hypercholesterolemic Patients
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, College of Medicine, Chung-Ang University, Seoul, Korea. cjkim@cau.ac.kr
- KMID: 2198372
- DOI: http://doi.org/10.12997/jla.2012.1.1.21
Abstract
OBJECTIVE
C-reactive protein (CRP), lipoprotein (a)[Lp(a)], and fibrinogen are associated with systemic inflammatory reactions. Statins have anti-inflammatory effects. However, the effect of statins on these parameters is inconsistent. We evaluated the effect of statins on inflammatory markers and variables related to changes in these markers.
METHODS
A total of 390 hypercholesterolemic patients were enrolled. Atorvastatin (n=112), lovastatin (n=25), pitavastatin (n=49), rosuvastatin (n=20), and simvastatin (n=184) were administered. Lipids, CRP, Lp(a), and fibrinogen levels were measured before and after 2 months of the therapy.
RESULTS
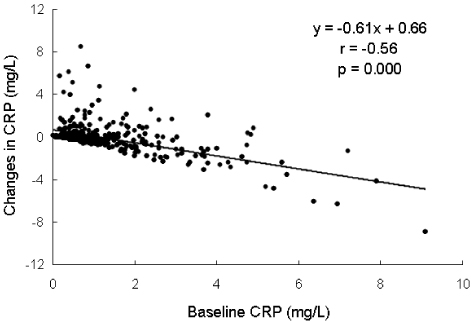
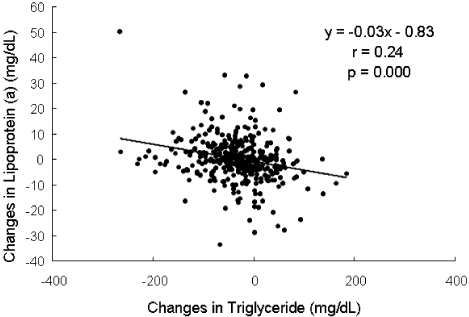
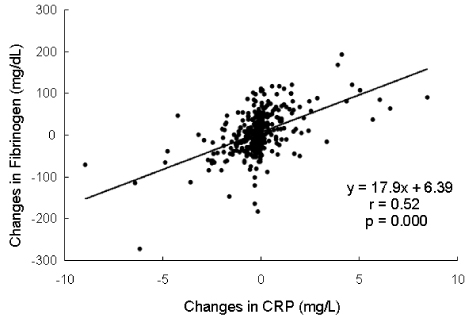
Statins reduced cholesterol, low density lipoprotein (LDL) cholesterol, and triglyceride levels by -28.9+/-9.1% (P=0.000), -41.4+/-12.4% (P=0.000), and -11.6+/-39.4% (P=0.000), respectively and increased high density lipoprotein (HDL) cholesterol level by 2.56+/-13.2% (P=0.014). CRP levels decreased from 1.23+/-1.30 to 1.14+/-1.29 mg/L (P=0.000). Lp(a) levels were not changed (P=0.91) and fibrinogen levels increased from 277.8+/-54.4 to 282.6+/-56.9 mg/dL (P=0.042). Changes in CRP levels were associated with baseline CRP levels (r=-0.56, P=0.000) and changes in HDL cholesterol levels (r=-0.14, P=0.005). Changes in Lp(a) levels were associated with changes in triglyceride (r=-0.24, P=0.000) and baseline aspartate aminotransferase level (r=0.12, P=0.015). Changes in fibrinogen levels were associated with baseline fibrinogen levels (r=-0.40, P=0.000), sex (r=0.18, P=0.001), and changes in HDL cholesterol levels (r=-0.15, P=0.003).
CONCLUSION
Inflammatory markers showed different responses to statins and changes in these markers were associated with different parameters. This finding suggests that anti-inflammatory effect of statin is confined to a specific pathway of inflammation.
Keyword
MeSH Terms
-
Aspartate Aminotransferases
C-Reactive Protein
Cholesterol
Cholesterol, HDL
Fibrinogen
Fluorobenzenes
Heptanoic Acids
Humans
Hydroxymethylglutaryl-CoA Reductase Inhibitors
Inflammation
Lipoprotein(a)
Lipoproteins
Lovastatin
Pyrimidines
Pyrroles
Quinolines
Simvastatin
Sulfonamides
Atorvastatin Calcium
Rosuvastatin Calcium
Aspartate Aminotransferases
C-Reactive Protein
Cholesterol
Cholesterol, HDL
Fibrinogen
Fluorobenzenes
Heptanoic Acids
Hydroxymethylglutaryl-CoA Reductase Inhibitors
Lipoprotein(a)
Lipoproteins
Lovastatin
Pyrimidines
Pyrroles
Quinolines
Simvastatin
Sulfonamides
Figure
Cited by 2 articles
-
Effect of Fenofibrate Therapy on Blood Creatinine Levels in Patients with Hypertension and Hypertriglyceridemia
Jun Hwan Cho, Young Hwan Choi, Cheol Won Hyeon, Kyung Joon Kim, Seonghyup Hyun, Jee Eun Kwon, Eun Young Kim, Wang-Soo Lee, Kwang Je Lee, Sang-Wook Kim, Tae Ho Kim, Chee Jeong Kim
J Lipid Atheroscler. 2013;2(1):19-26. doi: 10.12997/jla.2013.2.1.19.Cholesterol Lowering Effects of Low-dose Statins in Korean Patients
Jee Eun Kwon, Young Kim, Seonghyup Hyun, Hoyoun Won, Seung Yong Shin, Kwang Je Lee, Sang-Wook Kim, Tae Ho Kim, Chee Jeong Kim
J Lipid Atheroscler. 2014;3(1):21-28. doi: 10.12997/jla.2014.3.1.21.
Reference
-
1. Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, Kirby A, Sourjina T, Peto R, Collins R, Simes R. Cholesterol Treatment Trialists' (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005; 366:1267–1278.
Article2. Kim CJ, Lee KJ. Hypercholesterolemia; Management of Korean Patients in New Millennium. Korean J Med. 2007; 72:580–592.3. Forrester JS, Libby P. The inflammation hypothesis and its potential relevance to statin therapy. Am J Cardiol. 2007; 99:732–738.
Article4. Davignon J. Beneficial cardiovascular pleiotropic effects of statins. Circulation. 2004; 109:23 Suppl 1. III39–III43.
Article5. McFarlane SI, Muniyappa R, Francisco R, Sowers JR. Clinical review 145: Pleiotropic effects of statins: lipid reduction and beyond. J Clin Endocrinol Metab. 2002; 87:1451–1458.6. Ross R. Atherosclerosis an inflammatory disease. N Engl J Med. 1999; 340:115–126.7. Libby P. Current concepts of the pathogenesis of the acute coronary syndromes. Circulation. 2001; 104:365–372.
Article8. Kuller LH, Tracy RP, Shaten J, Meilahn EN. Relation of C-reactive protein and coronary heart disease in the MRFIT nested case-control study. Multiple Risk Factor Intervention Trial. Am J Epidemiol. 1996; 144:537–547.9. Ridker PM. Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation. 2003; 107:363–369.
Article10. Kaptoge S, Di Angelantonio E, Lowe G, Pepys MB, Thompson SG, Collins R, Danesh J. Emerging Risk Factors Collaboration. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet. 2010; 375:132–140.
Article11. Ridker PM, Rifai N, Pfeffer MA, Sacks F, Braunwald E. Long-term effects of pravastatin on plasma concentration of C-reactive protein. The Cholesterol and Recurrent Events (CARE) Investigators. Circulation. 1999; 100:230–235.
Article12. Albert MA, Danielson E, Rifai N, Ridker PM. PRINCE Investigators. Effect of statin therapy on C-reactive protein levels: the pravastatin inflammation/CRP evaluation (PRINCE): a randomized trial and cohort study. JAMA. 2001; 286:64–70.
Article13. Jung KS, Lee KE, Lee SH, Kim SJ, Lee KJ, Kim SW, Kim TH, Ko HS, Kim CJ, Ryu WS, Park AJ. Effect of hydroxymethyl glutaryl coenzyme A reductase inhibitor on high sensitivity C-reactive protein levels in hypercholesterolemic patients without atherosclerotic diseases. Korean Circ J. 2004; 34:381–387.
Article14. Fibrinogen Studies Collaboration. Plasma fibrinogen level and the risk of major cardiovascular diseases and nonvascular mortality: an individual participant meta-analysis. JAMA. 2005; 294:1799–1809.15. Kannel WB, D'Agostino RB, Belanger AJ. Update on fibrinogen as a cardiovascular risk factor. Ann Epidemiol. 1992; 2:457–466.
Article16. Beigel Y, Fuchs J, Snir M, Green P, Lurie Y, Djaldetti M. Lovastatin therapy in hypercholesterolemia: effect on fibrinogen, hemorrheologic parameters, platelet activity, and red blood cell morphology. J Clin Pharmacol. 1991; 31:512–517.
Article17. McDowell IF, Smye M, Trinick T, Shortt JA, Archibald MP, Trimble ER, Nicholls DP. Simvastatin in severe hypercholesterolaemia: a placebo controlled trial. Br J Clin Pharmacol. 1991; 31:340–343.
Article18. Mitropoulos KA, Armitage JM, Collins R, Meade TW, Reeves BE, Wallendszus KR, Wilson SS, Lawson A, Peto R. The Oxford Cholesterol Study Group. Randomized placebo-controlled study of the effects of simvastatin on haemostatic variables, lipoproteins and free fatty acids. Eur Heart J. 1997; 18:235–241.
Article19. Utermann G. The mysteries of lipoprotein(a). Science. 1989; 246:904–910.
Article20. Ridker PM, Hennekens CH, Stampfer MJ. A prospective study of lipoprotein(a) and the risk of myocardial infarction. JAMA. 1993; 270:2195–2199.
Article21. Kim CJ, Kwak MH, Kim KM, Ryu WS, Park CT, Ryoo UH. Lipoprotein(a) as a acute phase reactant. Korean J Lipidol. 1996; 6:111–115.22. Maeda S, Abe A, Seishima M, Makino K, Noma A, Kawade M. Transient changes of serum lipoprotein(a) as an acute phase protein. Atherosclerosis. 1989; 78:145–150.
Article23. Berg K, Leren TP. Unchanged serum lipoprotein(a) concentrations with lovastatin. Lancet. 1989; 2:812.24. Kostner GM, Gavish D, Leopold B, Bolzano K, Weintraub MS, Breslow JL. HMG CoA reductase inhibitors lower LDL cholesterol without reducing Lp(a) levels. Circulation. 1989; 80:1313–1319.
Article25. Ahn JH, Lee SY, Cho SW, Kim SM, Song YB, Lee KJ, Kim SW, Ko HS, Kim TH, Kim CJ, Ryu WS. Effect of long-term 3-hydroxy 3-methyl glutaryl CoA reductase inhibitor therapy on lipoprotein (a) concentration. Korean J Med. 2002; 63:283–289.26. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001; 285:2486–2497.27. Genest J. C-reactive protein: risk factor, biomarker and/or therapeutic target? Can J Cardiol. 2010; 26:41A–44A.
Article28. Kim CJ. Effects of fenofibrate on C-reactive protein levels in hypertriglyceridemic patients. J Cardiovasc Pharmacol. 2006; 47:758–763.
Article29. Navab M, Reddy ST, Van Lenten BJ, Fogelman AM. HDL and cardiovascular disease: atherogenic and atheroprotective mechanisms. Nat Rev Cardiol. 2011; 8:222–232.
Article30. Ko HS, Kim CJ, Ryu WS. Effect of fenofibrate on lipoprotein(a) in hypertriglyceridemic patients: impact of change in triglyceride level and liver function. J Cardiovasc Pharmacol. 2005; 46:405–411.31. Hahm KB, Kim WH, Han KH, Chon CY, Kang JK, Park IS, Choi HJ, Kim CJ, Kim HS, Paik SW, Kim EJ. Lipoprotein(a) in patients with various liver diseases. Korean J Gastroenterol. 1992; 24:275–283.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Ezetimibe Added to Ongoing Statin Therapy on C-Reactive Protein Levels in Hypercholesterolemic Patients
- The Relationship Between Fatigue and C-Reactive Protein in Epilepsy Patients
- Hypercholesterolemia; Management of Korean Patients in New Millennium
- High Sensitivity CRP, Fibrinogen and Homocysteine in Relation to Carotid Intima-media Thickness in Acute Ischemic Stroke
- Association among C-Reactive Protein, Pulse Pressure and Ischemic Heart Disease in Patients with Continuous Ambulatory Peritoneal Dialysis