J Korean Neurosurg Soc.
2015 Mar;57(3):197-203. 10.3340/jkns.2015.57.3.197.
The Effects of Propofol and Thiopental Continuous Infusion on Serum Potassium Disturbances in Neurosurgical Patients
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul, Korea. hppark@snu.ac.kr
- 2Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea.
- KMID: 2191221
- DOI: http://doi.org/10.3340/jkns.2015.57.3.197
Abstract
OBJECTIVE
The potassium disturbance associated with thiopental continuous infusion in neurosurgical patients is well known. However, the effect of propofol continuous infusion on serum potassium levels has not been investigated extensively.
METHODS
We reviewed the medical records of 60 consecutive patients who received coma therapy or deep sedation for intracranial pressure control using either thiopental or propofol between January 2010 and January 2012.
RESULTS
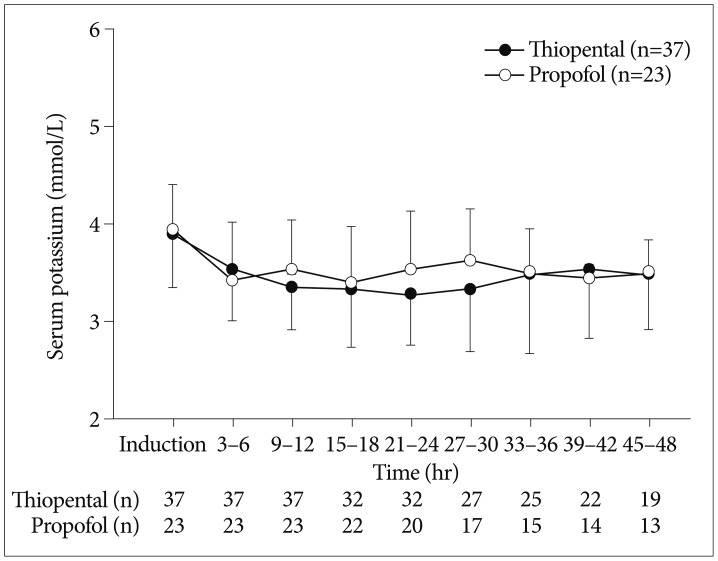
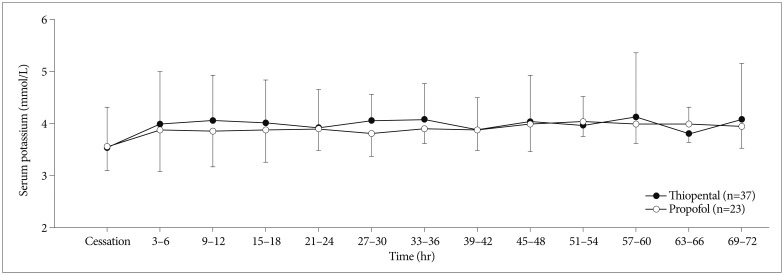
The overall incidence of hypokalemia (K<3.5 mmol/L) was comparable between thiopental and propofol groups (89.2% vs. 82.6%). But, the incidence of moderate to severe hypokalemia (K<3.0 mmol/L) was significantly higher in thiopental group (51.4% vs. 13.0%, p=0.003). The lowest potassium level (2.9 mmol/L vs. 3.2 mmol/L, p=0.020) was lower in thiopental group. The patients in the thiopental group required greater potassium replacement than the propofol group patients (0.08 mmol/kg/h vs. 0.02 mmol/kg/h, p<0.001). On multivariate analysis, thiopental [odds ratio, 95% confidence interval, 7.31 (1.78-27.81); p=0.005] was associated with moderate to severe hypokalemia during continuous infusion. The incidence of rebound hyperkalemia (K>5.0 mmol/L, 32.4% vs. 4.3%, p=0.010) and the peak potassium concentration (4.8 mmol/L vs. 4.2 mmol/L, p=0.037) after the cessation of therapy were higher in thiopental group. On multivariate analysis, thiopental [8.82 (1.00-77.81); p=0.049] and duration of continuous infusion [1.02 (1.00-1.04); p=0.016] were associated with rebound hyperkalemia once therapy was discontinued.
CONCLUSION
Propofol was less frequently associated with moderate to severe hypokalemia after induction and rebound hyperkalemia following the cessation of continuous infusion than thiopental.
MeSH Terms
Figure
Reference
-
1. An HS, Cho BM, Kang JH, Kim MK, Oh SM, Park SH. Efficacy of low dose barbiturate coma therapy for the patients with intractable intracranial hypertension using the bispectral index monitoring. J Korean Neurosurg Soc. 2010; 47:252–257. PMID: 20461164.
Article2. Astrup J, Rosenørn J, Cold GE, Bendtsen A, Møller Sørensen P. Minimum cerebral blood flow and metabolism during craniotomy. Effect of thiopental loading. Acta Anaesthesiol Scand. 1984; 28:478–481. PMID: 6496004.
Article3. Beal AL, Scheltema KE, Beilman GJ, Deuser WE. Hypokalemia following trauma. Shock. 2002; 18:107–110. PMID: 12166770.
Article4. Cairns CJ, Thomas B, Fletcher S, Parr MJ, Finfer SR. Life-threatening hyperkalaemia following therapeutic barbiturate coma. Intensive Care Med. 2002; 28:1357–1360. PMID: 12209290.
Article5. Capparelli FJ, Abello M, Patricio Maskin L, Arista E, Hlavnicka A, Diaz MF, et al. QTc prolongation after brain surgery. Neurol Res. 2013; 35:159–162. PMID: 23452578.
Article6. Carlsson C, Harp JR, Siesjö BK. Metabolic changes in the cerebral cortex of the rat induced by intravenous pentothalsodium. Acta Anaesthesiol Scand Suppl. 1975; 57:1–17. PMID: 128981.
Article7. Fogarty DJ, McCleane GJ. Propofol and serum potassium. Anaesthesia. 1992; 47:63–64. PMID: 1536410.
Article8. Friederich P, Urban BW. Interaction of intravenous anesthetics with human neuronal potassium currents in relation to clinical concentrations. Anesthesiology. 1999; 91:1853–1860. PMID: 10598630.
Article9. Hall RI, Sandham D, Cardinal P, Tweeddale M, Moher D, Wang X, et al. Propofol vs midazolam for ICU sedation : a Canadian multicenter randomized trial. Chest. 2001; 119:1151–1159. PMID: 11296183.10. Hartung HJ. [Intracranial pressure in patients with craniocerebral trauma after administration of propofol and thiopental]. Anaesthesist. 1987; 36:285–287. PMID: 3498377.11. Jung JY, Lee C, Ro H, Kim HS, Joo KW, Kim Y, et al. Sequential occurrence of life-threatening hypokalemia and rebound hyperkalemia associated with barbiturate coma therapy. Clin Nephrol. 2009; 71:333–337. PMID: 19281748.
Article12. Kam PC, Cardone D. Propofol infusion syndrome. Anaesthesia. 2007; 62:690–701. PMID: 17567345.
Article13. Kelly DF, Goodale DB, Williams J, Herr DL, Chappell ET, Rosner MJ, et al. Propofol in the treatment of moderate and severe head injury : a randomized, prospective double-blinded pilot trial. J Neurosurg. 1999; 90:1042–1052. PMID: 10350250.
Article14. Lee JH, Ko YS, Shin HJ, Yi JH, Han SW, Kim HJ. Is There a Relationship between Hyperkalemia and Propofol? Electrolyte Blood Press. 2011; 9:27–31. PMID: 21998604.
Article15. Lee JI, Kim YZ, Kim JS, Choi YC, Kim KH. Clinical comparison between barbiturate and propofol coma therapy in the patients with severe traumatic brain injury. J Korean Neurotraumatol Soc. 2008; 4:24–30.
Article16. Machata AM, Gonano C, Bîrsan T, Zimpfer M, Spiss CK. Rare but dangerous adverse effects of propofol and thiopental in intensive care. J Trauma. 2005; 58:643–645. PMID: 15761368.
Article17. Michenfelder JD. The interdependency of cerebral functional and metabolic effects following massive doses of thiopental in the dog. Anesthesiology. 1974; 41:231–236. PMID: 4854910.
Article18. Neil MJ, Dale MC. Hypokalaemia with severe rebound hyperkalaemia after therapeutic barbiturate coma. Anesth Analg. 2009; 108:1867–1868. PMID: 19448214.
Article19. Ng SY, Chin KJ, Kwek TK. Dyskalaemia associated with thiopentone barbiturate coma for refractory intracranial hypertension : a case series. Intensive Care Med. 2011; 37:1285–1289. PMID: 21567112.
Article20. Otterspoor LC, Kalkman CJ, Cremer OL. Update on the propofol infusion syndrome in ICU management of patients with head injury. Curr Opin Anaesthesiol. 2008; 21:544–551. PMID: 18784477.
Article21. Pomeranz S, Constantini S, Rappaport ZH. Hypokalaemia in severe head trauma. Acta Neurochir (Wien). 1989; 97:62–66. PMID: 2718795.
Article22. Ravussin P, Guinard JP, Ralley F, Thorin D. Effect of propofol on cerebrospinal fluid pressure and cerebral perfusion pressure in patients undergoing craniotomy. Anaesthesia. 1988; 43(Suppl):37–41. PMID: 3259094.
Article23. Schaefer M, Link J, Hannemann L, Rudolph KH. Excessive hypokalemia and hyperkalemia following head injury. Intensive Care Med. 1995; 21:235–237. PMID: 7790611.
Article24. Schalén W, Messeter K, Nordström CH. Complications and side effects during thiopentone therapy in patients with severe head injuries. Acta Anaesthesiol Scand. 1992; 36:369–377. PMID: 1595344.
Article25. Shin IW, Sohn JT, Choi JY, Lee HK, Lee CH, Chung YK. Cardiac arrest due to Severe hypokalemia during barbiturate coma therapy in a patient with severe acute head injury : a case report. Korean J Anesthesiol. 2006; 50:S71–S73.26. Stephan H, Sonntag H, Schenk HD, Kohlhausen S. [Effect of Disoprivan (propofol) on the circulation and oxygen consumption of the brain and CO2 reactivity of brain vessels in the human]. Anaesthesist. 1987; 36:60–65. PMID: 3107419.27. Van Hemelrijck J, Fitch W, Mattheussen M, Van Aken H, Plets C, Lauwers T. Effect of propofol on cerebral circulation and autoregulation in the baboon. Anesth Analg. 1990; 71:49–54. PMID: 2363528.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Effects of Propofol-Succinylcholine and Thiopentone-Succinylcholine on the Serum Potassium
- A Comparison Study of Propofol and Nitrous Oxide for Induction and Maintenance of Anesthesia in Cesarean Section with Thiopental and Enflurane
- Maternal and Neonatal Effects of Thiopental Sodium-Enflurane-N2O and Propofol-N2O Anesthesia for Cesarean Section
- Comparison of Propofol and Thiopental Anesthesia for Ambulatory Surgery
- The Changes of Serum Triiodothyronine(T3) and Thyroxine(T4) Levels during General Anesthesia with Enflurane and Propofol