Blood Res.
2015 Jun;50(2):97-102. 10.5045/br.2015.50.2.97.
Maximum standardized uptake value on positron emission tomography/computed tomography predicts clinical outcome in patients with relapsed or refractory diffuse large B-cell lymphoma
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University Hospital, Busan, Korea.
- 2Department of Hematology-Oncology, Pusan National University Hospital, Busan, Korea. Hemon@pusan.ac.kr
- 3Department of Hematology-Oncology, Chonnam National University Hwasun Hospital, Hwasun, Korea.
- 4Department of Hematology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 5Department of Hematology, Gachon University Gil Hospital, Incheon, Korea.
- 6Department of Hematology-Oncology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- 7Department of Nuclear Medicine, Pusan National University Hospital, Busan, Korea.
- 8Department of Pathology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- KMID: 2172773
- DOI: http://doi.org/10.5045/br.2015.50.2.97
Abstract
- BACKGROUND
Few clinical studies have clarified the prognostic factors that affect clinical outcomes for patients with relapsed or refractory diffuse large B-cell lymphoma (DLBCL) after immunochemotherapy.
METHODS
A total of 158 patients with relapsed or refractory DLBCL were enrolled. All patients underwent positron emission tomography/computed tomography (PET/CT) before and after salvage therapy. All enrolled patients previously received the ifosfamide, carboplatin, and etoposide regimen. Clinical outcomes were compared according to several factors (age > or = 65 years, low age-adjusted International Prognostic Index [aa-IPI], maximum standardized uptake value [SUVmax] <6.0 on PET/CT, time to relapse > or =12 months, complete response after salvage therapy). A low aa-IPI, SUVmax <6.0, and time to relapse > or = 12 months were independent prognostic factors for survival.
RESULTS
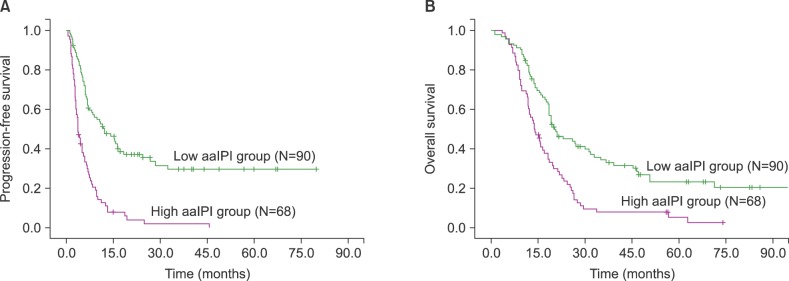
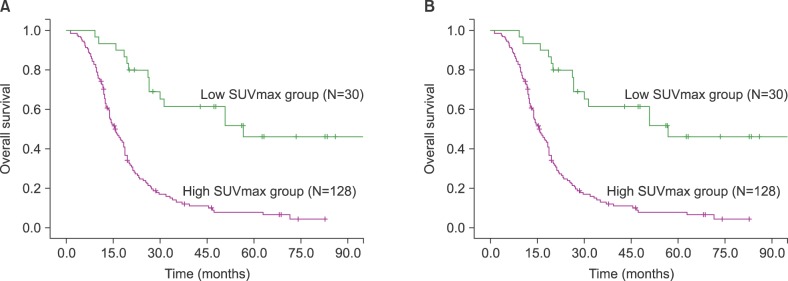
In univariate analysis and multivariate analysis, SUVmax below 6.0 (P<0.001 for progression-free survival (PFS), P<0.001 for overall survival (OS)) and low aa-IPI (P<0.001 for PFS, P<0.001 for OS) were independent prognostic factors associated with favorable outcome.
CONCLUSION
The aa-IPI and initial SUVmax were powerful prognostic factors in patients with relapsed or refractory DLBCL.
Keyword
MeSH Terms
Figure
Reference
-
1. Coiffier B, Thieblemont C, Van Den Neste E, et al. Long-term outcome of patients in the LNH-98.5 trial, the first randomized study comparing rituximab-CHOP to standard CHOP chemotherapy in DLBCL patients: a study by the Groupe d'Etudes des Lymphomes de l'Adulte. Blood. 2010; 116:2040–2045. PMID: 20548096.
Article2. Philip T, Guglielmi C, Hagenbeek A, et al. Autologous bone marrow transplantation as compared with salvage chemotherapy in relapses of chemotherapy-sensitive non-Hodgkin's lymphoma. N Engl J Med. 1995; 333:1540–1545. PMID: 7477169.
Article3. Hamlin PA, Zelenetz AD, Kewalramani T, et al. Age-adjusted International Prognostic Index predicts autologous stem cell transplantation outcome for patients with relapsed or primary refractory diffuse large B-cell lymphoma. Blood. 2003; 102:1989–1996. PMID: 12676776.
Article4. Gisselbrecht C, Glass B, Mounier N, et al. Salvage regimens with autologous transplantation for relapsed large B-cell lymphoma in the rituximab era. J Clin Oncol. 2010; 28:4184–4190. PMID: 20660832.
Article5. Spaepen K, Stroobants S, Dupont P, et al. Prognostic value of pretransplantation positron emission tomography using fluorine 18-fluorodeoxyglucose in patients with aggressive lymphoma treated with high-dose chemotherapy and stem cell transplantation. Blood. 2003; 102:53–59. PMID: 12609836.
Article6. Schot BW, Zijlstra JM, Sluiter WJ, et al. Early FDG-PET assessment in combination with clinical risk scores determines prognosis in recurring lymphoma. Blood. 2007; 109:486–491. PMID: 17003382.
Article7. Dickinson M, Hoyt R, Roberts AW, et al. Improved survival for relapsed diffuse large B cell lymphoma is predicted by a negative pre-transplant FDG-PET scan following salvage chemotherapy. Br J Haematol. 2010; 150:39–45. PMID: 20507301.
Article8. Lim I, Park JY, Kang HJ, et al. Prognostic significance of pretreatment 18F-FDG PET/CT in patients with relapsed/refractory B-cell non-Hodgkin's lymphoma treated by radioimmunotherapy using 131I-rituximab. Acta Haematol. 2013; 130:74–82. PMID: 23548464.9. Lopci E, Santi I, Derenzini E, et al. FDG-PET in the assessment of patients with follicular lymphoma treated by ibritumomab tiuxetan Y 90: multicentric study. Ann Oncol. 2010; 21:1877–1883. PMID: 20147744.
Article10. Cheson BD, Pfistner B, Juweid ME, et al. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007; 25:579–586. PMID: 17242396.11. Vose JM, Anderson JR, Kessinger A, et al. High-dose chemotherapy and autologous hematopoietic stem-cell transplantation for aggressive non-Hodgkin's lymphoma. J Clin Oncol. 1993; 11:1846–1851. PMID: 8105034.
Article12. Prince HM, Imrie K, Crump M, et al. The role of intensive therapy and autologous blood and marrow transplantation for chemotherapy-sensitive relapsed and primary refractory non-Hodgkin's lymphoma: identification of major prognostic groups. Br J Haematol. 1996; 92:880–889. PMID: 8616081.
Article13. Moskowitz CH, Bertino JR, Glassman JR, et al. Ifosfamide, carboplatin, and etoposide: a highly effective cytoreduction and peripheral-blood progenitor-cell mobilization regimen for transplant-eligible patients with non-Hodgkin's lymphoma. J Clin Oncol. 1999; 17:3776–3785. PMID: 10577849.
Article14. de Kreuk M, Ossenkoppele GJ, Meijer CJ, Huijgens PC. Prognostic factors for survival of non-Hodgkin's lymphoma patients treated with high-dose chemotherapy and autologous bone marrow transplantation. Bone Marrow Transplant. 1996; 17:963–971. PMID: 8807101.15. Rapoport AP, Rowe JM, Kouides PA, et al. One hundred autotransplants for relapsed or refractory Hodgkin's disease and lymphoma: value of pretransplant disease status for predicting outcome. J Clin Oncol. 1993; 11:2351–2361. PMID: 8246024.
Article16. Hoskins PJ, Le N, Gascoyne RD, et al. Advanced diffuse large-cell lymphoma treated with 12-week combination chemotherapy: natural history of relapse after initial complete response and prognostic variables defining outcome after relapse. Ann Oncol. 1997; 8:1125–1132. PMID: 9426332.
Article17. Blay J, Gomez F, Sebban C, et al. The International Prognostic Index correlates to survival in patients with aggressive lymphoma in relapse: analysis of the PARMA trial. Parma Group. Blood. 1998; 92:3562–3568. PMID: 9808548.18. Guglielmi C, Martelli M, Federico M, et al. Risk-assessment in diffuse large cell lymphoma at first relapse. A study by the Italian Intergroup for Lymphomas. Haematologica. 2001; 86:941–950. PMID: 11532622.19. Jabbour E, Peslin N, Arnaud P, et al. Prognostic value of the age-adjusted International Prognostic Index in chemosensitive recurrent or refractory non-Hodgkin's lymphomas treated with high-dose BEAM therapy and autologous stem cell transplantation. Leuk Lymphoma. 2005; 46:861–867. PMID: 16019530.
Article20. Berglund M, Thunberg U, Amini RM, et al. Evaluation of immunophenotype in diffuse large B-cell lymphoma and its impact on prognosis. Mod Pathol. 2005; 18:1113–1120. PMID: 15920553.
Article21. Spaepen K, Stroobants S, Dupont P, et al. Prognostic value of positron emission tomography (PET) with fluorine-18 fluorodeoxyglucose ([18F]FDG) after first-line chemotherapy in non-Hodgkin's lymphoma: is [18F]FDG-PET a valid alternative to conventional diagnostic methods? J Clin Oncol. 2001; 19:414–419. PMID: 11208833.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- 18F-2-Deoxy-2-Fluoro-D-Glucose Positron Emission Tomography: Computed Tomography for Preoperative Staging in Gastric Cancer Patients
- Diffuse large B-cell lymphoma presenting with cholecystitis-like symptoms
- Clinically Occult Diffuse Large B-Cell Lymphoma of the Middle Turbinate Identified Using ¹â¸F-Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography: A Case Report
- Primary Diffuse Large B-Cell Lymphoma of the Seminal Vesicle: a Case Report
- Diffuse Large B-Cell Lymphoma in the Era of Precision Oncology: How Imaging Is Helpful