J Korean Neurosurg Soc.
2015 Aug;58(2):150-154. 10.3340/jkns.2015.58.2.150.
Early Spontaneous Recanalization of Sigmoid Sinus Thrombosis Following a Closed Head Injury in a Pediatric Patient : A Case Report and Review of Literature
- Affiliations
-
- 1Department of Neurological Surgery, Dankook University College of Medicine, Cheonan, Korea. dkns0212@naver.com
- 2Department of Pediatrics, Dankook University College of Medicine, Cheonan, Korea.
- KMID: 2191326
- DOI: http://doi.org/10.3340/jkns.2015.58.2.150
Abstract
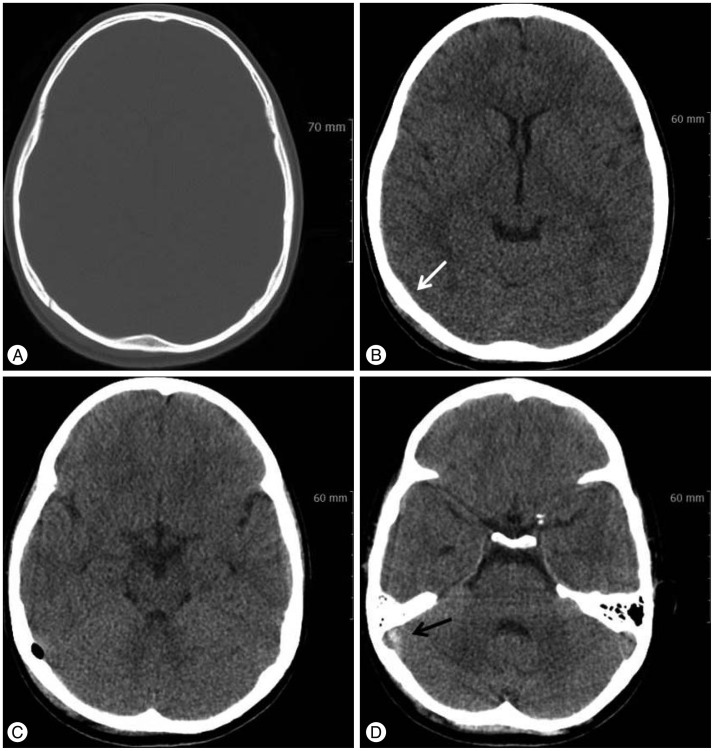
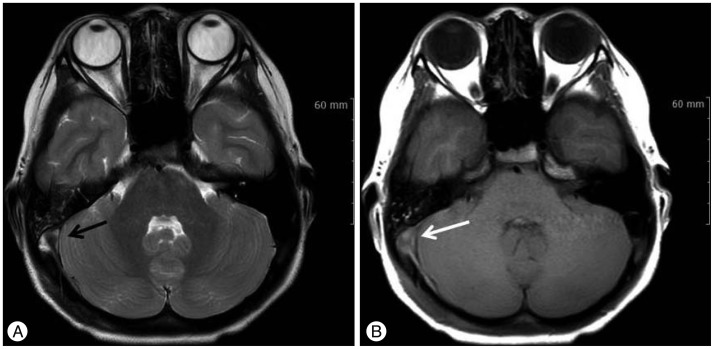
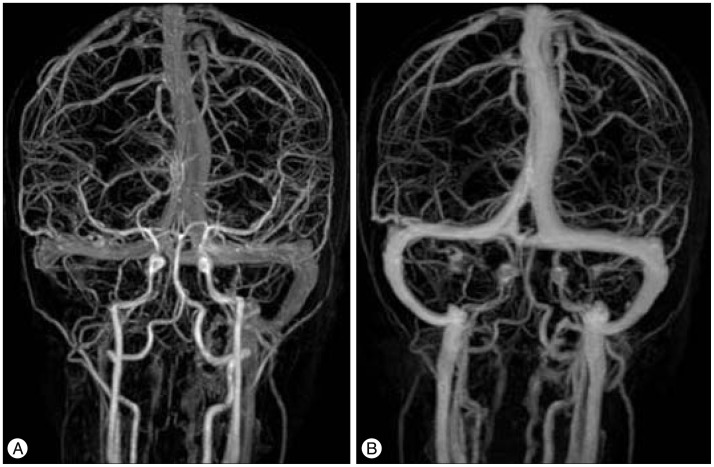
- Cerebral venous sinus thrombosis (CVST) following a closed head injury in pediatric patients is a rare condition, and an early spontaneous recanalization of this condition is extremely rare. A 10-year-old boy was admitted with a mild, intermittent headache and nausea five days after a bicycle accident. The brain computed tomography showed an epidural hematoma at the right occipital area with pneumocephalus due to a fracture of the occipital skull bone. The brain magnetic resonance imaging and the magnetic resonance venography demonstrated a flow signal loss from the right sigmoid sinus to the right jugular vein. The diagnosis was sigmoid sinus thrombosis, so close observations were selected as a treatment for the patient because of his gradually improving symptoms; however, he complained of vomiting 14 days the after conservative treatment. The patient was readmitted for a further examination of his symptoms. The laboratory and the gastroenterological examinations were normal. Due to concern regarding the worsening of the sigmoid sinus thrombosis, the brain magnetic resonance venography was rechecked and it revealed the recanalization of the venous flow in the sigmoid sinus and in the jugular vein.
MeSH Terms
Figure
Cited by 1 articles
-
Mechanical Thrombectomy for Refractory Cerebral Venous Sinus Thrombosis in a Child with Nephrotic Syndrome : A Case Report
Jing Ye, Yuan Yang, Weifeng Wan, Xuntai Ma, Lei Liu, Yong Liu, Zhongchun He, Zhengzhou Yuan
J Korean Neurosurg Soc. 2023;66(6):735-742. doi: 10.3340/jkns.2022.0254.
Reference
-
1. Awad AW, Bhardwaj R. Acute posttraumatic pediatric cerebral venous thrombosis : case report and review of literature. Surg Neurol Int. 2014; 5:53. PMID: 24818060.
Article2. Barnes C, Newall F, Furmedge J, Mackay M, Monagle P. Cerebral sinus venous thrombosis in children. J Paediatr Child Health. 2004; 40:53–55. PMID: 14718006.
Article3. Bishop FS, Finn MA, Samuelson M, Schmidt RH. Endovascular balloon angioplasty for treatment of posttraumatic venous sinus thrombosis. Case report. J Neurosurg. 2009; 111:17–21. PMID: 19326975.
Article4. Brors D, Schäfers M, Schick B, Dazert S, Draf W, Kahle G. Sigmoid and transverse sinus thrombosis after closed head injury presenting with unilateral hearing loss. Neuroradiology. 2001; 43:144–146. PMID: 11326560.
Article5. Buonanno FS, Moody DM, Ball MR, Laster DW. Computed cranial tomographic findings in cerebral sinovenous occlusion. J Comput Assist Tomogr. 1978; 2:281–290. PMID: 263491.
Article6. Dalgiç A, Seçer M, Ergüngör F, Okay O, Akdağ R, Ciliz D. Dural sinus thrombosis following head injury : report of two cases and review of the literature. Turk Neurosurg. 2008; 18:70–77. PMID: 18382983.7. deVeber G, Andrew M, Adams C, Bjornson B, Booth F, Buckley DJ, et al. Cerebral sinovenous thrombosis in children. N Engl J Med. 2001; 345:417–423.
Article8. Georgoulis G, Alexiou G, Prodromou N. Sigmoid sinus thrombosis as a sequela of head injury in children and its management. World Neurosurg. 2014; 81:e7.
Article9. Holzmann D, Huisman TA, Linder TE. Lateral dural sinus thrombosis in childhood. Laryngoscope. 1999; 109:645–651. PMID: 10201757.
Article10. Jackson BF, Porcher FK, Zapton DT, Losek JD. Cerebral sinovenous thrombosis in children : diagnosis and treatment. Pediatr Emerg Care. 2011; 27:874–880. quiz 881-883PMID: 21926891.11. Killewich LA, Bedford GR, Beach KW, Strandness DE Jr. Spontaneous lysis of deep venous thrombi : rate and outcome. J Vasc Surg. 1989; 9:89–97. PMID: 2911146.12. Killewich LA, Macko RF, Cox K, Franklin DR, Benjamin ME, Lilly MP, et al. Regression of proximal deep venous thrombosis is associated with fibrinolytic enhancement. J Vasc Surg. 1997; 26:861–868. PMID: 9372826.
Article13. Lebowitz DC, Ko MW, Cameron EK, Ko PY. Cerebral sinus thrombosis in a 6-year-old boy after a minor head injury. Pediatr Emerg Care. 2014; 30:177–179. PMID: 24589805.
Article14. Markel A, Meissner M, Manzo RA, Bergelin RO, Strandness DE Jr. Deep venous thrombosis : rate of spontaneous lysis and thrombus extension. Int Angiol. 2003; 22:376–382. PMID: 15153822.15. Meissner MH, Zierler BK, Bergelin RO, Chandler WL, Strandness DE Jr. Coagulation, fibrinolysis, and recanalization after acute deep venous thrombosis. J Vasc Surg. 2002; 35:278–285. PMID: 11854725.
Article16. Muthukumar N. Uncommon cause of sinus thrombosis following closed mild head injury in a child. Childs Nerv Syst. 2005; 21:86–88. PMID: 15168052.
Article17. Nehme J, Dcarie JC, Saliba I. Lateral sinus thrombosis : complication of minor head injury. Int J Pediatr Otorhinolaryngol. 2009; 73:629–635. PMID: 19084283.18. Ochagavia AR, Boque MC, Torre C, Alonso S, Sirvent JJ. Dural venous sinus thrombosis due to cranial trauma. Lancet. 1996; 347:1564. PMID: 8684142.
Article19. Saposnik G, Barinagarrementeria F, Brown RD Jr, Bushnell CD, Cucchiara B, Cushman M, et al. Diagnosis and management of cerebral venous thrombosis : a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011; 42:1158–1192. PMID: 21293023.
Article20. Shigemori Y, Koshinaga M, Suma T, Nakamura S, Murata Y, Kawamata T, et al. Jugular bulb venous thrombosis caused by mild head injury : a case report. Surg Neurol. 2007; 68:660–664. discussion 664PMID: 18053865.
Article21. Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med. 2005; 352:1791–1798. PMID: 15858188.
Article22. Stiefel D, Eich G, Sacher P. Posttraumatic dural sinus thrombosis in children. Eur J Pediatr Surg. 2000; 10:41–44. PMID: 10770246.
Article23. Taha JM, Crone KR, Berger TS, Becket WW, Prenger EC. Sigmoid sinus thrombosis after closed head injury in children. Neurosurgery. 1993; 32:541–545. discussion 545-546PMID: 8474644.
Article24. Tamimi A, Abu-Elrub M, Shudifat A, Saleh Q, Kharazi K, Tamimi I. Superior sagittal sinus thrombosis associated with raised intracranial pressure in closed head injury with depressed skull fracture. Pediatr Neurosurg. 2005; 41:237–240. PMID: 16195674.
Article25. Yuen HW, Gan BK, Seow WT, Tan HK. Dural sinus thrombosis after minor head injury in a child. Ann Acad Med Singapore. 2005; 34:639–641. PMID: 16382251.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Pulsatile Tinnitus by Sigmoid Sinus Diverticulum
- Thrombosis and Recanalization of Small Saccular Cerebral Aneurysm : Two Case Reports and a Suggestion for Possible Mechanism
- Fatal Septic Internal Jugular Vein-Sigmoid Sinus Thrombosis Associated with a Malpositioned Central Venous Catheter
- MR imaging of dural sinus thrombosis: A case report
- Intracranial Occlusion of Internal Carotid Artery in Acute Closed Head Injury: Case Report