J Korean Med Assoc.
2013 Jan;56(1):7-15. 10.5124/jkma.2013.56.1.7.
Treatment of dysphagia in patients with brain disorders
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. tairyoon@snu.ac.kr
- KMID: 2192895
- DOI: http://doi.org/10.5124/jkma.2013.56.1.7
Abstract
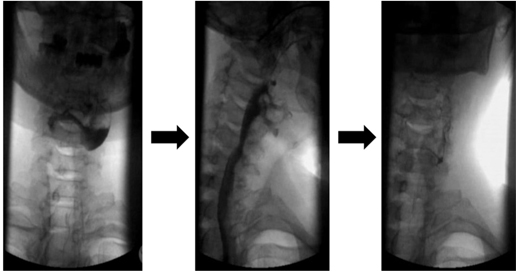
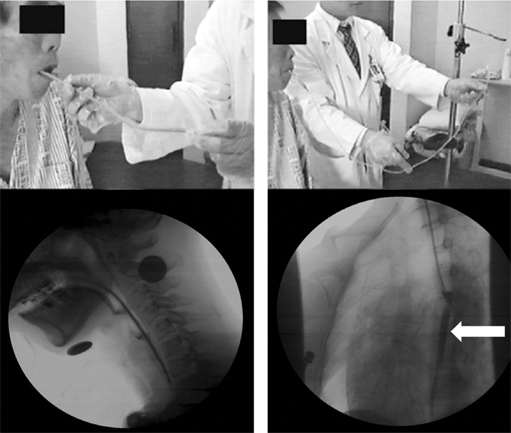
- Dysphagia is caused by various pathologic conditions of which brain disorders are the major etiology. If food materials enter an airway, aspiration pneumonia or serious asphyxia can develop, which necessitates early detection and proper management of dysphagia. Diagnosis of dysphagia includes history taking, physical examination, bedside screening tests, videofluoroscopic swallowing study (VFSS), and fiberoptic endoscopic examination of swallowing (FEES). Dysphagia management or rehabilitation consists of direct and indirect training methods. The direct one consists of modification of the texture and viscosity (using fluid thickener) of the diet, and diverse compensatory techniques for posture change (chin tuck, head rotation, and head tilt), airway protection (supraglottic swallowing and super-supraglottic swallowing) and improvement of bolus passage (effortful swallowing, multiple swallowing, Mendelsohn maneuver). Indirect training methods without using food are made up of thermal tactile stimulation, electrical stimulation of suprahyoid or infrahyoid muscles, repetitive transcranial magnetic stimulation, and strengthening of the tongue or pharyngeal muscles involved in swallowing (Shaker's exercise and vocal cord adduction exercise). Oral hygiene, adequate hydration, and nutritional support are also crucial. Although the prognosis of dysphagia is favorable with proper rehabilitation, enteral feeding through percutaneous endoscopic gastrostomy or an oroesophageal tube would be helpful to patients who have unresolved dysphagia for some time. Further large-scale clinical studies will be needed to establish evidence on various training methods for dysphagia management.
Keyword
MeSH Terms
-
Asphyxia
Brain
Brain Diseases
Deglutition
Deglutition Disorders
Diet
Electric Stimulation
Enteral Nutrition
Gastrostomy
Head
Humans
Mass Screening
Muscles
Nutritional Support
Oral Hygiene
Pharyngeal Muscles
Physical Examination
Pneumonia, Aspiration
Posture
Prognosis
Recovery of Function
Respiratory Aspiration
Tongue
Transcranial Magnetic Stimulation
Viscosity
Vocal Cords
Figure
Cited by 2 articles
-
Practical Assessment of Dysphagia in Stroke Patients
Kyoung Moo Lee, Hyo Jong Kim
Ann Rehabil Med. 2015;39(6):1018-1027. doi: 10.5535/arm.2015.39.6.1018.Effects of Head Rotation and Head Tilt on Pharyngeal Pressure Events Using High Resolution Manometry
Cheol Ki Kim, Ju Seok Ryu, Sun Hong Song, Jung Hoi Koo, Kyung Duck Lee, Hee Sun Park, Yoongul Oh, Kyunghoon Min
Ann Rehabil Med. 2015;39(3):425-431. doi: 10.5535/arm.2015.39.3.425.
Reference
-
1. Cook IJ, Dodds WJ, Dantas RO, Kern MK, Massey BT, Shaker R, Hogan WJ. Timing of videofluoroscopic, manometric events, and bolus transit during the oral and pharyngeal phases of swallowing. Dysphagia. 1989; 4:8–15.
Article2. Smithard DG, O'Neill PA, Parks C, Morris J. Complications and outcome after acute stroke. Does dysphagia matter? Stroke. 1996; 27:1200–1204.3. Leder SB. Gag reflex and dysphagia. Head Neck. 1996; 18:138–141.
Article4. Yoon K, Kim SB, Lee KW, Park SH. Clinical utility of the bedside swallowing evaluations for dysphagia. J Korean Acad Rehabil Med. 2003; 27:489–493.5. Teramoto S, Fukuchi Y. Detection of aspiration and swallowing disorder in older stroke patients: simple swallowing provocation test versus water swallowing test. Arch Phys Med Rehabil. 2000; 81:1517–1519.
Article6. Duncan PW, Zorowitz R, Bates B, Choi JY, Glasberg JJ, Graham GD, Katz RC, Lamberty K, Reker D. Management of adult stroke rehabilitation care: a clinical practice guideline. Stroke. 2005; 36:e100–e143.7. Kim JY, Koh ES, Kim HR, Chun SM, Lee SU, Jung SH. The diagnostic usefulness of the fiberoptic endoscopic evaluation of swallowing. J Korean Acad Rehabil Med. 2011; 35:14–22.8. Elmstahl S, Bulow M, Ekberg O, Petersson M, Tegner H. Treatment of dysphagia improves nutritional conditions in stroke patients. Dysphagia. 1999; 14:61–66.
Article9. Palmer JB, Drennan JC, Baba M. Evaluation and treatment of swallowing impairments. Am Fam Physician. 2000; 61:2453–2462.10. Han TR, Park JW, Park IC, Lee EK. Fluid and calory intake in patients with dysphagia. J Korean Acad Rehabil Med. 2002; 26:249–253.11. McCallum SL. The national dysphagia diet: implementation at a regional rehabilitation center and hospital system. J Am Diet Assoc. 2003; 103:381–384.
Article12. Paik NJ, Han TR, Park JW, Lee EK, Park MS, Hwang IK. Categorization of dysphagia diets with the line spread test. Arch Phys Med Rehabil. 2004; 85:857–861.13. Welch MV, Logemann JA, Rademaker AW, Kahrilas PJ. Changes in pharyngeal dimensions effected by chin tuck. Arch Phys Med Rehabil. 1993; 74:178–181.14. Baek SS, Park SB, Lee SG, Lee KM, Kim SH. The effect of neck posture in swallowing of stroke patients. J Korean Acad Rehabil Med. 1997; 21:8–12.15. Ohmae Y, Ogura M, Kitahara S, Karaho T, Inouye T. Effects of head rotation on pharyngeal function during normal swallow. Ann Otol Rhinol Laryngol. 1998; 107:344–348.
Article16. Bulow M, Olsson R, Ekberg O. Videomanometric analysis of supraglottic swallow, effortful swallow, and chin tuck in patients with pharyngeal dysfunction. Dysphagia. 2001; 16:190–195.
Article17. Hind JA, Nicosia MA, Roecker EB, Carnes ML, Robbins J. Comparison of effortful and noneffortful swallows in healthy middle-aged and older adults. Arch Phys Med Rehabil. 2001; 82:1661–1665.
Article18. Ding R, Larson CR, Logemann JA, Rademaker AW. Surface electromyographic and electroglottographic studies in normal subjects under two swallow conditions: normal and during the Mendelsohn manuever. Dysphagia. 2002; 17:1–12.
Article19. Shaker R, Easterling C, Kern M, Nitschke T, Massey B, Daniels S, Grande B, Kazandjian M, Dikeman K. Rehabilitation of swallowing by exercise in tube-fed patients with pharyngeal dysphagia secondary to abnormal UES opening. Gastroenterology. 2002; 122:1314–1321.
Article20. Crary MA, Carnaby-Mann GD, Faunce A. Electrical stimulation therapy for dysphagia: descriptive results of two surveys. Dysphagia. 2007; 22:165–173.
Article21. Yoon YS, Lim JT, Yun SB, Ohm BY, Kang JY, Lim HY, Chung BH, Kim JH. The effect of functional electrical stimulation on swallowing function in stroke patients with dysphagia. J Korean Acad Rehabil Med. 2006; 30:417–423.22. Kim DY, Koh ES, Kang BS, Han TR, Lee SU. Effects of electrical stimulation for dysphagia caused by stroke. J Korean Acad Rehabil Med. 2008; 32:9–14.23. Park YJ, Yang HS, Cha DY. Neuromuscular electrical stimulation therapy for patients with chronic dysphagia caused by stroke. J Korean Acad Rehabil Med. 2007; 31:636–641.24. Oh BM, Kim DY, Paik NJ. Recovery of swallowing function is accompanied by the expansion of the cortical map. Int J Neurosci. 2007; 117:1215–1227.
Article25. Khedr EM, Abo-Elfetoh N, Rothwell JC. Treatment of post-stroke dysphagia with repetitive transcranial magnetic stimulation. Acta Neurol Scand. 2009; 119:155–161.
Article26. Hamdy S, Jilani S, Price V, Parker C, Hall N, Power M. Modulation of human swallowing behaviour by thermal and chemical stimulation in health and after brain injury. Neurogastroenterol Motil. 2003; 15:69–77.
Article27. Han TR, Paik NJ, Park JW. The follow-up of oro-esophageal (OE) tube feeding. J Korean Acad Rehabil Med. 2001; 25:58–61.28. You DS, Chun MH, Kim HJ, Ryu JS, Song YJ, Park EJ, Choi KH. The effectiveness of oro-esophageal tube feeding with dysphagia after brainstem stroke. J Korean Acad Rehabil Med. 2011; 35:27–33.29. Suiter DM, McCullough GH, Powell PW. Effects of cuff deflation and one-way tracheostomy speaking valve placement on swallow physiology. Dysphagia. 2003; 18:284–292.
Article30. Smithard DG, O'Neill PA, England RE, Park CL, Wyatt R, Martin DF, Morris J. The natural history of dysphagia following a stroke. Dysphagia. 1997; 12:188–193.
Article