J Korean Orthop Assoc.
2009 Dec;44(6):627-633. 10.4055/jkoa.2009.44.6.627.
Preliminary Results after Reduction of DDH via Medial Approach
- Affiliations
-
- 1Department of Orthopaedic Surgery, Seoul National University College of Medicine, Seoul, Korea. tjcho@snu.ac.kr
- KMID: 2186289
- DOI: http://doi.org/10.4055/jkoa.2009.44.6.627
Abstract
- PURPOSE
We report the outcomes of medial open reduction for developmental dysplasia of the hip (DDH).
MATERIALS AND METHODS
This study reviewed the medical records and radiographs of 33 DDH cases treated by a medial open reduction and followed for at least two years. The mean age at surgery and follow-up duration was 11.4 months (range, 4 to 22) and 88 months (range, 24 to 168), respectively. The perioperative parameters, maintenance of reduction, and postoperative changes in the acetabular index and center-edge angle were recorded.
RESULTS
The acetabular index decreased from a preoperative average of 35degrees to 16degrees at the latest follow-up. The center-edge angle improved from an average of 7degrees at postoperative 1 year to 22degrees at the latest follow-up. A secondary bony procedure was performed in 15 cases at average age of 4.4 years. Avascular necrosis was noted in 8 cases, all of whom belonged to Kalamchi group I. Among the 21 patients over 6 years-old at the latest follow-up, 18 belonged to Severin groups I or II and the remaining 3 to group III. Redislocation occurred in one case.
CONCLUSION
A medial open reduction is a minimal surgical procedure that can effectively release the structures obstructing a femoral head reduction. It should be a useful treatment modality for selected cases with DDH.
MeSH Terms
Figure
Reference
-
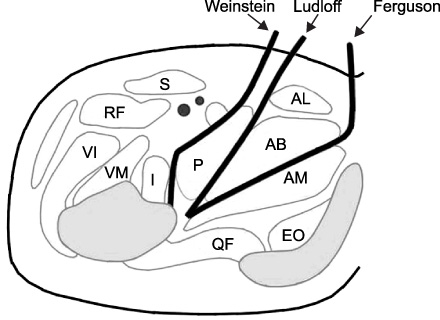
1. Ludloff K. The open reduction of the congenital hip dislocation by an anterior incision. Am J Orthop Surg. 1913. 10:438–454.2. Ferguson AB Jr. Primary open reduction of congenital dislocation of the hip using a median adductor approach. J Bone Joint Surg Am. 1973. 55:671–689.
Article3. Weinstein SL, Ponseti IV. Congenital dislocation of the hip. J Bone Joint Surg Am. 1979. 61:119–124.
Article4. Castillo R, Sherman FC. Medial adductor open reduction for congenital dislocation of the hip. J Pediatr Orthop. 1990. 10:335–340.
Article5. Kalamchi A, Schmidt TL, MacEwen GD. Congenital dislocation of the hip. Open reduction by the medial approach. Clin Orthop Relat Res. 1982. 169:127–132.6. Koizumi W, Moriya H, Tsuchiya K, Takeuchi T, Kamegaya M, Akita T. Ludloff's medial approach for open reduction of congenital dislocation of the hip. A 20-year follow-up. J Bone Joint Surg Br. 1996. 78:924–929.7. Roose PE, Chingren GL, Klaaren HE, Broock G. Open reduction for congenital dislocation of the hip using the Ferguson procedure. A review of twenty six cases. J Bone Joint Surg Am. 1979. 61:915–921.8. Mankey MG, Arntz GT, Staheli LT. Open reduction through a medial approach for congenital dislocation of the hip. A critical review of the Ludloff approach in sixty-six hips. J Bone Joint Surg Am. 1993. 75:1334–1345.
Article9. Mergen E, Adyaman S, Omeroglu H, Erdemli B, Isiklar U. Medial approach open reduction for congenital dislocation of the hip using the Ferguson procedure. A review of 31 hips. Arch Orthop Trauma Surg. 1991. 110:169–172.10. Isiklar ZU, Kandemir U, Ucar DH, Tumer Y. Is concomitant bone surgery necessary at the time of open reduction in developmental dislocation of the hip in children 12-18 months old? Comparison of open reduction in patients younger than 12 months old and those 12-18 months old. J Pediatr Orthop B. 2006. 15:23–27.
Article11. Rowe SM, Chun CH. Medial approach open reduction in congenital dislocation of hip. J Korean Orthop Assoc. 1986. 21:1063–1069.12. Salter RB, Kostuik J, Dallas S. Avascular necrosis of the femoral head as a complication of treatment for congenital dislocation of the hip in young children: a clinical and experimental investigation. Can J Surg. 1969. 12:44–61.13. Forlin E, Choi IH, Guille JT, Bowen JR, Glutting J. Prognostic factors in congenital dislocation of the hip treated with closed reduction. The importance of arthrographic evaluation. J Bone Joint Surg Am. 1992. 74:1140–1152.
Article14. Chen IH, Kuo KN, Lubicky JP. Prognosticating factors in acetabular development following reduction of developmental dysplasia of the hip. J Pediatr Orthop. 1994. 14:3–8.
Article15. Kalamchi A, MacEwen GD. Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg Am. 1980. 62:876–888.
Article16. Severin E. Congenital dislocation of the hip; development of the joint after closed reduction. J Bone Joint Surg Am. 1950. 32:507–518.17. Salter RB. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. J Bone Joint Surg Br. 1961. 43:518–539.
Article18. Grudziak JS, Ward WT. Dega osteotomy for the treatment of congenital dysplasia of the hip. J Bone Joint Surg Am. 2001. 83:845–854.
Article19. Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988. 232:26–36.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Percutaneous Pin Fixation for Unstable Developmental Dislocation of the Hip
- Medial Approach of Supracondylar Fracture of the Humerus in Children
- The Transcaruncular Approach for the Reduction of Medial Orbital Wall Fracture
- Open reduction and Internal Fixation of Calcaneus Fractures by Staples and Screws
- Treatment of Congenital Dislocation of Hip by Open Reduction