J Korean Neurosurg Soc.
2016 Mar;59(2):137-142. 10.3340/jkns.2016.59.2.137.
Early Bone Marrow Edema Pattern of the Osteoporotic Vertebral Compression Fracture : Can Be Predictor of Vertebral Deformity Types and Prognosis?
- Affiliations
-
- 1Department of Radiology, Graduate School, Kyung Hee University, Seoul, Korea.
- 2Department of Radiology, Kyung Hee University Hospital, Kyung Hee University School of Medicine, Seoul, Korea. t2star@naver.com
- 3Department of Radiology, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea.
- 4Department of Neurosurgery, Kyung Hee University Hospital, Kyung Hee University School of Medicine, Seoul, Korea.
- KMID: 2192043
- DOI: http://doi.org/10.3340/jkns.2016.59.2.137
Abstract
OBJECTIVE
To evaluate whether an early bone marrow edema pattern predicts vertebral deformity types and prognosis in osteoporotic vertebral compression fracture (OVCF).
METHODS
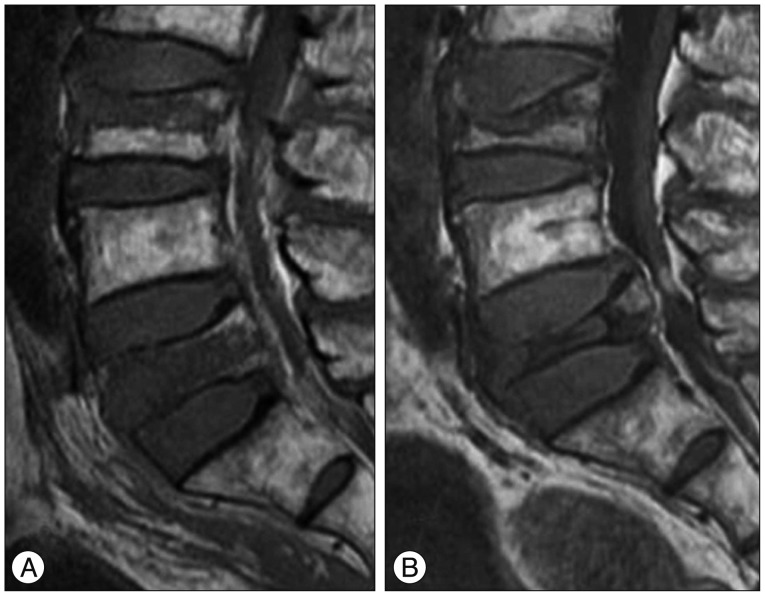
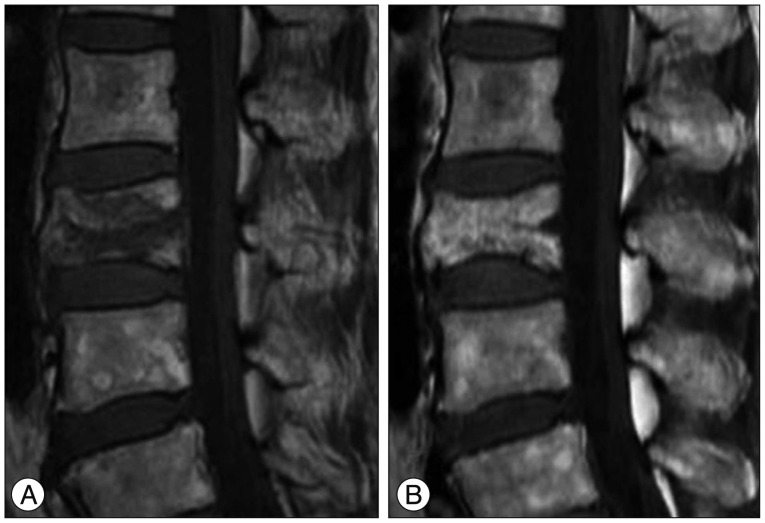
This retrospective study enrolled 64 patients with 75 acute OVCFs who underwent early MRI and followed up MRI. On early MRI, the low SI pattern of OVCF on T1WI were assessed and classified into 3 types (diffuse, globular or patchy, band-like). On followed up MRI, the vertebral deformity types (anterior wedge, biconcave, crush), degree of vertebral body height loss, incidence of vertebral osteonecrosis and spinal stenosis were assessed for each vertebral fracture types.
RESULTS
According to the early bone marrow edema pattern on T1WI, 26 vertebrae were type 1, 14 vertebrae were type 2 and 35 vertebrae were type 3. On followed up MRI, the crush-type vertebral deformity was most frequent among the type 1 OVCFs, the biconcave-type vertebral deformity was most frequent among the type 2 OVCFs and the anterior wedge-type vertebral deformity was most frequent among the type 3 OVCFs (p<0.001). In addition, type 1 early bone marrow edema pattern of OVCF on T1WI were associated with higher incidence of severe degree vertebral body height loss, vertebral osteonecrosis and spinal stenosis on the follow up MRI.
CONCLUSION
Early bone marrow edema pattern of OVCF on T1WI, significant correlated with vertebral deformity types on the follow up MRI. The severe degree of vertebral height loss, vertebral osteonecrosis, and spinal stenosis were more frequent in patients with diffuse low SI pattern.
MeSH Terms
Figure
Cited by 1 articles
-
Posttraumatic Delayed Vertebral Collapse : Kummell’s Disease
Jeongwook Lim, Seung-Won Choi, Jin-Young Youm, Hyon-Jo Kwon, Seon-Hwan Kim, Hyeon-Song Koh
J Korean Neurosurg Soc. 2018;61(1):1-9. doi: 10.3340/jkns.2017.0505.010.
Reference
-
1. Baker LL, Goodman SB, Perkash I, Lane B, Enzmann DR. Benign versus pathologic compression fractures of vertebral bodies : assessment with conventional spin-echo, chemical-shift, and STIR MR imaging. Radiology. 1990; 174:495–502. PMID: 2296658.
Article2. Baur A, Stäbler A, Arbogast S, Duerr HR, Bartl R, Reiser M. Acute osteoporotic and neoplastic vertebral compression fractures : fluid sign at MR imaging. Radiology. 2002; 225:730–735. PMID: 12461253.
Article3. Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009; 361:557–568. PMID: 19657121.
Article4. Ismail AA, Cooper C, Felsenberg D, Varlow J, Kanis JA, Silman AJ, et al. Number and type of vertebral deformities : epidemiological characteristics and relation to back pain and height loss. European Vertebral Osteoporosis Study Group. Osteoporos Int. 1999; 9:206–213. PMID: 10450408.
Article5. Jung HS, Jee WH, McCauley TR, Ha KY, Choi KH. Discrimination of metastatic from acute osteoporotic compression spinal fractures with MR imaging. Radiographics. 2003; 23:179–187. PMID: 12533652.
Article6. Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009; 361:569–579. PMID: 19657122.
Article7. Kanchiku T, Taguchi T, Kawai S. Magnetic resonance imaging diagnosis and new classification of the osteoporotic vertebral fracture. J Orthop Sci. 2003; 8:463–466. PMID: 12898295.
Article8. Kazawa N. T2WI MRI and MRI-MDCT correlations of the osteoporotic vertebral compressive fractures. Eur J Radiol. 2012; 81:1630–1636. PMID: 21636232.
Article9. Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J. 2006; 6:479–487. PMID: 16934715.
Article10. Lee HM, Park SY, Lee SH, Suh SW, Hong JY. Comparative analysis of clinical outcomes in patients with osteoporotic vertebral compression fractures (OVCFs) : conservative treatment versus balloon kyphoplasty. Spine J. 2012; 12:998–1005. PMID: 23026068.
Article11. Lee SG, Yoo CJ. Percutaneous vertebroplasty in the treatment of vertebral body compression fracture with osteoporosis : preliminary report. J Korean Neurosurg Soc. 2000; 29:615–622.12. Lenchik L, Rogers LF, Delmas PD, Genant HK. Diagnosis of osteoporotic vertebral fractures : importance of recognition and description by radiologists. AJR Am J Roentgenol. 2004; 183:949–958. PMID: 15385286.
Article13. Liu JT, Liao WJ, Tan WC, Lee JK, Liu CH, Chen YH, et al. Balloon kyphoplasty versus vertebroplasty for treatment of osteoporotic vertebral compression fracture : a prospective, comparative, and randomized clinical study. Osteoporos Int. 2010; 21:359–364. PMID: 19513578.
Article14. McKiernan F, Faciszewski T. Intravertebral clefts in osteoporotic vertebral compression fractures. Arthritis Rheum. 2003; 48:1414–1419. PMID: 12746915.
Article15. Mikles MR, Stchur RP, Graziano GP. Posterior instrumentation for thoracolumbar fractures. J Am Acad Orthop Surg. 2004; 12:424–435. PMID: 15615508.
Article16. Oner FC, van Gils AP, Dhert WJ, Verbout AJ. MRI findings of thoracolumbar spine fractures : a categorisation based on MRI examinations of 100 fractures. Skeletal Radiol. 1999; 28:433–443. PMID: 10486011.
Article17. Robinson Y, Olerud C. Vertebroplasty and kyphoplasty--a systematic review of cement augmentation techniques for osteoporotic vertebral compression fractures compared to standard medical therapy. Maturitas. 2012; 72:42–49. PMID: 22425141.
Article18. Ryu CW, Han H, Lee YM, Lim MK. The intravertebral cleft in benign vertebral compression fracture : the diagnostic performance of non-enhanced MRI and fat-suppressed contrast-enhanced MRI. Br J Radiol. 2009; 82:976–981. PMID: 19581311.
Article19. Ryu KN, Jin W, Ko YT, Yoon Y, Oh JH, Park YK, et al. Bone bruises : MR characteristics and histological correlation in the young pig. Clin Imaging. 2000; 24:371–380. PMID: 11368941.
Article20. Theodorou DJ. The intravertebral vacuum cleft sign. Radiology. 2001; 221:787–788. PMID: 11719679.
Article21. Venmans A, Klazen CA, Lohle PN, Mali WP, van Rooij WJ. Natural history of pain in patients with conservatively treated osteoporotic vertebral compression fractures : results from VERTOS II. AJNR Am J Neuroradiol. 2012; 33:519–521. PMID: 22116114.
Article22. Wiggins MC, Sehizadeh M, Pilgram TK, Gilula LA. Importance of intravertebral fracture clefts in vertebroplasty outcome. AJR Am J Roentgenol. 2007; 188:634–640. PMID: 17312047.
Article23. Yu CW, Hsu CY, Shih TT, Chen BB, Fu CJ. Vertebral osteonecrosis : MR imaging findings and related changes on adjacent levels. AJNR Am J Neuroradiol. 2007; 28:42–47. PMID: 17213422.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Influence of Vertebral Bone Marrow Edema on Outcome in Non-Acute Osteoporotic Patients Treated with Percutaneous Vertebroplasty
- Long Term Follow-up of Osteoporotic Vertebral Fractures According to the Morphologic Analysis of Fracture Pattern
- The Effect of Disc Degeneration in Osteoporotic Vertebral Fracture
- Association Between Osteoporotic Vertebral Fracture and Body Mass Index
- Risk Factors for Subsequent Fracture after Osteoporotic Vertebral Compression Fracture