J Clin Neurol.
2013 Apr;9(2):91-96. 10.3988/jcn.2013.9.2.91.
A Comparison of Stent-Assisted Mechanical Thrombectomy and Conventional Intra-Arterial Thrombolysis for Acute Cerebral Infarction
- Affiliations
-
- 1Department of Neurology, Chungnam National University Hospital and School of Medicine, Daejeon, Korea. jeikim@cnu.ac.kr
- 2Department of Neurosurgery, Chungnam National University Hospital and School of Medicine, Daejeon, Korea. solesoul@hanmail.net
- 3Department of Information and Statistics, College of Natural Science, Chungnam National University, Daejeon, Korea.
- KMID: 2179167
- DOI: http://doi.org/10.3988/jcn.2013.9.2.91
Abstract
- BACKGROUND AND PURPOSE
We evaluated whether stent-assisted thrombectomy (SAT) is safer or more clinically beneficial than aggressive mechanical clot disruption (AMCD) for patients with acute intracranial artery occlusion.
METHODS
We retrospectively analyzed the clinical data of 72 patients (33 with SAT and 39 with AMCD) who underwent intra-arterial thrombolysis for acute intracranial artery occlusions. Procedure parameters, clinical outcomes, and incidence of complications were compared between the SAT and AMCD groups.
RESULTS
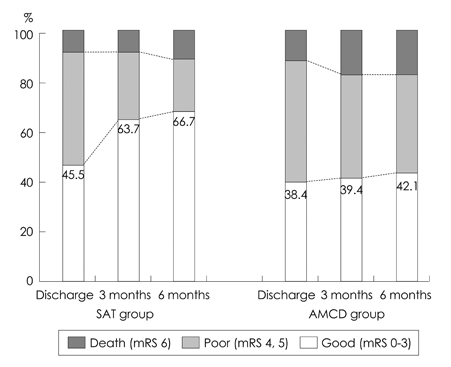
The time interval to recanalization was shorter in SAT patients (69.2+/-39.6 minutes, mean+/-standard deviation) than in AMCD patients (94.4+/-48.0 minutes, p<0.05). Recanalization was achieved in more SAT patients (91%) than AMCD patients (80%), but with no statistically significance. Urokinase was used less frequently in SAT patients (21%) than in AMCD patients (92%, p<0.05), and the incidence of symptomatic hemorrhages was lower in SAT patients (3%) than in AMCD patients (18%, p<0.05). Device-related complications in SAT patients comprised two cases of stent fracture and one case of distal migration of a captured thrombus. The proportion of patients with good outcomes, defined as scores from 0 to 3 on the modified Rankin Scale, was similar in the two groups at discharge (SAT, 46%; AMCD, 39%), but significantly higher in the SAT group than in the AMCD group at 3 months (64% vs. 40%, p<0.05) and 6 months (67% vs. 42%, p<0.05) after discharge.
CONCLUSIONS
The outcomes and clinical parameters were better for SAT during thrombolytic procedures for acute intracranial artery occlusions than for AMCD for up to 6 months. However, some device-related complications occurred during stent interventions.
MeSH Terms
Figure
Reference
-
1. Khatri P, Abruzzo T, Yeatts SD, Nichols C, Broderick JP, Tomsick TA, et al. Good clinical outcome after ischemic stroke with successful revascularization is time-dependent. Neurology. 2009. 73:1066–1072.
Article2. Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke. 2007. 38:967–973.
Article3. Linfante I, Llinas RH, Selim M, Chaves C, Kumar S, Parker RA, et al. Clinical and vascular outcome in internal carotid artery versus middle cerebral artery occlusions after intravenous tissue plasminogen activator. Stroke. 2002. 33:2066–2071.
Article4. Noser EA, Shaltoni HM, Hall CE, Alexandrov AV, Garami Z, Cacayorin ED, et al. Aggressive mechanical clot disruption: a safe adjunct to thrombolytic therapy in acute stroke? Stroke. 2005. 36:292–296.5. Sorimachi T, Fujii Y, Tsuchiya N, Nashimoto T, Harada A, Ito Y, et al. Recanalization by mechanical embolus disruption during intra-arterial thrombolysis in the carotid territory. AJNR Am J Neuroradiol. 2004. 25:1391–1402.6. Watanabe M, Mori T, Imai K, Izumoto H, Kamiya T. Intra-arterial fibrinolysis combined with balloon angioplasty in patients with serious symptoms due to acute embolic total occlusion of the carotid artery [abstract]. Stroke. 2004. 35:298.7. Imai K, Mori T, Izumoto H, Watanabe M. Successful thrombectomy in acute terminal internal carotid occlusion using a basket type microsnare in conjunction with temporary proximal occlusion: a case report. AJNR Am J Neuroradiol. 2005. 26:1395–1398.8. Smith WS, Sung G, Saver J, Budzik R, Duckwiler G, Liebeskind DS, et al. Mechanical thrombectomy for acute ischemic stroke: final results of the Multi MERCI trial. Stroke. 2008. 39:1205–1212.9. Flint AC, Duckwiler GR, Budzik RF, Liebeskind DS, Smith WS. MERCI and Multi MERCI Writing Committee. Mechanical thrombectomy of intracranial internal carotid occlusion: pooled results of the MERCI and Multi MERCI Part I trials. Stroke. 2007. 38:1274–1280.
Article10. The Penumbra Pivotal Stroke Trial Investigators. The Penumbra Pivotal Stroke Trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke. 2009. 40:2761–2768.11. Castaño C, Dorado L, Guerrero C, Millán M, Gomis M, Perez de la Ossa N, et al. Mechanical thrombectomy with the Solitaire AB device in large artery occlusions of the anterior circulation: a pilot study. Stroke. 2010. 41:1836–1840.
Article12. Nayak S, Ladurner G, Killer M. Treatment of acute middle cerebral artery occlusion with a Solitaire AB stent: preliminary experience. Br J Radiol. 2010. 83:1017–1022.
Article13. Seifert M, Ahlbrecht A, Dohmen C, Spuentrup E, Moeller-Hartmann W. Combined interventional stroke therapy using intracranial stent and local intraarterial thrombolysis (LIT). Neuroradiology. 2011. 53:273–282.
Article14. Roth C, Papanagiotou P, Behnke S, Walter S, Haass A, Becker C, et al. Stent-assisted mechanical recanalization for treatment of acute intracerebral artery occlusions. Stroke. 2010. 41:2559–2567.
Article15. The National institute of Neurological Disorders and Stroke (NINDS) rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995. 333:1581–1587.16. Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003. 34:e109–e137.
Article17. Keris V, Rudnicka S, Vorona V, Enina G, Tilgale B, Fricbergs J. Combined intraarterial/intravenous thrombolysis for acute ischemic stroke. AJNR Am J Neuroradiol. 2001. 22:352–358.18. Pessin MS, Del Zoppo GJ, Estol CJ. Thrombolytic agents in the treatment of stroke. Clin Neuropharmacol. 1990. 13:271–289.
Article19. Wolpert SM, Bruckmann H, Greenlee R, Wechsler L, Pessin MS, del Zoppo GJ. The rt-PA Acute Stroke Study Group. Neuroradiologic evaluation of patients with acute stroke treated with recombinant tissue plasminogen activator. AJNR Am J Neuroradiol. 1993. 14:3–13.20. Khatri P, Wechsler LR, Broderick JP. Intracranial hemorrhage associated with revascularization therapies. Stroke. 2007. 38:431–440.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adjuvant Tirofiban Injection Through Deployed Solitaire Stent As a Rescue Technique After failed Mechanical Thrombectomy in Acute Stroke
- Primary stent retrieval for acute intracranial large artery occlusion due to atherosclerotic disease
- Intra-Arterial Thrombolysis to Improve Final Thrombolysis in Cerebral Infarction Score after Thrombectomy: A Case-Series Analysis
- Successful Intra-arterial Stent Thrombectomy in Acute Infarction Caused by Spontaneous Middle Cerebral Artery Dissection
- Forced Arterial Suction Thrombectomy of Septic Embolic Middle Cerebral Artery Occlusion Due to Infective Endocarditis: an Illustrative Case and Review of the Literature