J Korean Orthop Assoc.
2014 Aug;49(4):278-284. 10.4055/jkoa.2014.49.4.278.
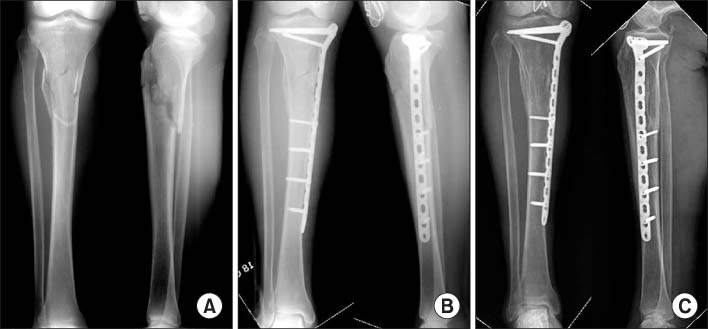
Medial Minimally Invasive Percutaneous Plate Osteosynthesis in Proximal Tibial Comminuted Fractures
- Affiliations
-
- 1Department of Orthopedic Surgery, Gachon University School of Medicine, Incheon, Korea. bklee@gilhospital.com
- 2Department of Orthopedic Surgery, Sokcho Medical Center, Sokcho, Korea.
- KMID: 2185183
- DOI: http://doi.org/10.4055/jkoa.2014.49.4.278
Abstract
- PURPOSE
This goal of this study is to evaluate the clinical and radiological outcomes of proximal tibial comminuted fractures treated with medial minimally invasive percutaneous plate osteosynthesis (MIPPO).
MATERIALS AND METHODS
We evaluated 43 patients who underwent medial MIPPO from February 2008 to February 2012 and were followed up for more than one year. According to the AO/OTA classification, there were 30 patients of 41-A3 and 13 patients of 41-C2. Thirty-six patients had closed fractures and seven patients had open fractures. We assessed clinical outcomes, radiologic results and postoperative complications.
RESULTS
All fractures were united at an average of 18.3+/-8.1 weeks except three patients with nonunion. According to Schatzker and Lambert assessment, excellent results were achieved for 22 patients and good results were achieved for 21 patients. The average tibial plateau angle was 89.1degrees+/-2.7degrees and the average posterior tibial slope angle was 10.5degrees+/-4.6degrees. In assessment of lower limb alignment, the average femorotibial angle was 175.1degrees+/-2.9degrees and the mean deviation of mechanical axis was 46.5%+/-12.7%. In terms of complications, three patients had nonunion, but complete bony union was achieved by autogenous cancellous bone grafting. Seven patients complained of skin irritation around the plate. However, there was no skin necrosis, infection, or limited range of motion in seven patients with skin irritation.
CONCLUSION
Medial MIPPO for proximal tibial comminuted fractures provides favorable clinical outcomes and good radiological alignments.
MeSH Terms
Figure
Reference
-
1. Cole JD. Intramedullary fixation of proximal tibia fractures. Tech Orthop. 1998; 13:27–37.
Article2. Dendrinos GK, Kontos S, Katsenis D, Dalas A. Treatment of high-energy tibial plateau fractures by the Ilizarov circular fixator. J Bone Joint Surg Br. 1996; 78:710–717.
Article3. Lang GJ, Cohen BE, Bosse MJ, Kellam JF. Proximal third tibial shaft fractures. Should they be nailed? Clin Orthop Relat Res. 1995; 315:64–74.4. Spagnolo R, Pace F. Management of the Schatzker VI fractures with lateral locked screw plating. Musculoskelet Surg. 2012; 96:75–80.
Article5. Whiteside LA, Lesker PA. The effects of extraperiosteal and subperiosteal dissection. II. On fracture healing. J Bone Joint Surg Am. 1978; 60:26–30.
Article6. Lachiewicz PF, Funcik T. Factors influencing the results of open reduction and internal fixation of tibial plateau fractures. Clin Orthop Relat Res. 1990; 259:210–215.
Article7. Littenberg B, Weinstein LP, McCarren M, et al. Closed fractures of the tibial shaft. A meta-analysis of three methods of treatment. J Bone Joint Surg Am. 1998; 80:174–183.8. Cole PA, Zlowodzki M, Kregor PJ. Treatment of proximal tibia fractures using the less invasive stabilization system: surgical experience and early clinical results in 77 fractures. J Orthop Trauma. 2004; 18:528–535.9. Ha SH, Kim DH, Lee JY. Treatment of proximal tibia fractures using LCP by MIPO technique. J Korean Fract Soc. 2010; 23:34–41.
Article10. Byun YS, Park KC, Bong HJ, Lee CH. Minimally invasive plate osteosynthesis for proximal tibial shaft fracture. J Korean Fract Soc. 2011; 24:23–27.
Article11. Park KC. Proximal tibia fracture: plating. J Korean Fract Soc. 2009; 22:206–213.
Article12. Oh CW, Oh JK, Jeon IH, et al. Minimally invasive percutaneous plate stabilization of proximal tibial fractures. J Korean Fract Soc. 2004; 17:224–229.
Article13. Mullaji AB, Padmanabhan V, Jindal G. Total knee arthroplasty for profound varus deformity: technique and radiological results in 173 knees with varus of more than 20 degrees. J Arthroplasty. 2005; 20:550–561.14. Sim JA, Lee BK, Kim KH, Lee YS. Minimally invasive percutaneous plate stabilization using a medial locking plate for proximal tibial fractures: technical note. J Korean Fract Soc. 2013; 26:327–332.15. Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007; 21:S1–S133.16. Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976; 58:453–458.17. Schatzker J, Lambert DC. Supracondylar fractures of the femur. Clin Orthop Relat Res. 1979; 138:77–83.
Article18. Bauer GC, Insall J, Koshino T. Tibial osteotomy in gonarthrosis (osteo-arthritis of the knee). J Bone Joint Surg Am. 1969; 51:1545–1563.
Article19. Sim JA, Kwak JH, Yang SH, Choi ES, Lee BK. Effect of weight-bearing on the alignment after open wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2010; 18:874–878.
Article20. Kim DK, Lee BK, Sim JA. A short term follow-up of open wedge high tibial osteotomyusing locking compression plate(R). J Korean Orthop Assoc. 2007; 42:84–90.21. Oh CW, Oh JK, Jeon IH, et al. Double plating of proximal tibial fractures using minimally invasive percutaneous osteosynthesis technique. J Korean Fract Soc. 2005; 18:250–255.
Article22. Chae IJ, Park SW, Lee SH, Noh W, Kim HJ, Hahn SB. Treatment of shatzker type VI tibia plateau fracture using lateral and posteromedial dual incision approach and dual plating. J Korean Fract Soc. 2009; 22:252–258.
Article23. Egol KA, Su E, Tejwani NC, Sims SH, Kummer FJ, Koval KJ. Treatment of complex tibial plateau fractures using the less invasive stabilization system plate: clinical experience and a laboratory comparison with double plating. J Trauma. 2004; 57:340–346.
Article24. Ali AM, Saleh M, Bolongaro S, Yang L. The strength of different fixation techniques for bicondylar tibial plateau fractures: a biomechanical study. Clin Biomech (Bristol, Avon). 2003; 18:864–870.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Percutaneous Plate Stabilization Using a Medial Locking Plate for Proximal Tibial Fractures: Technical Note
- Minimally Invasive Percutaneous Plate Osteosynthesis Using a Lateral Plate in Distal Tibial Fracture
- Minimally Invasive Percutaneous Plate Osteosynthesis Using Periarticular Plate for Distal Tibial Fractures
- Minimally Invasive Plate Osteosynthesis for Periarticular Tibial Fractures
- Minimally Invasive Percutaneous Plate Stabilization of Proximal Tibial Fractures