Chonnam Med J.
2015 Apr;51(1):19-25. 10.4068/cmj.2015.51.1.19.
Nine-Month Follow-up Results of Treatment for Nasolacrimal Duct Obstruction by Probing with Adjunctive Mitomycin C in Adults: A Prospective Randomized Placebo-Controlled Trial
- Affiliations
-
- 1Department of Ophthalmology, Jahrom University of Medical Sciences, Jahrom, Iran.
- 2Department of Student Research Committee, Jahrom University of Medical Sciences, Jahrom, Iran.
- 3Zoonoses Research Center, Jahrom University of Medical Sciences, Jahrom, Iran. amin_m505@yahoo.com
- 4Department of Student Research Committee, Shiraz University of Medical Sciences, Shiraz, Iran.
- KMID: 2172143
- DOI: http://doi.org/10.4068/cmj.2015.51.1.19
Abstract
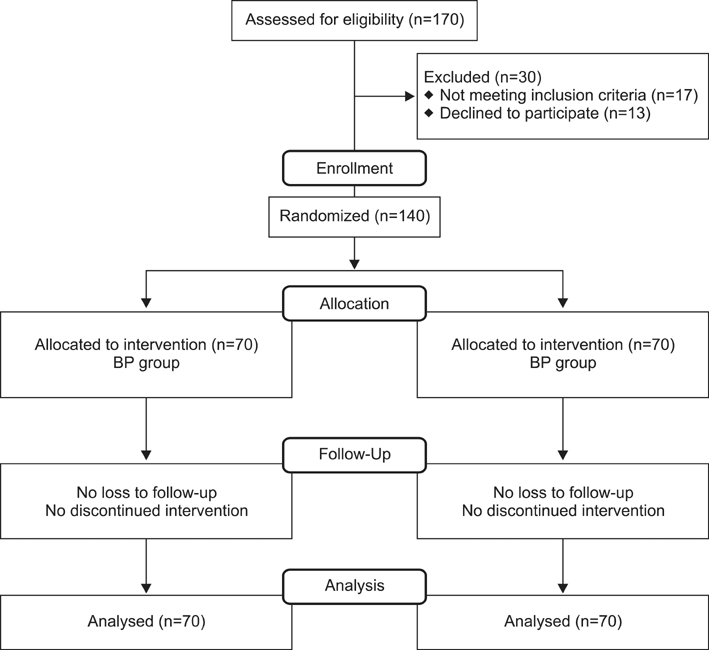
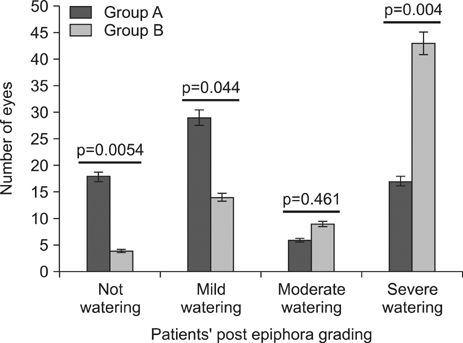
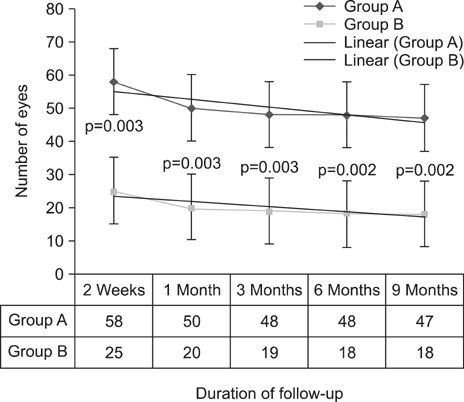
- The current study aimed to determine the efficacy of probing with adjunctive mitomycin C (MMC) as a treatment for nasolacrimal duct obstruction (NLDO) in adults and to study the association of probing success with demographic and obstruction characteristics. This was a prospective, randomized, double-blind, placebo-controlled trial including 140 patients (each with a unilateral NLDO) scheduled for nasolacrimal probing who were randomly assigned to receive MMC (0.2 mg/ml, 70 patients; group A) or placebo (normal saline, 70 patients; group B). Irrigation was carried out with 0.5 cc of MMC (0.2 mg/mL) in the duct with a nasal pack for 10 minutes in group A. Patients' postprobing epiphora was evaluated at 2 weeks and 1, 3, 6, and 9 months postoperatively. Probing was judged to be a success if there was no or mild watering for at least 9 months after the procedure. There were no significant differences between the two study groups in demographic characteristics or duration of the operation (p=0.062). The overall success rate of probing with MMC was 47/70 (67.1%), which was significantly higher than the success rate of the procedure with placebo (p=0.0027). When the sex of the patients was controlled for by logistic regression, a significant association between the failure rate of probing and increasing age was found in cases and controls (p=0.004 vs. p=0.006, respectively). No significant side effects of probing with MMC were noted after 9 months of follow-up. Administering MMC in a dosage of 0.2 mg/mL during nasolacrimal probing significantly increased the success rate of probing. The failure rate of probing increased with age. A low dose of MMC is cheap, safe, and easily accessible; thus, it is recommended during nasolacrimal probing, especially in patients who refuse dacryocystorhinostomy surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Ali MJ. Lacrimal disorders and surgery: historical perspectives. In : Ali MJ, editor. Principles and Practice of Lacrimal Surgery. New Delhi: Springer;2015. p. 1–8.2. Sobel RK, Carter KD, Allen RC. Bilateral lacrimal drainage obstruction and its association with secondary causes. Ophthal Plast Reconstr Surg. 2014; 30:152–156.
Article3. Kamal S, Ali MJ. Primary Acquired Nasolacrimal Duct Obstruction (PANDO) and Secondary Acquired Lacrimal Duct Obstructions (SALDO). In : Ali MJ, editor. Principles and Practice of Lacrimal Surgery. New Delhi: Springer;2015. p. 133–141.4. Nemet AY, Vinker S. Associated morbidity of nasolacrimal duct obstruction--a large community based case-control study. Graefes Arch Clin Exp Ophthalmol. 2014; 252:125–130.
Article5. Baig R, Khan QA, Ahmad K. Long-term outcome of primary external dacryocystorhinostomy. J Coll Physicians Surg Pak. 2013; 23:641–644.6. Ekinci M, Çağatay HH, Oba ME, Yazar Z, Kaplan A, Gökçe G, et al. The long-term follow-up results of external dacryocystorhinostomy skin incision scar with W incision. Orbit. 2013; 32:349–355.
Article7. Kaufman SC, Jacobs DS, Lee WB, Deng SX, Rosenblatt MI, Shtein RM. Options and adjuvants in surgery for pterygium: a report by the American Academy of Ophthalmology. Ophthalmology. 2013; 120:201–208.8. Kashkouli MB, Heirati A, Pakdel F, Kiavash V, Naseripour M, Aghamohammadi F. Long-term follow-up of invasive ocular surface squamous cell carcinoma treated with excision, cryotherapy, and topical mitomycin C. Graefes Arch Clin Exp Ophthalmol. 2012; [Epub ahead of print].
Article9. Birkholz ES, Goins KM, Sutphin JE, Kitzmann AS, Wagoner MD. Treatment of ocular surface squamous cell intraepithelial neoplasia with and without mitomycin C. Cornea. 2011; 30:37–41.
Article10. Lichtinger A, Pe'er J, Frucht-Pery J, Solomon A. Limbal stem cell deficiency after topical mitomycin C therapy for primary acquired melanosis with atypia. Ophthalmology. 2010; 117:431–437.
Article11. Lim LA, Madigan MC, Conway RM. Conjunctival melanoma: a review of conceptual and treatment advances. Clin Ophthalmol. 2013; 6:521–531.
Article12. Tsai CC, Kau HC, Kao SC, Hsu WM, Liu JH. Efficacy of probing the nasolacrimal duct with adjunctive Mitomycin-C for epiphora in adults. Ophthalmology. 2002; 109:172–174.
Article13. Sinha MK, Bajaj MS, Pushker N, Ghose S, Chandra M. Efficacy of probing with mitomycin-C in adults with primary acquired nasolacrimal duct obstruction. J Ocul Pharmacol Ther. 2013; 29:353–355.
Article14. Ghobadifar MA, Degani N, Dezhkam I, Rezaei N. Probing with mitomycin-C in adults with nasolacrimal duct obstruction. J Ocul Pharmacol Ther. 2013; 29:515.
Article15. Choontanom R. Probing and syringing with 3% solution of NaCl and/or 0.2 mg/ml mitomycin-C in nasolacrimal duct obstruction patients. J Med Assoc Thai. 2010; 93:Suppl 6. S197–S202.16. Razeghinezhad MR, Banihashemi SA, Bagheri B. Probing with adjunctive Mitomycin-C In adult patients with nasolacrimal duct obstruction. Med J Hormozgan Univ. 2005; 9:219–220.17. Tabatabaii SZAD, Sadeghi TA, Kasaei AAF. Efficacy of nasolacrimal duct probing with adjuctive Mitomycin C for adult partial nasolacrimal duct obstruction (Pnldo). Iran J Ophthalmol. 2005; 18:6–10.18. Rubinfeld RS, Pfister RR, Stein RM, Foster CS, Martin NF, Stoleru S, et al. Serious complications of topical mitomycin-C after pterygium surgery. Ophthalmology. 1992; 99:1647–1654.
Article19. Kashkouli MB, Beigi B, Parvaresh MM, Kassaee A, Tabatabaee Z. Late and very late initial probing for congenital nasolacrimal duct obstruction: what is the cause of failure? Br J Ophthalmol. 2003; 87:1151–1153.
Article20. Stager D, Baker JD, Frey T, Weakley DR Jr, Birch EE. Office probing of congenital nasolacrimal duct obstruction. Ophthalmic Surg. 1992; 23:482–484.
Article21. Linberg JV, McCormick SA. Primary acquired nasolacrimal duct obstruction. A clinicopathologic report and biopsy technique. Ophthalmology. 1986; 93:1055–1063.22. DeAngelis D, Hurwitz J, Oestreicher J, Howarth D. The pathogenesis and treatment of lacrimal obstruction: The value of lacrimal sac and bone analysis. Orbit. 2001; 20:163–172.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Silicone Nasolacrimal Intubation with Mitomycin C Treatmentfor Treatment of Incomplete Nasolacrimal Duct Obstruction
- The Clinical outcome of Probing and Silicone Tube Intubation for Congenital Nasolacrimal Duct Obstruction
- The Effect of Mitomycin C Instillation after Silicone Intubation in Adult Partial Nasolacrimal Duct Obstruction
- The Effect of Probing for Congenital Nasolacrimal Duct Obstruction
- Silicone Intubation and Postoperative Mitomycin Application for Partial Nasolacrimal Duct Obstruction in Adults