J Korean Orthop Assoc.
2011 Jun;46(3):200-204. 10.4055/jkoa.2011.46.3.200.
The Comparative Study between Combined and Posterior Surgical Treatments for Post-traumatic Kyphosis
- Affiliations
-
- 1Department of Orthopaedic Surgery, Guri Hospital, Hanyang University College of Medicine, Guri, Korea. hyparkys@hanyang.ac.kr
- KMID: 2185445
- DOI: http://doi.org/10.4055/jkoa.2011.46.3.200
Abstract
- PURPOSE
We wanted to analyse the differences of the radiological and clinical results between the combined approach and the posterior approach for treating posttraumatic kyphosis in elderly patients and to determine the risk factors for the loss of correction after the operation.
MATERIALS AND METHODS
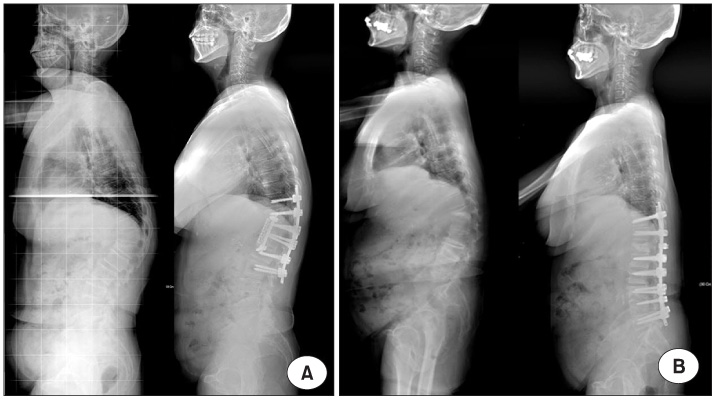
Between September 2004 and August 2009, 19 patients who underwent an operation for posttraumatic kyphosis and were follow-up for at least one year were included in this study. The combined approach (A group) was done for 10 patients, while the posterior approach (B group) was done for 9 patients. Radiological study and clinical evaluation, including the Korean version of the Oswestry disability index and the visual analog scale (VAS), were performed before surgery, after surgery and at the final follow-up. The risk factors related to the loss of correction of kyphosis at the fracture site were analyzed.
RESULTS
In group A, the mean kyphotic angles were 35.2 before surgery, 11.1 degrees after surgery and 15.7 degrees at the final follow-up. There was 24.1 degrees (correction; 68.5%) of correction of the kyphotic angle with 4.6 degrees (19%) loss of correction. In group B, the mean kyphotic angles were 34.2 before surgery, 9.3 degrees after surgery and 13.8 degrees at the final follow-up. There was 24.9 degrees (72.8%) correction of the kyphotic angle with 4.5 degrees (18.3%) loss of correction. The clinical data was improved to the same degrees. The loss of correction was statistically correlated with osteoporosis.
CONCLUSION
In conclusion, the posterior approach can correct the posttraumatic kyphosis in a fashion similar to that of the combined approach. The patient's osteoporosis should be thoroughly treated for preventing correction loss.
Figure
Reference
-
1. Buchowski JM, Kuhns CA, Bridwell KH, Lenke LG. Surgical management of posttraumatic thoracolumbar kyphosis. Spine J. 2008. 8:666–677.
Article2. Gronholz MJ. Prevention, diagnosis, and management of osteoporosis-related fracture: a multifactoral osteopathic approach. J Am Osteopath Assoc. 2008. 108:575–585.3. Schneider DL, von Mühlen D, Barrett-Connor E, Sartoris DJ. Kyphosis does not equal vertebral fractures: the Rancho Bernardo study. J Rheumatol. 2004. 31:747–752.4. Gaines RW Jr. The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am. 2000. 82-A:1458–1476.
Article5. Vaccaro AR, Silber JS. Post-traumatic spinal deformity. Spine (Phila Pa 1976). 2001. 26:24 Suppl. S111–S118.
Article6. Suk SI, Kim JH, Chung ER, et al. Surgical treatment of post-traumatic kyphosis with neurologic compromised osteoporotic fracture-comparison between anterior-posterior surgery versus posterior egg-shell procedure. J Korean Soc Spine Surg. 2002. 9:148–157.7. Fairbank JCT, Pynsent PB. The oswestry disability index. Spine. 2000. 25:2940–2953.
Article8. Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS 3rd, Cook SD. Effects of bone mineral density on pedicle screw fixation. Spine (Phila Pa 1976). 1994. 19:2415–2420.
Article9. Bridwell KH. Causes of sagittal spinal imbalance and assessment of the extent of needed correction. Instr Course Lect. 2006. 55:567–575.10. Chin DK, Park JY, Yoon YS, et al. Prevalence of osteoporosis in patients requiring spine surgery: incidence and significance of osteoporosis in spine disease. Osteoporos Int. 2007. 18:1219–1224.
Article11. Gehrig L, Lane J, O'Connor MI. Osteoporosis: management and treatment strategies for orthopaedic surgeons. J Bone Joint Surg Am. 2008. 90:1362–1374.12. Manson NA, Phillips FM. Minimally invasive techniques for the treatment of osteoporotic vertebral fractures. J Bone Joint Surg Am. 2006. 88:1862–1872.
Article13. Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine (Phila Pa 1976). 2006. 31:19 Suppl. S171–S178.
Article14. Gill JB, Levin A, Burd T, Longley M. Corrective osteotomies in spine surgery. J Bone Joint Surg Am. 2008. 90:2509–2520.
Article15. Suk SI, Kim JH, Lee SM, Chung ER, Lee JH. Anterior-posterior surgery versus posterior closing wedge osteotomy in posttraumatic kyphosis with neurologic compromised osteoporotic fracture. Spine (Phila Pa 1976). 2003. 28:2170–2175.
Article16. Bridwell KH, Lewis SJ, Lenke LG, Baldus C, Blanke K. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Joint Surg Am. 2003. 85-A:454–463.
Article17. Bridwell KH, Lewis SJ, Rinella A, Lenke LG, Baldus C, Blanke K. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. Surgical technique. J Bone Joint Surg Am. 2004. 86-A:Suppl 1. 44–50.18. Murrey DB, Brigham CD, Kiebzak GM, Finger F, Chewning SJ. Transpedicular decompression and pedicle subtraction osteotomy (eggshell procedure): a retrospective review of 59 patients. Spine (Phila Pa 1976). 2002. 27:2338–2345.19. Kim EH, Cho KN, Kim CH. Surgical treatment of post-traumatic kyphosis. J Korean Orthop Assoc. 1998. 33:367–374.20. Burval DJ, McLain RF, Milks R, Inceoglu S. Primary pedicle screw augmentation in osteoporotic lumbar vertebrae: biomechanical analysis of pedicle fixation strength. Spine (Phila Pa 1976). 2007. 32:1077–1083.21. Cook SD, Salkeld SL, Stanley T, Faciane A, Miller SD. Biomechanical study of pedicle screw fixation in severely osteoporotic bone. Spine J. 2004. 4:402–408.22. Kado DM, Prenovost K, Crandall C. Narrative review: hyperkyphosis in older persons. Ann Intern Med. 2007. 147:330–338.
Article23. Lee JC, Soh JW, Jo JH, Kim YI, Shin BJ. Comparative analysis of surgical options in the treatment of lumbar degenerative kyphosis. J Korean Soc Spine Surg. 2009. 16:8–16.
Article24. Tokuhashi Y, Ajiro Y, Umezawa N. Outcomes of posterior fusion using pedicle screw fixation in patients >or=70 years with lumbar spinal canal stenosis. Orthopedics. 2008. 31:1096.
Article25. Seo WY, Park YS, Cho JL. Does a radiolucent zone surrounding the pedicle screws mean nonunion? J Korean Orthop Assoc. 2009. 44:344–349.
Article26. Chang MC, Liu CL, Chen TH. Polymethylmethacrylate augmentation of pedicle screw for osteoporotic spinal surgery: a novel technique. Spine (Phila Pa 1976). 2008. 33:E317–E324.27. Guyer RD, Patterson M, Ohnmeiss DD. Failed back surgery syndrome: diagnostic evaluation. J Am Acad Orthop Surg. 2006. 14:534–543.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment of Post - traumatic Kyphosis
- Surgical Treatment in Delayed Posttraumatic Thoracolumbar Kyphosis
- Surgical Correction of Fixed Kyphosis
- Surgical Treatment of Post-Traumatic Kyphosis with Neurologic Compromised Osteoporotic Fracture: Comparison between Anterior-Posterior Surgery versus Posterior Egg-Shell Procedure
- Surgical Correction of Fixed Kyphosis