J Lipid Atheroscler.
2014 Jun;3(1):43-48. 10.12997/jla.2014.3.1.43.
Acute Stent Thrombosis after Coronary Stenting in Patients with Acute Coronary Syndrome
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea.
- 2Division of Cardiology, Department of Internal Medicine, Seoul Boramae Medical Center, Seoul, Korea. shkimmd@snu.ac.kr
- 3Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2198360
- DOI: http://doi.org/10.12997/jla.2014.3.1.43
Abstract
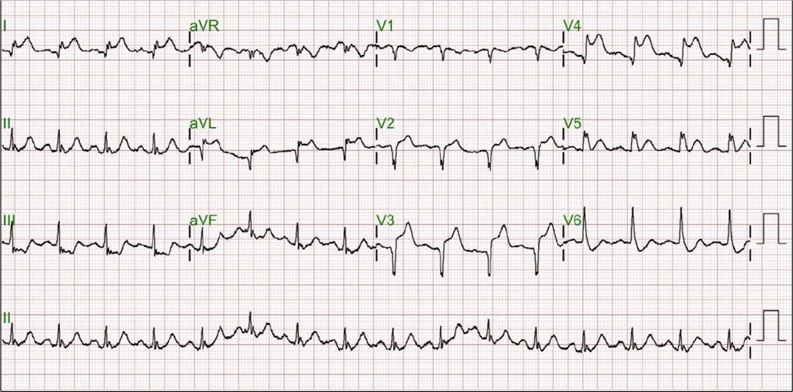
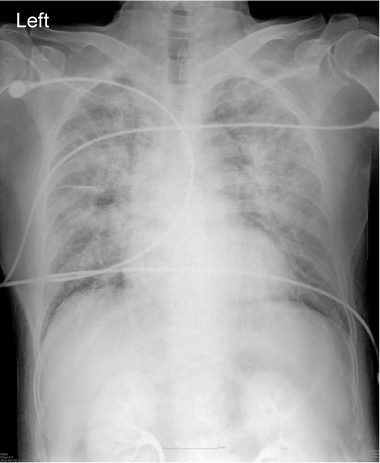
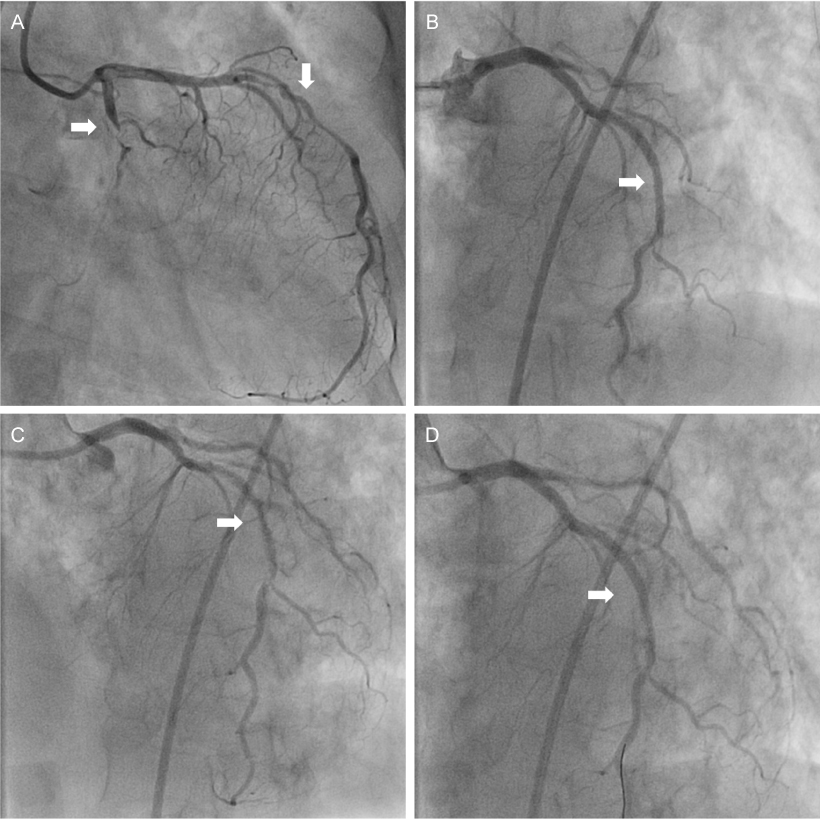
- Acute stent thrombosis after percutaneous coronary intervention (PCI) is still problematic because of the subsequent development of myocardial infarction and poor prognosis. The incidence of acute stent thrombosis, occurring within 0-24hours after PCI, is relatively low, but underlying causes and treatment strategy are not well defined. Multi-vessel disease, ST-elevated myocardial infarction (STEMI), and large thrombotic burden are known risk factors of acute stent thrombosis. Thrombus aspiration, balloon angioplasty and glycoprotein IIb/IIIa receptor blocker could be therapeutic options. Recently we experienced two cases of acute stent thrombosis which developed during PCI with the aggravation of chest pain, and acute stent thrombosis were diagnosed immediately and successfully treated. Here we report two cases of acute stent thrombosis during PCI for one patient with STEMI and the other with acute coronary syndrome, which were successfully treated with thrombus aspiration and intravenous infusion of glycoprotein IIb/IIIa receptor blocker.
MeSH Terms
Figure
Reference
-
1. Aoki J, Lansky AJ, Mehran R, Moses J, Bertrand ME, McLaurin BT, et al. Early stent thrombosis in patients with acute coronary syndromes treated with drug-eluting and bare metal stents: the Acute Catheterization and Urgent Intervention Triage Strategy trial. Circulation. 2009; 119(5):687–698.
Article2. Daemen J, Wenaweser P, Tsuchida K, Abrecht L, Vaina S, Morger C, et al. Early and late coronary stent thrombosis of sirolimus-eluting and paclitaxel-eluting stents in routine clinical practice: data from a large two-institutional cohort study. Lancet. 2007; 369(9562):667–678.
Article3. Stone GW, Moses JW, Ellis SG, Schofer J, Dawkins KD, Morice MC, et al. Safety and efficacy of sirolimus- and paclitaxel-eluting coronary stents. N Engl J Med. 2007; 356(10):998–1008.
Article4. Mauri L, Hsieh WH, Massaro JM, Ho KK, D'Agostino R, Cutlip DE. Stent thrombosis in randomized clinical trials of drug-eluting stents. N Engl J Med. 2007; 356(10):1020–1029.
Article5. Iakovou I, Schmidt T, Bonizzoni E, Ge L, Sangiorgi GM, Stankovic G, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005; 293(17):2126–2130.
Article6. Park SH, HongGR , Seo HS, Tahk SJ. Stent Thrombosis after Successful Drug-Eluting Stent Implantation. Korean Circ J. 2005; 35:163–171.
Article7. Park KW, Hwang SJ, Kwon DA, Oh BH, Park YB, Chae IH, et al. Characteristics and predictors of drug-eluting stent thrombosis: results from the multicenter 'Korea Stent Thrombosis (KoST)' registry. Circ J. 2011; 75(7):1626–1632.
Article8. Beinart R, Abu Sham'a R, Segev A, Hod H, Guetta V, Shechter M, et al. The incidence and clinical predictors of early stent thrombosis in patients with acute coronary syndrome. Am Heart J. 2010; 159(1):118–124.
Article9. Akhtar MM, Jones DA, Gallagher S, Weerackody R, Sammut E, et al. Thrombectomy and platelet glycoprotein IIB/IIIA blockade for stent thrombosis. Heart. 2012; 98:A2.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Simultaneous Multivessel Acute Stent Thrombosis in a Patient with Gastrointestinal Bleeding
- Acute Coronary Stent Thrombosis in Cancer Patients: A Case Series Report
- Very Late Stent Thrombosis in Coronary Bare-Metal Stent Implantation: A Case Report
- Subacute In-stent Thrombosis after Carotid Artery Stenting: A Case Report
- A Case of Recurrent Stent Thrombosis in a Patient with Essential Thrombocythemia