J Korean Orthop Assoc.
2007 Aug;42(4):453-460. 10.4055/jkoa.2007.42.4.453.
Progression of Preoperative Degeneration of the Adjacent Segmentafter Instrumented Lumbar Arthrodesis
- Affiliations
-
- 1Department of Orthopedic Surgery, Inha University College of Medicine, Incheon, Korea. chokj@inha.ac.kr
- KMID: 2186506
- DOI: http://doi.org/10.4055/jkoa.2007.42.4.453
Abstract
-
PURPOSE: Preoperative degeneration has not been clearly defined as a risk factor of adjacent segment disease (ASD). The aim of this study was to analyze the progression of preoperative degeneration at the adjacent segment after instrumented lumbar fusion.
MATERIALS AND METHODS
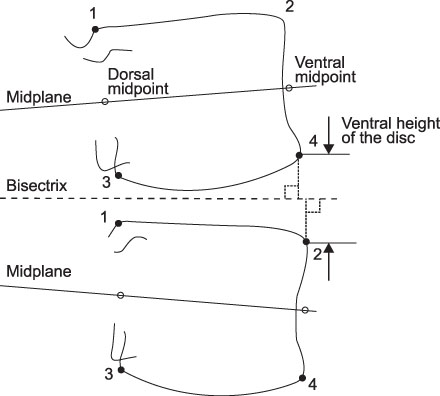
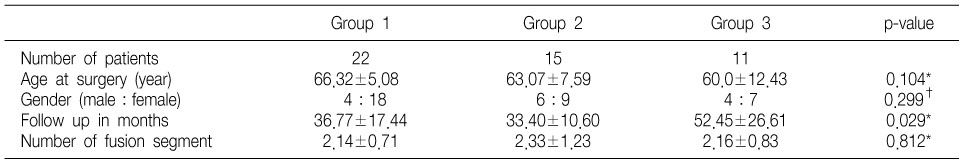
Forty-eight patients (mean age: 63.9, range: 39-77) who underwent posterolateral fusion for a degenerative lumbar spine were reviewed. All the patients showed preoperative degenerative changes at the adjacent segment. The preoperative degeneration included disc degeneration (n=42), degenerative lumbar scoliosis (n=7), posterior translation (n=7), lateral translation (n=9), and spondylolisthesis (n=1). The patients were divided into the following three groups according to the progression of degeneration: Group I, No progression; Group II, asymptomatic radiographic progression; and Group III, symptomatic progression.
RESULTS
There were 22, 15, and 11 patients in Groups I, II and III, respectively. The incidence of symptomatic progression of degeneration was 22.9%. Of the 42 patients showing disc degeneration, 9 patients (21.4%) developed symptomatic progression. On the other hand, 3 out of 7 (42.9%) patients with posterior translation and 5 out of 7 (71.4%) patients with degenerative scoliosis developed symptomatic progression. The age and number of fused segments were not predisposing factors to progression.
CONCLUSION
The incidence of symptomatic adjacent segment disease in patients with preoperative degeneration was 22.9%. Preoperative coronal malalignment and posterior translation might be risk factors for adjacent segment disease. Correct selection of the fusion level is important for reducing the incidence of adjacent segment disease.
MeSH Terms
Figure
Cited by 1 articles
-
Proximal Adjacent Segment Disease following Posterior Instrumentation and Fusion for Degenerative Lumbar Scoliosis
Kyu-Jung Cho, Seung-Lim Park, Myung-Gu Kim, Yung-Hyun Yoon, Joong-Sun Lee, Se-Il Suk
J Korean Orthop Assoc. 2009;44(1):109-117. doi: 10.4055/jkoa.2009.44.1.109.
Reference
-
1. Aota Y, Kumano K, Hirabayashi S. Postfusion instability at the adjacent segment after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Disord. 1995. 8:464–473.2. Bastian L, Lange U, Knop C, Tusch G, Blauth M. Evaluation of the mobility of adjacent segment after posterior thoracolumbar fixation: a biomechanical study. Eur Spine J. 2001. 10:295–300.3. Booth KC, Bridwell KH, Eisenberg BA, Baldus CR, Lenke LG. Minimum 5-year results of degenerative spondylolisthesis treated with decompression and instrumented posterior fusion. Spine. 1999. 24:1721–1727.
Article4. Chen WJ, Lai PL, Chen LH. Adjacent instability after instrumented lumbar fusion. Chang Gung Med J. 2003. 26:792–798.5. Etebar S, Cahill DW. Risk factors for adjacent segment failure following lumbar fixation with rigid instrumentation for degenerative instability. J Neurosurg. 1999. 90:Suppl 2. S163–S169.6. Frobin W, Brinckmann P, Kramer M, Hartwig E. Height of lumbar discs measured from radiographs compared with degeneration and height classified from MR images. Eur Radiol. 2001. 11:263–269.
Article7. Frymoyer JW, Hanley E, Howe J, Kuhlmann D, Matteri RE. A comparison of radiographic findings in fusion and nonfusion patients ten or more years following lumbar disc surgery. Spine. 1979. 4:435–440.
Article8. Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am. 2004. 86:1497–1503.
Article9. Guigui P, Lambert P, Lassale B, Deburge A. Long term outcome at adjacent level of lumbar arthrodesis. Rev Chir Orthop Reparatrice Appar Mot. 1997. 83:685–696.10. Ha KY, Kim YH, Kang KS. Surgery for adjacent segment changes after lumbosacral fusion. J Korean Soc Spine Surg. 2002. 9:332–340.
Article11. Ha KY, Moon MS, Paek SY. Effect of instrumental stabilization and fusion of degenerative lumbar scoliosis on unfused adjacent segment. J Korean Soc Spine Surg. 1995. 2:270–278.12. Ha KY, Sung TP. Changes of the adjacent mobile segment after cat spine fixation. J Korean Orthop Assoc. 1997. 32:1808–1816.
Article13. Hambly MF, Wiltse LL, Raghavan N, Schneiderman G, Koenig C. The transition zone above a lumbosacral fusion. Spine. 1998. 23:1785–1792.
Article14. Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. 2004. 4:Suppl 6. S190–S194.
Article15. Jeon CH, Chung NS, Yang YM, Kim NH, Kim YC, Kim KH. Adjacent segment degeneration after spinal fusion in lumbar degenerative disorders. J Korean Soc Spine Surg. 2004. 11:238–245.
Article16. Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J. 2001. 10:314–319.
Article17. Kumar MN, Jacquot F, Hall H. Long-term following up of functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease. Eur Spine J. 2001. 10:309–313.18. Lee CK, Langrana NA. Lumbosacral spinal fusion. A biomechanical study. Spine. 1984. 9:574–581.
Article19. Miyakoshi N, Abe E, Shimada Y, Okuyama K, Suzuki T, Sato K. Outcome of one-level posterior lumbar interbody fusion for spondylolisthesis and postoperative intervertebral disc degeneration adjacent to the fusion. Spine. 2000. 25:1837–1842.
Article20. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine. 2004. 29:1938–1944.
Article21. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. 2001. 26:1873–1878.
Article22. Rahm MD, Hall BB. Adjacent-segment degeneration after lumbar fusion with instrumentation: a retrospective study. J Spinal Disord. 1996. 9:392–400.23. Schlegel JD, Smith JA, Schleusener RL. Lumbar motion segment pathology adjacent to thoracolumbar, lumbar, and lumbosacral fusion. Spine. 1996. 21:970–981.24. Stagnara P, De Mauroy JC, Dran G, et al. Reciprocal angulation of the vertebral bodies in the saggital plane: approach to references for the evaluation of kyphosis and lordosis. Spine. 1982. 7:335–342.25. Throckmorton TW, Hilibrand AS, Mencio GA, Hodge A, Spengler DM. The impact of adjacent level disc degeneration on health status outcomes following lumbar fusion. Spine. 2003. 28:2546–2550.
Article26. Whitecloud TS, David JM, Olive PM. Operative treatment of the degenerated segment adjacent to a lumbar fusion. Spine. 1994. 19:531–536.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship between New Osteoporotic Vertebral Fracture and Instrumented Lumbar Arthrodesis
- Revision Arthrodesis After Lumbar Fusion in Degenerative Lumbar Disease
- The Causes of Revision Arthrodesis for the Degenerative Changes at the Adjacent Segment after Lumbosacral Fusion for Degenerative Lumbar Diseases
- Change of Lumbar Motion after Multi-Level Posterior Dynamic Stabilization with Bioflex System : 1 Year Follow Up
- Predictable Risk Factors for Adjacent Segment Degeneration After Lumbar Fusion