J Korean Orthop Assoc.
2015 Oct;50(5):412-417. 10.4055/jkoa.2015.50.5.412.
Complete Rupture of the Tibialis Anterior Tendon Due to Intratendinous Ganglion Cyst
- Affiliations
-
- 1Department of Orthopaedic Surgery, Wonkwang University School of Medicine, Iksan, Korea. kanghongje@hanmail.net
- KMID: 2185105
- DOI: http://doi.org/10.4055/jkoa.2015.50.5.412
Abstract
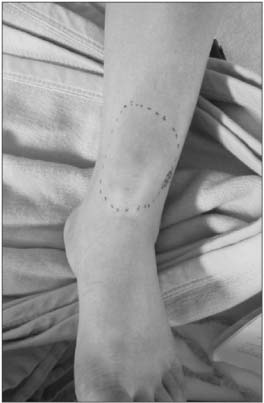
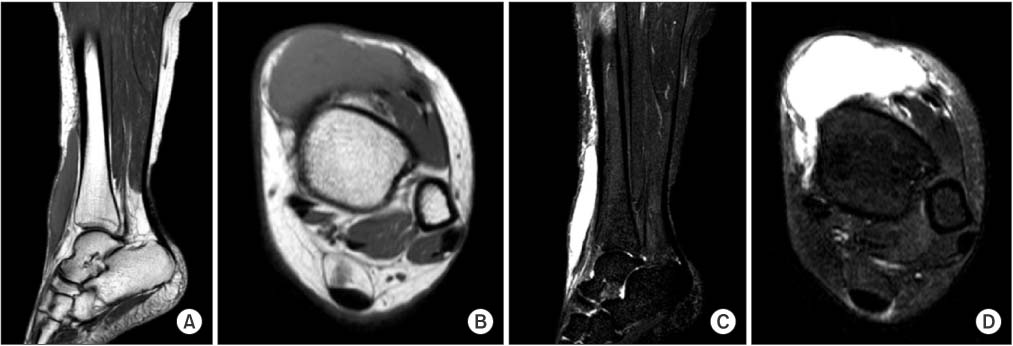
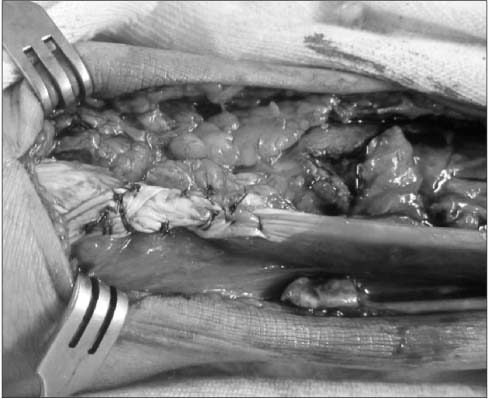
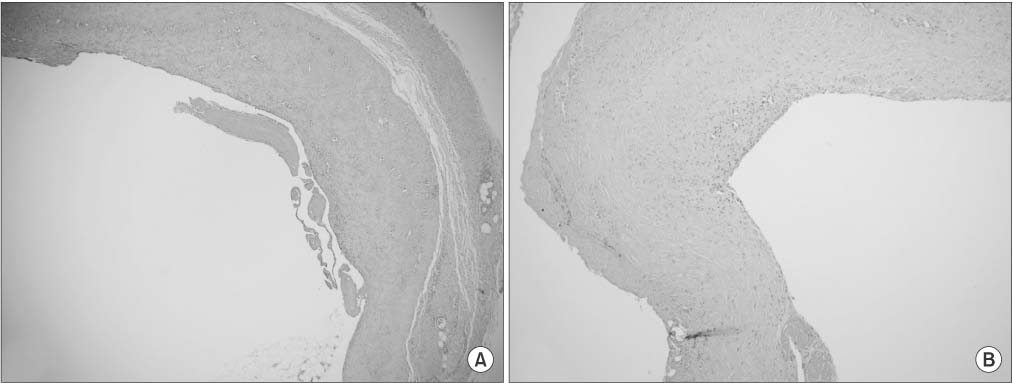
- Spontaneous rupture of the tibialis anterior tendon is rare among ordinary people. The tendon rupture usually occurs in patients iatrogenically after local steroid injection to the tendon or with pre-existing systemic disease such as diabetes mellitus, gout, and rheumatic disease. However, no case of complete rupture of the tibialis anterior tendon due to an intratendinous ganglion cyst has been reported. We report on a case of a 39-year-old female with spontaneous rupture of the tibialis anterior tendon due to intratendinous ganglion cyst and her clinical results.
MeSH Terms
Figure
Cited by 1 articles
-
Chronic Longitudinal Rupture of the Tibialis Anterior Tendon: A Case Report
Jiyoun Kim
J Korean Foot Ankle Soc. 2023;27(3):99-102. doi: 10.14193/jkfas.2023.27.3.99.
Reference
-
1. Jerome JT, Varghese M, Sankaran B, Thomas S, Thirumagal SK. Tibialis anterior tendon rupture in gout--case report and literature review. Foot Ankle Surg. 2008; 14:166–169.2. Sapkas GS, Tzoutzopoulos A, Tsoukas FC, Triantafillopoulos IK. Spontaneous tibialis anterior tendon rupture: delayed repair with free-sliding tibialis anterior tendon graft. Am J Orthop (Belle Mead NJ). 2008; 37:E213–E216.3. Khoury NJ, el-Khoury GY, Saltzman CL, Brandser EA. Rupture of the anterior tibial tendon: diagnosis by MR imaging. AJR Am J Roentgenol. 1996; 167:351–354.4. DiDomenico LA, Williams K, Petrolla AF. Spontaneous rupture of the anterior tibial tendon in a diabetic patient: results of operative treatment. J Foot Ankle Surg. 2008; 47:463–467.5. Aydingöz U, Aydingöz O. Spontaneous rupture of the tibialis anterior tendon in a patient with psoriasis. Clin Imaging. 2002; 26:209–211.6. Markarian GG, Kelikian AS, Brage M, Trainor T, Dias L. Anterior tibialis tendon ruptures: an outcome analysis of operative versus nonoperative treatment. Foot Ankle Int. 1998; 19:792–802.7. Waldecker U. Unusual location of a posttraumatic ganglion and rupture of the peroneus brevis tendon: a case report. J Foot Ankle Surg. 2005; 44:163–165.8. Petersen W, Stein V, Tillmann B. Blood supply of the tibialis anterior tendon. Arch Orthop Trauma Surg. 1999; 119:371–375.9. Sammarco VJ, Sammarco GJ, Henning C, Chaim S. Surgical repair of acute and chronic tibialis anterior tendon ruptures. J Bone Joint Surg Am. 2009; 91:325–332.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chronic Longitudinal Rupture of the Tibialis Anterior Tendon: A Case Report
- Intratendinous Ganglion: A Case Report
- Using Acellular Dermal Matrix to Treat Repetitive Tendon Rupture after Excision of Ruptured Intratendinous Ganglion
- Clinical Features of Tibialis Anterior Tendon Rupture
- Clinical Experience of Intratendinous Ganglion in the Extensor Tendon of Hand