J Korean Med Assoc.
2007 Jun;50(6):523-532. 10.5124/jkma.2007.50.6.523.
Surgical Management of Chronic Low Back Pain
- Affiliations
-
- 1Department of Neurosurgery, Seoul National Univeristy College of Medicie, Korea. taj@snu.ac.kr
- KMID: 2184861
- DOI: http://doi.org/10.5124/jkma.2007.50.6.523
Abstract
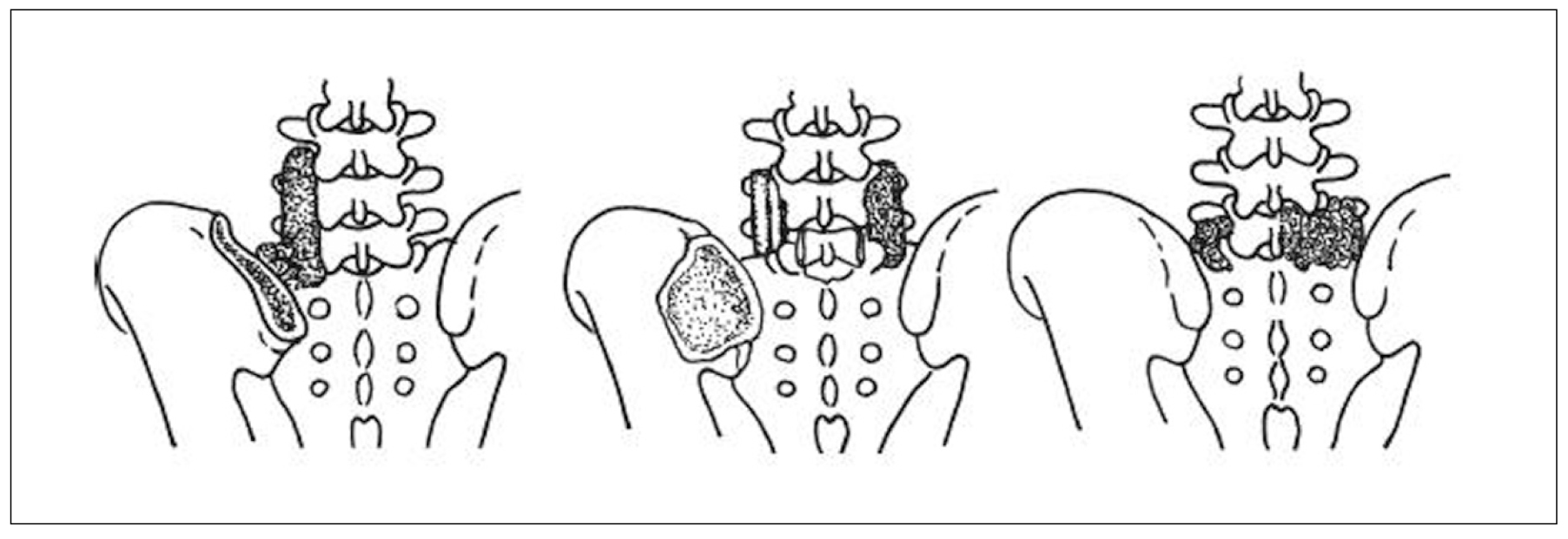
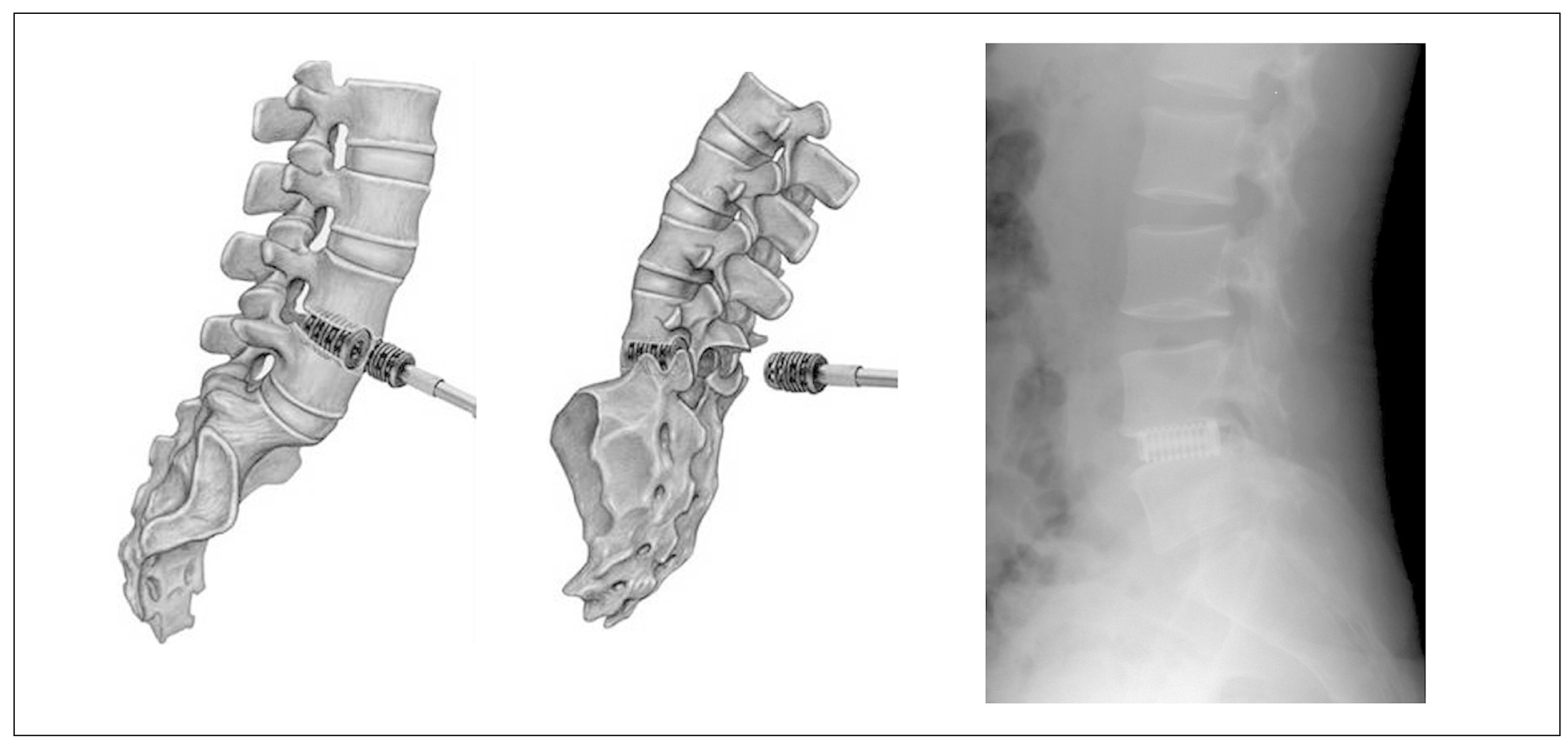
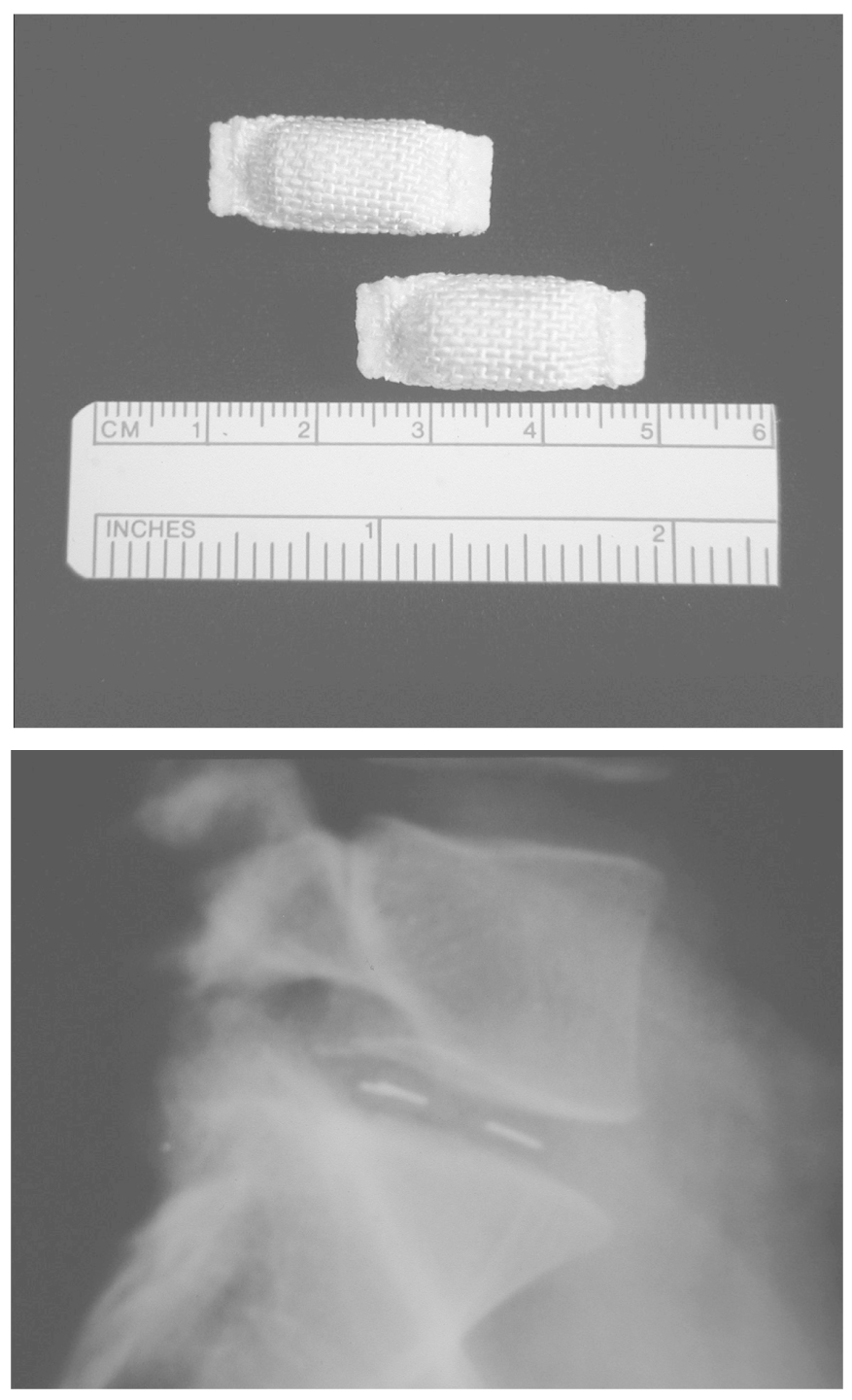
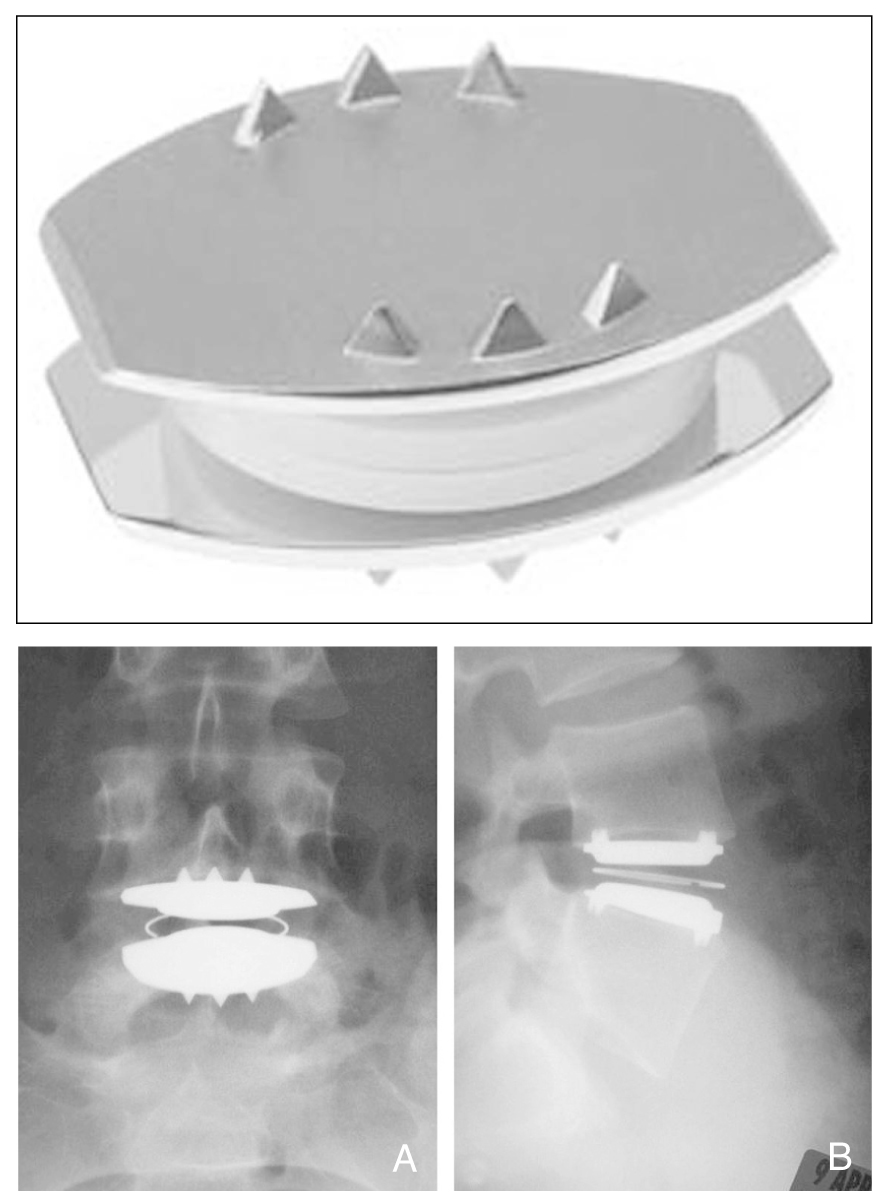
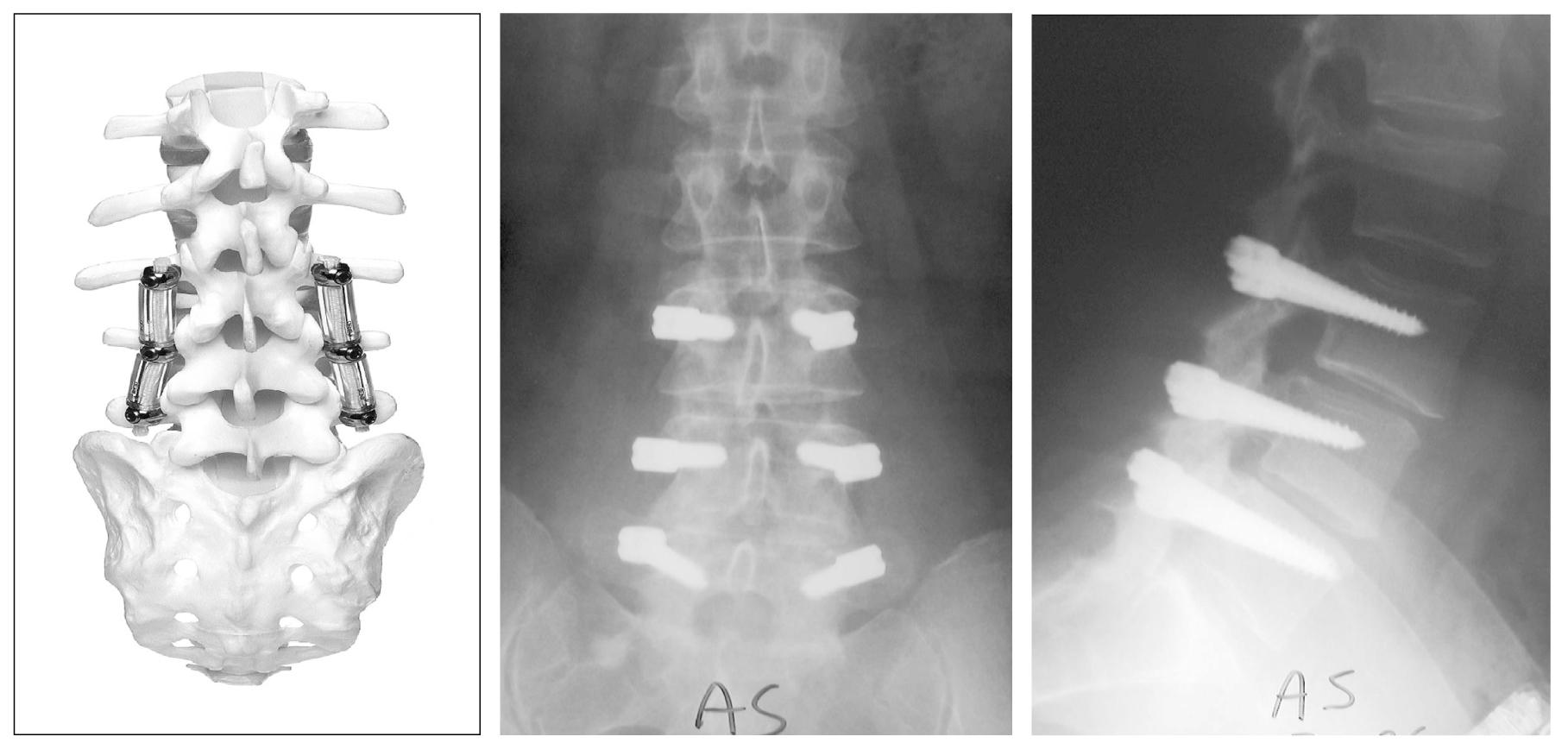
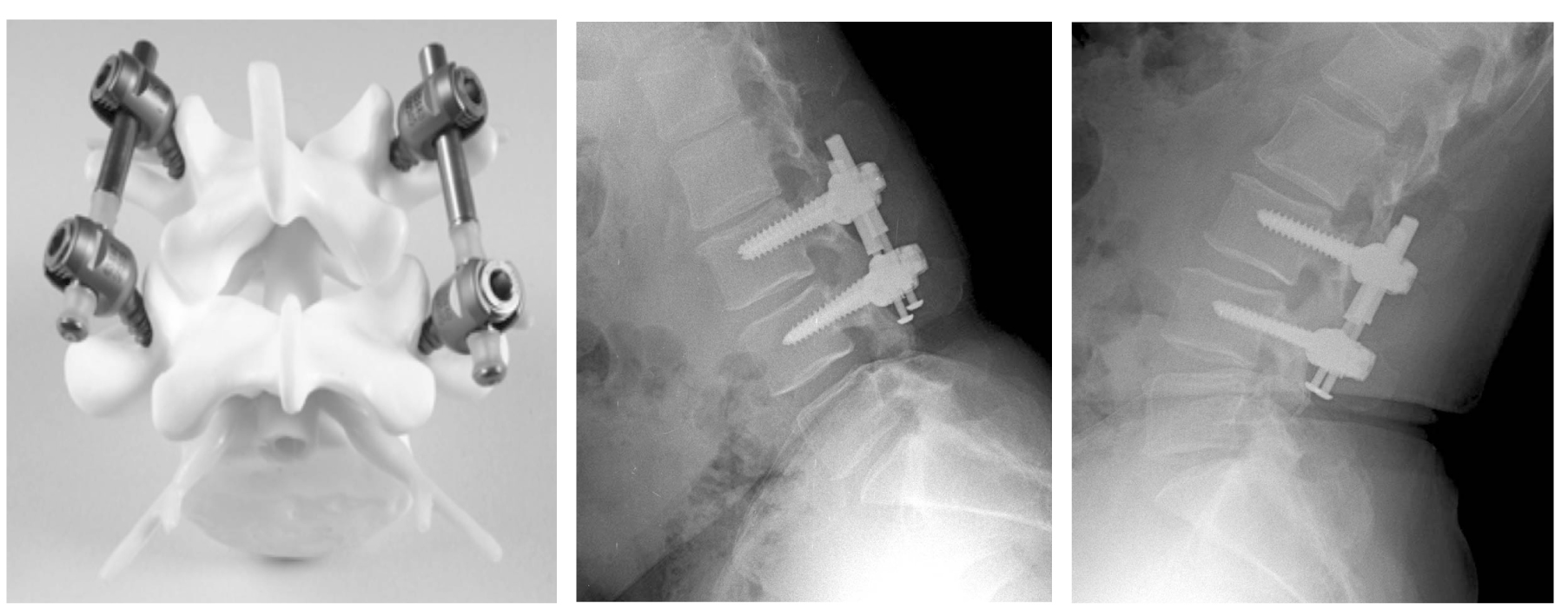
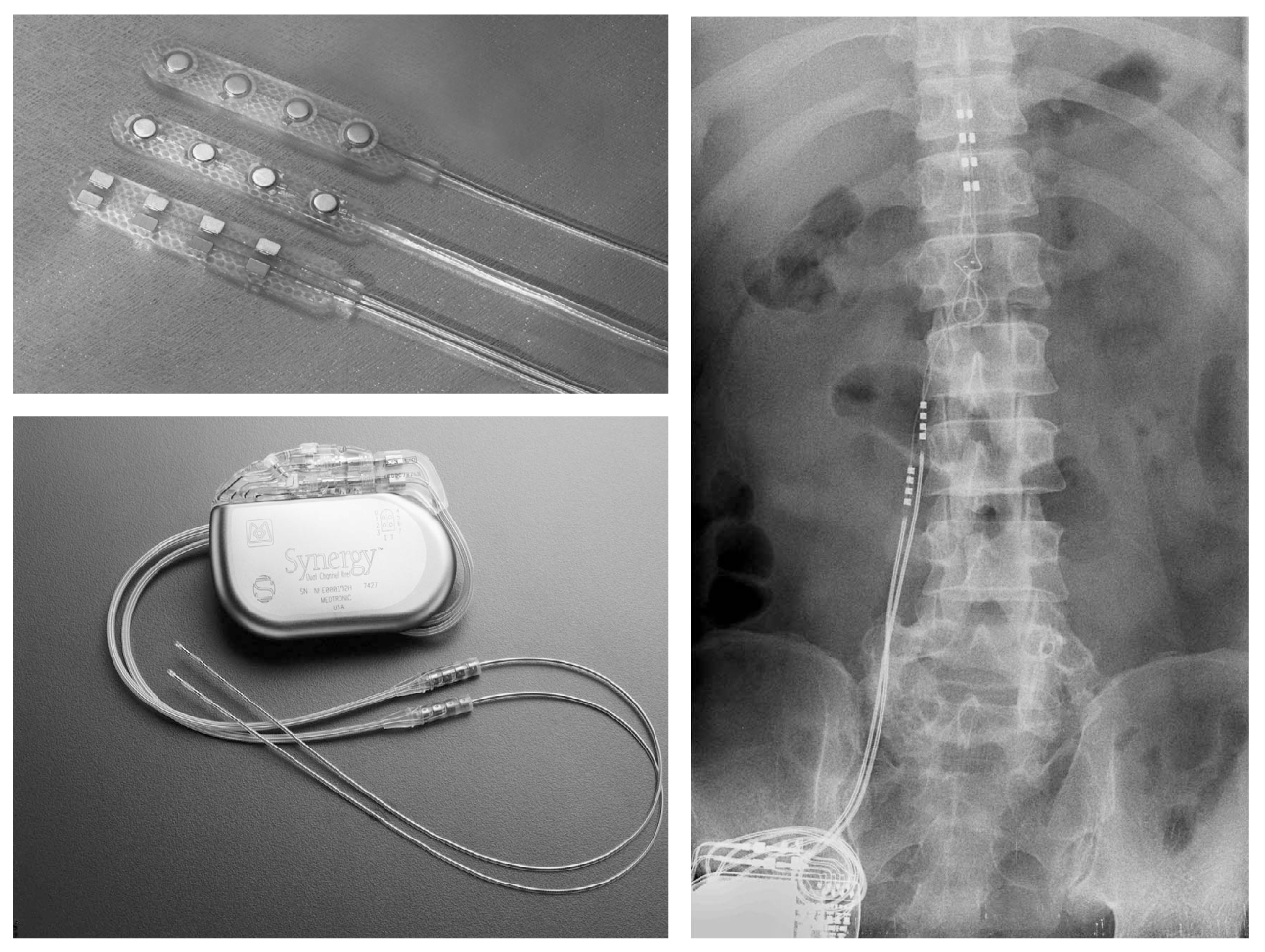
- Conservative therapy remains the mainstay treatment of chronic low back pain (LBP). If this has failed, surgical options may be considered in carefully selected patients. Still surgical treatment for chronic LBP is a matter of intensive and controversial discussions. Nevertheless, surgical management for chronic (LBP) has been evolved and increased gradually. Spinal fusion has been the established surgical option in cases that did not respond to conservative therapy. Besides spinal fusion, newer technologies such as artificial disc replacement, dynamic stabilization, and spinal cord stimulation are being increasingly considered. Although successful results of these procedures have been published, evidence-based data on the efficacy and benefits of most of these techniques are still lacking. However, empirical data show good or at least satisfactory clinical results of these procedures when they were applied under restrictive indication criteria. Further prospective randomized controlled studies are mandatory to determine the role of these procedures, and basic research is necessary to understand the pathogenesis of LBP at the molecular and genetic levels
Keyword
Figure
Cited by 1 articles
-
The Effects of Comprehensive Education Program on Anxiety, Uncertainty and Athletic Performance of Patients undergo Spinal Nerve Block
Seon Hee Kim, Eun Sook Lee
Korean J Adult Nurs. 2017;29(2):143-153. doi: 10.7475/kjan.2017.29.2.143.
Reference
-
1. Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999. 354:581–585.
Article2. Barolat G. Current state of spinal cord stimulation. Neurosurg Q. 1995. 5:11–23.3. Bertagnoli R, Kumar S. Indications for full prosthetic disc arthroplasty: a correlation of clinical outcome against a variety of indications. Eur Spine J. 2002. 11:S131–S136.
Article4. Booth KC, Bridwell KH, Lenke LG, Baldus CR, Blanke KM. Complications and predictive factors for the successful treatment of flatback deformity (fixed sagittal imbalance). Spine. 1999. 24:1712–1720.
Article5. Brox JI, Sorensen R, Friis A, Nygaard O, Indahl A, Keller A, Ingebrigtsen T, Eriksen HR, Holm I, Koller AK, Riise R, Reikeras O. Randomized clinical trial of lumbar instrumented fusion and cognitive intervention and exercises in patients with chronic low back pain and disc degeneration. Spine. 2003. 28:1913–1921.
Article6. Cameron T. Safety and efficacy of spinal cord stimulation for the treatment of chronic pain: a 20-year literature review. J Neurosurg(Spine). 2004. 100:254–267.
Article7. Danielsson AJ, Nachemson AL. Radiologic findings and curve progression 22 years after treatment for adolescent idiopathic scoliosis: comparison of brace and surgical treatment with matching control group of straight individuals. Spine. 2001. 26:516–525.
Article8. Delamarter RB, Fribourg DM, Kanim LE, Bae H. ProDisc artificial total lumbar disc replacement: introduction and early results from the United States clinical trial. Spine. 2003. 28:S167–S175.
Article9. Deyo RA, Nachemson A, Mirza SK. Spinal-fusion surgery-the case for restraint. N Engl J Med. 2004. 350:722–726.
Article10. Frelinghuysen P, Huang RC, Girardi FP, Cammisa FP Jr. Lumbar total disc replacement part I: rationale, biomechanics, and implant types. Orthop Clin North Am. 2005. 36:293–299.
Article11. Fritzell P, Hagg O, Wessberg P, Nordwall A. Swedish Lumbar Spine Study Group. 2001 Volvo Award Winner in Clinical Studies: Lumbar fusion versus nonsurgical treatment for chronic low back pain: a multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine. 2001. 26:2521–2532.
Article12. Geisler FH, Blumenthal SL, Guyer RD, McAfee PC, Regan JJ, Johnson JP, Mullin B. Neurological complications of lumbar artificial disc replacement and comparison of clinical results with those related to lumbar arthrodesis in the literature: results of a multicenter, prospective, randomized investigational device exemption study of Charite intervertebral disc. J Neurosurg Spine. 2004. 1:143–154.
Article13. German JW, Foley KT. Disc arthroplasty in the management of the painful lumbar motion segment. Spine. 2005. 30:S60–S67.
Article14. Grob D, Benini A, Junge A, Mannion AF. Clinical experience with the Dynesys semirigid fixation system for the lumbar spine: surgical and patient-oriented outcome in 50 cases after an average of 2 years. Spine. 2005. 30:324–331.
Article15. Hashimoto T, Oha F, Shigenobu K, Kanayama M, Harada M, Ohkoshi Y, Tada H, Yamamoto K, Yamane S. Mid-term clinical results of Graf stabilization for lumbar degenerative pathologies. a minimum 2-year follow-up. Spine J. 2001. 1:283–289.
Article16. Hoppenstein R. Electrical stimulation of the ventral and dorsal columns of the spinal cord for relief of chronic intractable pain: preliminary report. Surg Neurol. 1975. 4:187–194.17. Kumar MN, Jacquot F, Hall H. Long-term follow-up of functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease. Eur Spine J. 2001. 10:309–313.
Article18. Lee CK. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine. 1988. 13:375–377.
Article19. Le Huec JC, Mathews H, Basso Y, Aunoble S, Hoste D, Bley B, Friesem T. Clinical results of Maverick lumbar total disc replacement: two-year prospective follow-up. Orthop Clin North Am. 2005. 36:315–322.
Article20. Lemaire JP, Carrier H, Sariali el H, Skalli W, Lavaste F. Clinical and radiological outcomes with the Charite artificial disc: a 10-year minimum follow-up. J Spinal Disord Tech. 2005. 18:353–359.21. Madan SS, Boeree NR. Comparison of instrumented anterior interbody fusion with instrumented circumferential lumbar fusion. Eur Spine J. 2003. 12:567–575.
Article22. Mulholland RC, Sengupta DK. Rationale, principles and experimental evaluation of the concept of soft stabilization. Eur Spine J. 2002. 11:S198–S205.
Article23. North RB, Kidd DH, Farrokhi F, Piantadosi SA. Spinal cord stimulation versus repeated lumbosacral spine surgery for chronic pain: a randomized, controlled trial. Neunaurgery. 2005. 56:98–106.
Article24. Oakley JC, Weiner RL. Spinal cord stimulation for complex regional pain syndrome: a prospective study at two centers. Neuromodulation. 1999. 5:47–50.25. Ohnmeiss DD, Rashbaum RF. Patient satisfaction with spinal cord stimulation for predominant complaints of chronic, intractable low back pain. Spine J. 2001. 1:358–363.
Article26. Resnick DK, Choudhri TF, Dailey AT, Groff MW, Khoo L, Matz PG, Mummaneni P, Watters WC 3rd, Wang J, Walters BC, Hadley MN. Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 7: intractable low-back pain without stenosis or spondylolisthesis. J Neurosurg Spine. 2005. 2:670–672.
Article27. Senegas L. Mechanical supplementation by non-rigid fixation in degenerative intervertebral lumbar segments: the Wallis system. Eur Spine J. 2002. 11:S164–S169.
Article28. Sengupta DK. Dynamic stabilization devices in the treatment of low back pain. Orthop Clin North Am. 2004. 35:43–56.
Article29. Simpson AK, Cholewicki J, Grauer J. Chronic low back pain. Curr Pain Headache Rep. 2006. 10:431–436.
Article30. Stoll TM, Dubois G, Schwarzenbach O. The dynamic neutralization system for the spine: a multi-center study of a novel non-fusion system. Eur Spine J. 2002. 11:S170–S178.
Article31. Errico Thomas J. Lumbar disc arthroplasy. Clinical Orthopaedics and related research. 2005. 435:106–117.32. Turner JA, Ersek M, Herron L, Haselkorn J, Kent D, Ciol MA, Deyo R. Patient outcomes after lumbar spinal fusions. JAMA. 1992. 268:907–911.
Article33. van Tulder MW, Koes B, Malmivaara A. Outcome of non-invasive treatment modalities on back pain: an evidence-based review. Eur Spine J. 2006. 15:S64–S81.
Article34. Zigler JE. Clinical results with ProDisc: European experience and U.S. investigation device exemption study. Spine. 2003. 28:S163–S166.
Article35. Zigler JE. Lumbar spine arthroplasty using the ProDisc II. Spine J. 2004. 4:S260–S267.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Oceupational Chronic Low Baek Pain: A Case Report
- Interventional therapy for chronic low back pain
- Treatment of Chronic Low Back and Leg Pain Using a Spinal Cord Stimulator: Two case reports
- Intradiscal Electrothermal Annuloplasty in Chronic Discogenic Low Back Pain
- Surgical Treatment of Degenerative Lumbar Disc Disease