J Clin Neurol.
2013 Apr;9(2):97-102. 10.3988/jcn.2013.9.2.97.
Hemispheric Differences in Ischemic Stroke: Is Left-Hemisphere Stroke More Common?
- Affiliations
-
- 1Department of Neurology, University of Florida, Gainesville, FL, USA. vhedna@mail.ufl.edu
- 2Department of Emergency Medicine, University of Florida, Gainesville, FL, USA.
- 3Department of Neurosciences, University of Florida, Gainesville, FL, USA.
- 4Department of Neurosurgery, University of Florida, Gainesville, FL, USA.
- KMID: 2179168
- DOI: http://doi.org/10.3988/jcn.2013.9.2.97
Abstract
- BACKGROUND AND PURPOSE
Understanding the mechanisms underlying stroke can aid the development of therapies and improve the final outcome. The purposes of this study were to establish whether there are characteristic mechanistic differences in the frequency, severity, functional outcome, and mortality between left- and right-hemisphere ischemic stroke and, given the velocity differences in the carotid circulation and direct branching of the left common carotid artery from the aorta, whether large-vessel ischemia (including cardioembolism) is more common in the territory of the left middle cerebral artery.
METHODS
Trial cohorts were combined into a data set of 476 samples. Using Trial of Org 10172 in Acute Stroke Treatment criteria, ischemic strokes in a total 317 patients were included in the analysis. Hemorrhagic stroke, stroke of undetermined etiology, cryptogenic stroke, and bilateral ischemic strokes were excluded. Laterality and vascular distribution were correlated with outcomes using a logistic regression model. The etiologies of the large-vessel strokes were atherosclerosis and cardioembolism.
RESULTS
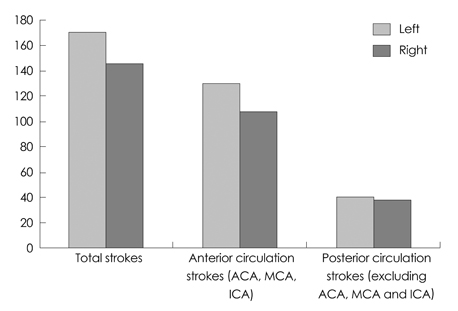
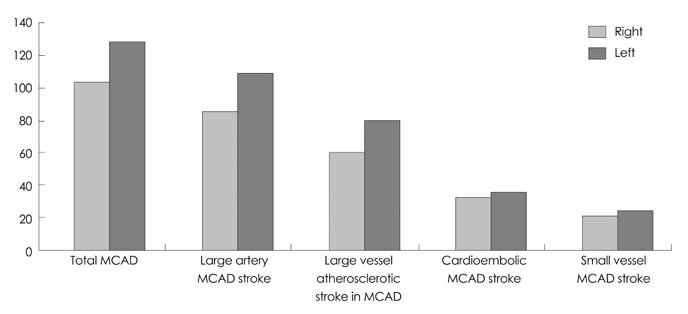
The overall event frequency, mortality, National Institutes of Health Stroke Scale (NIHSS) score, Glasgow Coma Scale score, and rate of mechanical thrombectomy interventions differed significantly between the hemispheres. Left-hemispheric strokes (54%) were more common than right-hemispheric strokes (46%; p=0.0073), and had higher admission NIHSS scores (p=0.011), increased mortality (p=0.0339), and higher endovascular intervention rates (p< or =0.0001). ischemic strokes were more frequent in the distribution of the left middle cerebral artery (122 vs. 97; p=0.0003) due to the higher incidence of large-vessel ischemic stroke in this area (p=0.0011).
CONCLUSIONS
Left-hemispheric ischemic strokes appear to be more frequent and often have a worse outcome than their right-hemispheric counterparts. The incidence of large-vessel ischemic strokes is higher in the left middle cerebral artery distribution, contributing to these hemispheric differences. The hemispheric differences exhibit a nonsignificant trend when strokes in the middle cerebral artery distribution are excluded from the analysis.
Keyword
MeSH Terms
Figure
Reference
-
1. Cassvan A, Ross PL, Dyer PR, Zane L. Lateralization in stroke syndromes as a factor in ambulation. Arch Phys Med Rehabil. 1976. 57:583–587.2. Naess H, Waje-Andreassen U, Thomassen L, Myhr KM. High incidence of infarction in the left cerebral hemisphere among young adults. J Stroke Cerebrovasc Dis. 2006. 15:241–244.
Article3. Rodríguez Hernández SA, Kroon AA, van Boxtel MP, Mess WH, Lodder J, Jolles J, et al. Is there a side predilection for cerebrovascular disease? Hypertension. 2003. 42:56–60.
Article4. Woo D, Broderick JP, Kothari RU, Lu M, Brott T, Lyden PD, et al. NINDS t-PA Stroke Study Group. Does the National Institutes of Health Stroke Scale favor left hemisphere strokes? Stroke. 1999. 30:2355–2359.
Article5. Fink JN, Selim MH, Kumar S, Silver B, Linfante I, Caplan LR, et al. Is the association of National Institutes of Health Stroke Scale scores and acute magnetic resonance imaging stroke volume equal for patients with right- and left-hemisphere ischemic stroke? Stroke. 2002. 33:954–958.
Article6. Grau AJ, Weimar C, Buggle F, Heinrich A, Goertler M, Neumaier S, et al. Risk factors, outcome, and treatment in subtypes of ischemic stroke: the German stroke data bank. Stroke. 2001. 32:2559–2566.
Article7. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993. 24:35–41.
Article8. Fink JN, Frampton CM, Lyden P, Lees KR. Virtual International Stroke Trials Archive Investigators. Does hemispheric lateralization influence functional and cardiovascular outcomes after stroke?: an analysis of placebo-treated patients from prospective acute stroke trials. Stroke. 2008. 39:3335–3340.
Article9. Di Legge S, Saposnik G, Nilanont Y, Hachinski V. Neglecting the difference: does right or left matter in stroke outcome after thrombolysis? Stroke. 2006. 37:2066–2069.10. Rothrock JF, Lyden PD, Hesselink JR, Brown JJ, Healy ME. Brain magnetic resonance imaging in the evaluation of lacunar stroke. Stroke. 1987. 18:781–786.
Article11. Arditi H, Feldman R, Hammerman C, Eidelman AI. Cerebral blood flow velocity asymmetry, neurobehavioral maturation, and the cognitive development of premature infants across the first two years. J Dev Behav Pediatr. 2007. 28:362–368.
Article12. DeCarli C, Kawas C, Morrison JH, Reuter-Lorenz PA, Sperling RA, Wright CB. Session II: Mechanisms of age-related cognitive change and targets for intervention: neural circuits, networks, and plasticity. J Gerontol A Biol Sci Med Sci. 2012. 67:747–753.
Article13. Ances BM, Liang CL, Leontiev O, Perthen JE, Fleisher AS, Lansing AE, et al. Effects of aging on cerebral blood flow, oxygen metabolism, and blood oxygenation level dependent responses to visual stimulation. Hum Brain Mapp. 2009. 30:1120–1132.
Article14. Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Executive summary: heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012. 125:188–197.15. Tsivgoulis G, Saqqur M, Sharma VK, Lao AY, Hill MD, Alexandrov AV, et al. Association of pretreatment blood pressure with tissue plasminogen activator-induced arterial recanalization in acute ischemic stroke. Stroke. 2007. 38:961–966.
Article16. Generalized efficacy of t-PA for acute stroke. Subgroup analysis of the NINDS t-PA Stroke Trial. Stroke. 1997. 28:2119–2125.17. Nogueira RG, Liebeskind DS, Sung G, Duckwiler G, Smith WS, et al. MERCI. Predictors of good clinical outcomes, mortality, and successful revascularization in patients with acute ischemic stroke undergoing thrombectomy: pooled analysis of the Mechanical Embolus Removal in Cerebral Ischemia (MERCI) and Multi MERCI Trials. Stroke. 2009. 40:3777–3783.
Article18. Wang RY, Wang PS, Yang YR. Effect of age in rats following middle cerebral artery occlusion. Gerontology. 2003. 49:27–32.
Article19. Khaw KT, Barrett-Connor E, Suarez L, Criqui MH. Predictors of stroke-associated mortality in the elderly. Stroke. 1984. 15:244–248.
Article