Chonnam Med J.
2012 Aug;48(2):123-127. 10.4068/cmj.2012.48.2.123.
Clinical Effect of a Mixed Solution of Sodium Hyaluronate and Sodium Carboxymethylcellulose During the Transconjunctival Approach for Orbital Wall Reconstruction
- Affiliations
-
- 1Department of Ophthalmology, Research Institute of Medical Sciences, Chonnam National University Medical School and Hospital, Gwangju, Korea. kcyoon@jnu.ac.kr
- KMID: 2172214
- DOI: http://doi.org/10.4068/cmj.2012.48.2.123
Abstract
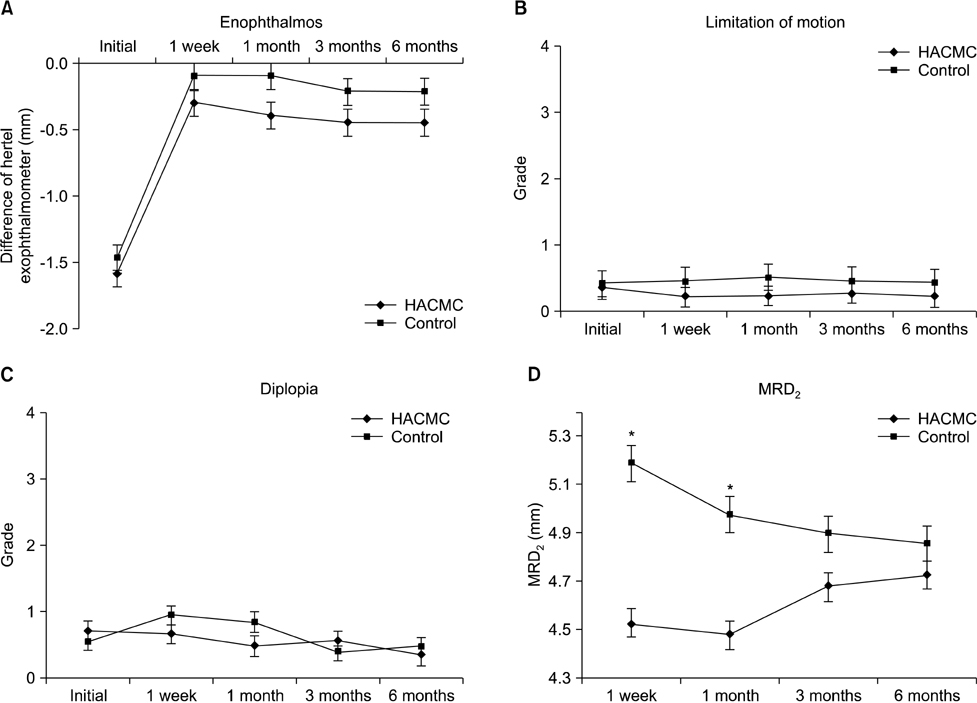
- This study aimed to evaluate the anti-adhesive effect of a mixed solution of sodium hyaluronate and sodium carboxymethylcellulose (HACMC, Guardix-sol(R)) during the transconjunctival approach to orbital wall reconstruction. Eighty-seven patients who underwent orbital wall reconstruction by the transconjunctival approach were enrolled in this prospective study. We applied HACMC between the orbicularis oculi muscle and the orbital septum after surgery in 47 patients and did not use it in 40 patients. Lower lid retraction and marginal reflex distance 2 (MRD2) were measured to analyze the degree of postoperative adhesion at 1 week and 1, 3, and 6 months. The degree of MRD2 showed clinically significant differences at postoperative 1 week and 1 month between the HACMC and control groups (p<0.05). Lower lid ectropion developed in two patients (5.0%) in the control group but did not occur in the HACMC group. In orbital wall reconstruction by the transconjunctival approach, the HACMC mixture solution is effective for preventing adhesion and lower lid ectropion during the early postoperative period.
Keyword
MeSH Terms
Figure
Reference
-
1. Rhee JS, Lynch J, Loehrl TA. Intranasal endoscopy-assisted repair of medial orbital wall fractures. Arch Facial Plast Surg. 2000. 2:269–273.
Article2. Westfall CT, Shore JW, Nunery WR, Hawes MJ, Yaremchuk MJ. Operative complications of the transconjunctival inferior fornix approach. Ophthalmology. 1991. 98:1525–1528.
Article3. Beck DE, Cohen Z, Fleshman JW, Kaufman HS, van Goor H, Wolff BG. Adhesion Study Group Steering Committee. A prospective, randomized, multicenter, controlled study of the safety of Seprafilm adhesion barrier in abdominopelvic surgery of the intestine. Dis Colon Rectum. 2003. 46:1310–1319.
Article4. Kelekci S, Uygur D, Yilmaz B, Sut N, Yesildaglar N. Comparison of human amniotic membrane and hyaluronate/carboxymethylcellulose membrane for prevention of adhesion formation in rats. Arch Gynecol Obstet. 2007. 276:355–359.
Article5. Naito Y, Shin'oka T, Hibino N, Matsumura G, Kurosawa H. A novel method to reduce pericardial adhesion: a combination technique with hyaluronic acid biocompatible membrane. J Thorac Cardiovasc Surg. 2008. 135:850–856.
Article6. Yaacobi Y, Hamed LM, Kaul KS, Fanous MM. Reduction of postoperative adhesions secondary to strabismus surgery in rabbits. Ophthalmic Surg. 1992. 23:123–128.
Article7. Ozkan SB, Kir E, Culhaci N, Dayanir V. The effect of Seprafilm on adhesions in strabismus surgery-an experimental study. J AAPOS. 2004. 8:46–49.
Article8. Kwon SW, Seo YW, Cho YA. Antiadhesive effect of the mixed solution of hyaluronate and sodium carboxymethylcellulose after strabismus surgery. J Korean Ophthalmol Soc. 2009. 50:145–150.
Article9. Park JW, Park HY, Yoon KC. Clinical effect of the mixed solution of sodium hyaluronate and sodium carboxymethylcellulose after endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2010. 51:795–801.
Article10. Taban M, Nakra T, Mancini R, Douglas RS, Goldberg RA. Orbital wall fracture repair using Seprafilm. Ophthal Plast Reconstr Surg. 2009. 25:211–214.
Article11. Bansagi ZC, Meyer DR. Internal orbital fractures in the pediatric age group: characterization and management. Ophthalmology. 2000. 107:829–836.
Article12. Yang HW, Bae JH, Lee HC. The postoperative recovery of ocular motility in pediatric blow-out fracture. J Korean Ophthalmol Soc. 2003. 44:259–264.13. Moon CS, Moon SH, Jang JW. Topographic anatomic difference of the eyelid according to age in Korean. J Korean Ophthalmol Soc. 2003. 44:1865–1871.14. Nowinski D, Messo E, Hedlund A. Treatment of orbital fractures: evaluation of surgical techniques and materials for reconstruction. J Craniofac Surg. 2010. 21:1033–1037.15. Baumann A, Ewers R. Use of the preseptal transconjunctival approach in orbit reconstruction surgery. J Oral Maxillofac Surg. 2001. 59:287–291.
Article16. Mullins JB, Holds JB, Branham GH, Thomas JR. Complications of the transconjunctival approach. A review of 400 cases. Arch Otolaryngol Head Neck Surg. 1997. 123:385–388.17. Novelli G, Ferrari L, Sozzi D, Mazzoleni F, Bozzetti A. Transconjunctival approach in orbital traumatology: a review of 56 cases. J Craniomaxillofac Surg. 2011. 39:266–270.
Article18. Hellebrekers BW, Trimbos-Kemper TC, Trimbos JB, Emeis JJ, Kooistra T. Use of fibrinolytic agents in the prevention of postoperative adhesion formation. Fertil Steril. 2000. 74:203–212.
Article19. Kimmelman CP, Edelstein DR, Cheng HJ. Sepragel sinus (hylan B) as a postsurgical dressing for endoscopic sinus surgery. Otolaryngol Head Neck Surg. 2001. 125:603–608.
Article20. Gago LA, Saed GM, Chauhan S, Elhammady EF, Diamond MP. Seprafilm (modified hyaluronic acid and carboxymethylcellulose) acts as a physical barrier. Fertil Steril. 2003. 80:612–616.
Article21. Oncel M, Remzi FH, Senagore AJ, Connor JT, Fazio VW. Comparison of a novel liquid (Adcon-P) and a sodium hyaluronate and carboxymethylcellulose membrane (Seprafilm) in postsurgical adhesion formation in a murine model. Dis Colon Rectum. 2003. 46:187–191.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antiadhesive Effect of the Mixed Solution of Hyaluronate and Sodium Carboxymethylcellulose After Strabismus Surgery
- Clinical Effect of the Mixed Solution of Sodium Hyaluronate and Sodium Carboxymethylcellulose After Endonasal Dacryocystorhinostomy
- Results of the Mixed Solution of Hyaluronate and Sodium Carboxymethylcellulose in Endonasal Dacryocystorhinostomy
- Repair of Orbital Wall Fracture Using Transcaruncular Approach
- Successful Removal of Apocrinehydrocytoma Using Indocyanine Green and Sodium Hyaluronate