J Korean Orthop Assoc.
2014 Feb;49(1):1-6. 10.4055/jkoa.2014.49.1.1.
Ankle Sprains: Epidemiology, Anatomy and Injury Mechanism
- Affiliations
-
- 1Department of Orthopaedic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. kissung@gmail.com
- KMID: 2185238
- DOI: http://doi.org/10.4055/jkoa.2014.49.1.1
Abstract
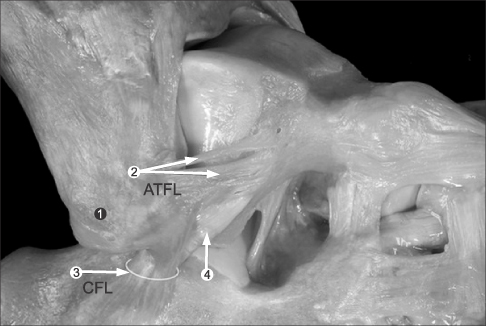
- Ankle sprain is one of the most common musculoskeletal injuries, nearly half of all ankle sprains occur during athletic activity. With a high incidence, as many as 40% of patients may experience residual discomfort including pain and instability, underscoring the importance of proper treatment and effective strategies for prevention. The stability of the ankle joint is maintained by both bony structure and ligamentous complex. The anterior talofibular ligament is the primary restraint of internal rotation and adduction of the talus with the ankle joint unloaded, while both bony mortise structure and calcaneofibular ligament restrict adduction of the talus with the ankle joint loaded. Plantar flexion and inversion is the most common mechanism of ankle sprains, which lead to injury of the anterior talofibular ligament followed by calcaneofibular ligament. Ligament injuries are classified according to three grades based on the extent of rupture and the severity of clinical features. Associated injuries with lateral ankle sprain include peroneus tendon rupture, osteochondral fracture, deltoid ligament injury, syndesmosis injury, and nerve traction injuries.
Keyword
MeSH Terms
Figure
Reference
-
1. Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ Jr. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010; 92:2279–2284.
Article2. Kannus P, Renström P. Treatment for acute tears of the lateral ligaments of the ankle. Operation, cast, or early controlled mobilization. J Bone Joint Surg Am. 1991; 73:305–312.
Article3. Maehlum S, Daljord OA. Acute sports injuries in Oslo: a one-year study. Br J Sports Med. 1984; 18:181–185.
Article4. Lee KT, Kim JS, Young KW, et al. Chronic lateral ankle instability: Efficacy of combination of ankle arthroscopic exploration and modified brostrom operation. J Korean Foot Ankle Soc. 2010; 14:123–129.5. Milgrom C, Shlamkovitch N, Finestone A, et al. Risk factors for lateral ankle sprain: a prospective study among military recruits. Foot Ankle. 1991; 12:26–30.
Article6. Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998; 19:653–660.
Article7. Anderson ME. Reconstruction of the lateral ligaments of the ankle using the plantaris tendon. J Bone Joint Surg Am. 1985; 67:930–934.
Article8. Schaap GR, de Keizer G, Marti K. Inversion trauma of the ankle. Arch Orthop Trauma Surg. 1989; 108:273–275.
Article9. Staples OS. Result study of ruptures of lateral ligaments of the ankle. Clin Orthop Relat Res. 1972; 85:50–58.
Article10. Konradsen L, Bech L, Ehrenbjerg M, Nickelsen T. Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports. 2002; 12:129–135.
Article11. van Rijn RM, van Os AG, Bernsen RM, Luijsterburg PA, Koes BW, Bierma-Zeinstra SM. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Med. 2008; 121:324–331.
Article12. Linde F, Hvass I, Jürgensen U, Madsen F. Early mobilizing treatment in lateral ankle sprains. Course and risk factors for chronic painful or function-limiting ankle. Scand J Rehabil Med. 1986; 18:17–21.13. Kjaersgaard-Andersen P, Wethelund JO, Helmig P, Nielsen S. Effect of the calcaneofibular ligament on hindfoot rotation in amputation specimens. Acta Orthop Scand. 1987; 58:135–138.14. Kjaersgaard-Andersen P, Wethelund JO, Nielsen S. Lateral talocalcaneal instability following section of the calcaneofibular ligament: a kinesiologic study. Foot Ankle. 1987; 7:355–361.
Article15. Coughlin MJ, Mann RA, Saltzman CL. Surgery of the foot and ankle. 8th ed. Philadelphia: Mosby Elsvier;2007. p. 1453.16. Attarian DE, McCrackin HJ, DeVito DP, McElhaney JH, Garrett WE Jr. Biomechanical characteristics of human ankle ligaments. Foot Ankle. 1985; 6:54–58.
Article17. Rasmussen O. Stability of the ankle joint. Analysis of the function and traumatology of the ankle ligaments. Acta Orthop Scand Suppl. 1985; 211:1–75.18. Berg EE. The symptomatic os subfibulare. Avulsion fracture of the fibula associated with recurrent instability of the ankle. J Bone Joint Surg Am. 1991; 73:1251–1254.
Article19. Heilman AE, Braly WG, Bishop JO, Noble PC, Tullos HS. An anatomic study of subtalar instability. Foot Ankle. 1990; 10:224–228.
Article20. Jackson DW, Ashley RL, Powell JW. Ankle sprains in young athletes. Relation of severity and disability. Clin Orthop Relat Res. 1974; 101:201–215.21. Hertel J. Functional instability following lateral ankle sprain. Sports Med. 2000; 29:361–371.
Article22. Richie DH Jr. Functional instability of the ankle and the role of neuromuscular control: a comprehensive review. J Foot Ankle Surg. 2001; 40:240–251.
Article23. O'Neill PJ, Parks BG, Walsh R, Simmons LM, Miller SD. Excursion and strain of the superficial peroneal nerve during inversion ankle sprain. J Bone Joint Surg Am. 2007; 89:979–986.24. Nitz AJ, Dobner JJ, Kersey D. Nerve injury and grades II and III ankle sprains. Am J Sports Med. 1985; 13:177–182.
Article25. Johnston EC, Howell SJ. Tension neuropathy of the superficial peroneal nerve: associated conditions and results of release. Foot Ankle Int. 1999; 20:576–582.
Article26. Mizel MS, Hecht PJ, Marymont JV, Temple HT. Evaluation and treatment of chronic ankle pain. Instr Course Lect. 2004; 53:311–321.
Article