Ann Dermatol.
2011 Aug;23(3):396-399. 10.5021/ad.2011.23.3.396.
A Sporadic Case of Mal de Meleda Caused by Gene Mutation in SLURP-1 in Korea
- Affiliations
-
- 1Department of Dermatology, Hanyang University College of Medicine, Seoul, Korea. drko0303@hanyang.ac.kr
- KMID: 2171939
- DOI: http://doi.org/10.5021/ad.2011.23.3.396
Abstract
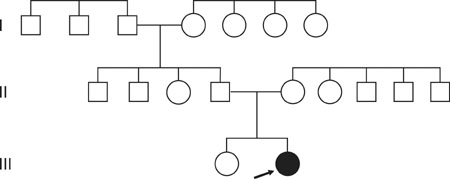
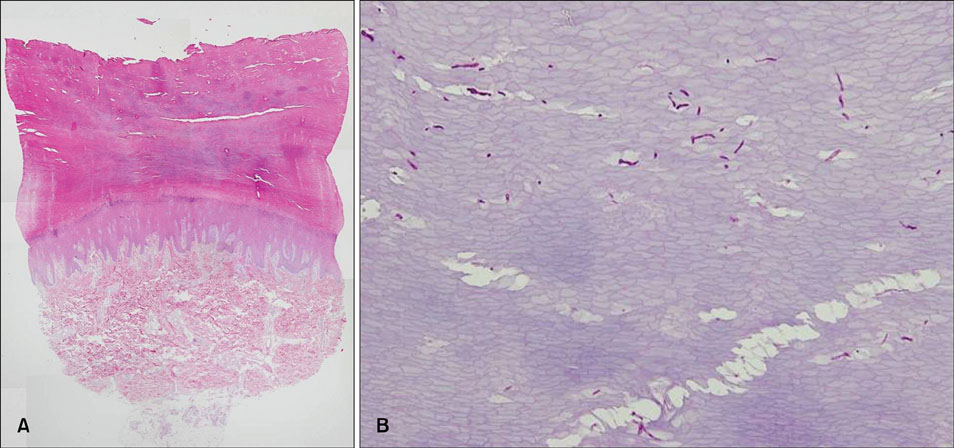
- Mal de Meleda (MDM), also known as keratoderma palmoplantaris transgrediens, is a rare inherited form of palmoplantar keratoderma. It is characterized by erythema and hyperkeratosis of the palms and soles, extending to the dorsal aspects of the hands and feet. A 15-year-old Korean female presented with sharply demarcated hyperkeratotic plaques on the palms and soles, which extended to the dorsal surfaces of the hands and feet, in a "glove-and-socks" distribution. The histopathologic study showed marked hyperkeratosis, acanthosis, and normogranulosis, without epidermolysis. Her genetic study detected compound heterozygous mutation in exon 3 of the ARS gene encoding SLURP-1. Family history did not reveal any other affected members and no consanguineous relationship was found. In view of these findings, we diagnosed this case as the first reported sporadic case of MDM in Korea, the farthest location from the endemic island of Meleda.
MeSH Terms
Figure
Reference
-
1. Wajid M, Kurban M, Shimomura Y, Christiano AM. Mutations in the SLURP-1 gene underlie Mal de Meleda in three Pakistani families. J Dermatol Sci. 2009. 56:27–32.
Article2. Chao SC, Lai FJ, Yang MH, Lee JY. Mal de Meleda in a taiwanese. J Formos Med Assoc. 2005. 104:276–278.3. Ergin S, Erdogan BS, Aktan S. Mal de Meleda: a new geographical localization in Anatolia. Dermatology. 2003. 206:124–130.
Article4. Kelsell DP, Stevens HP. The palmoplantar keratodermas: much more than palms and soles. Mol Med Today. 1999. 5:107–113.
Article5. Saftić V, Rudan D, Zgaga L. Mendelian diseases and conditions in Croatian island populations: historic records and new insights. Croat Med J. 2006. 47:543–552.6. Fischer J, Bouadjar B, Heilig R, Huber M, Lefèvre C, Jobard F, et al. Mutations in the gene encoding SLURP-1 in Mal de Meleda. Hum Mol Genet. 2001. 10:875–880.
Article7. Chimienti F, Hogg RC, Plantard L, Lehmann C, Brakch N, Fischer J, et al. Identification of SLURP-1 as an epidermal neuromodulator explains the clinical phenotype of Mal de Meleda. Hum Mol Genet. 2003. 12:3017–3024.
Article8. Katugampola RP, Finlay AY. Oral retinoid therapy for disorders of keratinization: single-centre retrospective 25 years' experience on 23 patients. Br J Dermatol. 2006. 154:267–276.
Article9. Braun-Falco M. Hereditary palmoplantar keratodermas. J Dtsch Dermatol Ges. 2009. 7:971–984.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Familial hyperkalemic periodic paralysis caused by a de novo mutation in the sodium channel gene SCN4A
- Somatic Mutational Analysis of MEN1 and Phenotypic Correlation in Sporadic Parathyroid Tumors
- Mal de Debarquement Syndrome with Apogeotropic Positional Nystagmus
- De novo a novel variant of CaSR gene in a neonate with congenital hypoparathyroidism
- APC Mutation Spectra in Sporadic Colon Cancer Tissue among Korean