J Korean Orthop Assoc.
2012 Apr;47(2):133-139. 10.4055/jkoa.2012.47.2.133.
Prediction of Early Postoperative Infection after Arthroplasty Using the C-Reactive Protein Level
- Affiliations
-
- 1Department of Orthopaedic Surgery, Soonchunhyang University College of Medicine, Seoul, Korea. huuytime@gmail.com
- KMID: 2185389
- DOI: http://doi.org/10.4055/jkoa.2012.47.2.133
Abstract
- PURPOSE
C-reactive protein (CRP) has been shown to be useful in the diagnosis of periprosthetic infection. This study analyzed the serial CRP measurements in patients with acute postoperative infection by comparing with the serial CRP measurements in patients without postoperative infection.
MATERIALS AND METHODS
From 2004 to 2009, 33 patients with acute postoperative infection developed within 4 weeks of surgery were enrolled including 26 cases of hip arthroplasty and 7 cases of total knee arthroplasty. We measured the serial CRP levels in the groups with both deep infection and superficial infection. The CRP measurements in the group without postoperative infection were also analyzed based on the changing pattern of CRP.
RESULTS
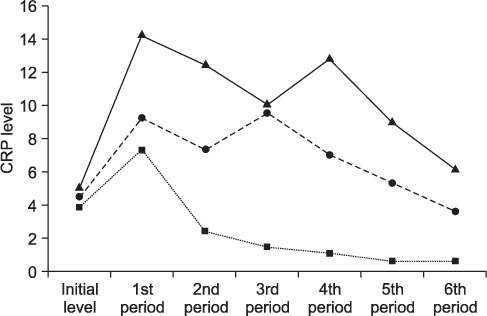
In the non-infected group, CRP level sharply increased in 2-3 days postoperatively and it showed a continuing downward pattern till the third postoperative week. However, a bimodal curve pattern was obtained in the groups with both deep and superficial infection. The group with deep infection showed a second increase in CRP level around the 13th postoperative day and the group with superficial infection showed a second increase in CRP level around the 10th postoperative day.
CONCLUSION
If there are bimodal patterns of CRP after arthroplasty, acute postoperative infections can be suspected. We can treat them effectively without delay by detection of bimodal increase in CRP.
Keyword
Figure
Reference
-
1. Galat DD, McGovern SC, Larson DR, Harrington JR, Hanssen AD, Clarke HD. Surgical treatment of early wound complications following primary total knee arthroplasty. J Bone Joint Surg Am. 2009. 91:48–54.
Article2. Saleh K, Olson M, Resig S, et al. Predictors of wound infection in hip and knee joint replacement: results from a 20 year surveillance program. J Orthop Res. 2002. 20:506–515.
Article3. Bose WJ, Gearen PF, Randall JC, Petty W. Long-term outcome of 42 knees with chronic infection after total knee arthroplasty. Clin Orthop Relat Res. 1995. 319:285–296.
Article4. Brandt CM, Sistrunk WW, Duffy MC, et al. Staphylococcus aureus prosthetic joint infection treated with debridement and prosthesis retention. Clin Infect Dis. 1997. 24:914–919.
Article5. Tsukayama DT, Estrada R, Gustilo RB. Infection after total hip arthroplasty. A study of the treatment of one hundred and six infections. J Bone Joint Surg Am. 1996. 78:512–523.
Article6. Ugraş AA, Kural C, Kural A, Demirez F, Koldaş M, Cetinus E. Which is more important after total knee arthroplasty: local inflammatory response or systemic inflammatory response? Knee. 2011. 18:113–116.
Article7. Bilgen O, Atici T, Durak K, Karaeminoğullari , Bilgen MS. C-reactive protein values and erythrocyte sedimentation rates after total hip and total knee arthroplasty. J Int Med Res. 2001. 29:7–12.
Article8. Koo KH, Yang JW, Cho SH, et al. Impregnation of vancomycin, gentamicin, and cefotaxime in a cement spacer for two-stage cementless reconstruction in infected total hip arthroplasty. J Arthroplasty. 2001. 16:882–892.
Article9. Estes CS, Beauchamp CP, Clarke HD, Spangehl MJ. A two-stage retention débridement protocol for acute periprosthetic joint infections. Clin Orthop Relat Res. 2010. 468:2029–2038.
Article10. Van Kleunen JP, Knox D, Garino JP, Lee GC. Irrigation and débridement and prosthesis retention for treating acute periprosthetic infections. Clin Orthop Relat Res. 2010. 468:2024–2028.
Article11. Chiu FY, Chen CM. Surgical débridement and parenteral antibiotics in infected revision total knee arthroplasty. Clin Orthop Relat Res. 2007. 461:130–135.
Article12. Mont MA, Waldman B, Banerjee C, Pacheco IH, Hungerford DS. Multiple irrigation, debridement, and retention of components in infected total knee arthroplasty. J Arthroplasty. 1997. 12:426–433.
Article13. Vilchez F, Martínez-Pastor JC, García-Ramiro S, et al. Outcome and predictors of treatment failure in early post-surgical prosthetic joint infections due to Staphylococcus aureus treated with debridement. Clin Microbiol Infect. 2011. 17:439–444.
Article14. Piper KE, Fernandez-Sampedro M, Steckelberg KE, et al. C-reactive protein, erythrocyte sedimentation rate and orthopedic implant infection. PLoS One. 2010. 5:e9358.
Article15. Shen H, Zhang N, Zhang X, Ji W. C-reactive protein levels after 4 types of arthroplasty. Acta Orthop. 2009. 80:330–333.
Article16. Dupont C, Rodenbach J, Flachaire E. The value of C-reactive protein for postoperative monitoring of lower limb arthroplasty. Ann Readapt Med Phys. 2008. 51:348–357.
Article17. Greidanus NV, Masri BA, Garbuz DS, et al. Use of erythrocyte sedimentation rate and C-reactive protein level to diagnose infection before revision total knee arthroplasty. A prospective evaluation. J Bone Joint Surg Am. 2007. 89:1409–1416.18. Berbari E, Mabry T, Tsaras G, et al. Inflammatory blood laboratory levels as markers of prosthetic joint infection: a systematic review and meta-analysis. J Bone Joint Surg Am. 2010. 92:2102–2109.19. Neumaier M, Scherer MA. C-reactive protein levels for early detection of postoperative infection after fracture surgery in 787 patients. Acta Orthop. 2008. 79:428–432.
Article20. Jenny JY. C-reactive protein levels for early detection of postoperative infection after fracture surgery in 787 patients. Acta Orthop. 2008. 79:874.21. White J, Kelly M, Dunsmuir R. C-reactive protein level after total hip and total knee replacement. J Bone Joint Surg Br. 1998. 80:909–911.
Article22. Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Am J Infect Control. 1992. 20:271–274.
Article23. Allami MK, Jamil W, Fourie B, Ashton V, Gregg PJ. Superficial incisional infection in arthroplasty of the lower limb. Interobserver reliability of the current diagnostic criteria. J Bone Joint Surg Br. 2005. 87:1267–1271.24. Moran E, Masters S, Berendt AR, McLardy-Smith P, Byren I, Atkins BL. Guiding empirical antibiotic therapy in orthopaedics: the microbiology of prosthetic joint infection managed by debridement, irrigation and prosthesis retention. J Infect. 2007. 55:1–7.
Article25. Darwiche H, Barsoum WK, Klika A, Krebs VE, Molloy R. Retrospective analysis of infection rate after early reoperation in total hip arthroplasty. Clin Orthop Relat Res. 2010. 468:2392–2396.
Article26. Parvizi J, Ghanem E, Menashe S, Barrack RL, Bauer TW. Periprosthetic infection: what are the diagnostic challenges? J Bone Joint Surg Am. 2006. 88:Suppl 4. 138–147.
Article27. Piper KE, Jacobson MJ, Cofield RH, et al. Microbiologic diagnosis of prosthetic shoulder infection by use of implant sonication. J Clin Microbiol. 2009. 47:1878–1884.
Article28. Buttaro MA, Tanoira I, Comba F, Piccaluga F. Combining C-reactive protein and interleukin-6 may be useful to detect periprosthetic hip infection. Clin Orthop Relat Res. 2010. 468:3263–3267.
Article29. Park KK, Kim TK, Chang CB, Yoon SW, Park KU. Normative temporal values of CRP and ESR in unilateral and staged bilateral TKA. Clin Orthop Relat Res. 2008. 466:179–188.
Article30. Di Cesare PE, Chang E, Preston CF, Liu CJ. Serum interleukin-6 as a marker of periprosthetic infection following total hip and knee arthroplasty. J Bone Joint Surg Am. 2005. 87:1921–1927.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erythrocyte sedimentation rate and C-reactive protein values in patients with hip arthroplasty
- The Effectiveness of C-Reactive Protein Surveillance as a Method to Monitor the Post-Operative Antibiotics Administration after Total Knee Replacement Arthroplasty
- Efficacy of Taurolidine Irrigation in Primary Total Knee Arthroplasty
- Early change of C-reactive protein level in TKA : Antibiotic-loaded vs Plain bone cement
- Comparison of Difference in Hematologic and Hemodynamic Outcomes between Primary Total Knee Arthroplasty and Revision of Infected Total Knee Arthroplasty