Ann Dermatol.
2011 Aug;23(3):369-374. 10.5021/ad.2011.23.3.369.
Chromoblastomycosis Caused by Fonsecaea pedrosoi
- Affiliations
-
- 1Department of Dermatology, College of Medicine, Dongguk University, Gyeongju, Korea. smg@dongguk.ac.kr
- 2Department of Laboratory Medicine, College of Medicine, Dongguk University, Gyeongju, Korea.
- 3Department of Dermatology, College of Medicine, Inha University, Incheon, Korea.
- KMID: 2171932
- DOI: http://doi.org/10.5021/ad.2011.23.3.369
Abstract
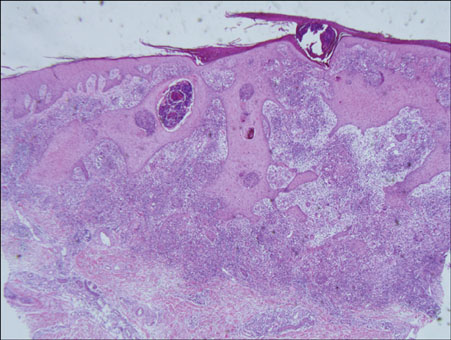
- We report herein a case of chromoblastomycosis caused by Fonsecaea (F.) pedrosoi in a 39-year-old male, who showed multiple, asymptomatic, scaly erythematous plaques on the left shin for 12 months. Histopathologically, chronic granulomatous inflammation and either sclerotic or muriform cells were observed. The fungal culture produced typical black colonies of F. pedrosoi. The DNA sequence of the internal transcribed spacer (ITS) region of the clinical sample was 100% match to that of F. pedrosoi IFM 47061 (GenBank accession number AB240943). The patient was treated with 200 mg of itraconazole daily, for 3 months. Skin lesions were improved. In Korea, only 9 cases of chromoblastomycosis, including this case, have been reported until now. The etiologic agent was F. pedrosoi in the majority of cases (6/9;67%). The incidence of chromoblastomycosis was slightly higher in female, and the upper limbs were more affected than the lower limbs in patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Queiroz-Telles F, Esterre P, Perez-Blanco M, Vitale RG, Salgado CG, Bonifaz A. Chromoblastomycosis: an overview of clinical manifestations, diagnosis and treatment. Med Mycol. 2009. 47:3–15.
Article2. Kwon-Chung KJ, Bennett JE. Medical mycology. 1992. Philadelphia: Lea & Febiger;337–355.3. López Martínez R, Méndez Tovar LJ. Chromoblastomycosis. Clin Dermatol. 2007. 25:188–194.
Article4. Suh MK, Lee YH. Infectious caused by dematiaceous fungi. Korean J Med Mycol. 2005. 10:77–82.5. Santos AL, Palmeira VF, Rozental S, Kneipp LF, Nimrichter L, Alviano DS, et al. Biology and pathogenesis of Fonsecaea pedrosoi, the major etiologic agent of chromoblastomycosis. FEMS Microbiol Rev. 2007. 31:570–591.
Article6. Kondo M, Hiruma M, Nishioka Y, Mayuzumi N, Mochida K, Ikeda S, et al. A case of chromomycosis caused by Fonsecaea pedrosoi and a review of reported cases of dematiaceous fungal infection in Japan. Mycoses. 2005. 48:221–225.
Article7. Yaguchi T, Tanaka R, Nishimura K, Udagawa S. Molecular phylogenetics of strains morphologically identified as Fonsecaea pedrosoi from clinical specimens. Mycoses. 2007. 50:255–260.
Article8. Ahn SK, Lee SN. A case of chromonycosis. Korean J Dermatol. 1990. 28:345–348.9. Suh MK, Sung YO, Yoon KS, Ha GY, Kim JR. A case of chromoblastomycosis caused by Fonsecaea pedrosoi. Korean J Dermatol. 1996. 34:832–836.10. Kim HU, Son GY, Ihm CW. A case of chromoblastomycosis showing a good response to itraconazole. Ann Dermatol. 1997. 9:51–54.
Article11. Kim SW, Oh SH, Choi SK, Lee YH, Yoon JH, Bang YJ, et al. Chromoblastomycosis treated with occlusive dressing of amphotericin B cream. Korean J Med Mycol. 2000. 5:144–149.12. Kang NG, Suh MK, Park SG, Song KY, Kim TH. A case of chromomycosis showing ulcerative lesions on dorsa of hands. Korean J Dermatol. 2002. 40:174–177.13. Lee CW, Sim SJ, Song KH, Kim KH. A case of chromoblastomycosis treated with terbinafine. Korean J Med Mycol. 2003. 8:26–29.14. Jun JB, Park JY, Kim DW, Suh SB. Chromoblastomycosis caused by Rhinocladiella aquaspersa. Korean J Med Mycol. 2004. 9:117–122.15. Park SG, Oh SH, Suh SB, Lee KH, Chung KY. A case of chromoblastomycosis with an unusual clinical manifestation caused by Phialophora verrucosa on an unexposed area: treatment with a combination of amphotericin B and 5-flucytosine. Br J Dermatol. 2005. 152:560–564.
Article16. De Hoog GS, Queiroz-Telles F, Haase G, Fernandez-Zeppenfeldt G, Attili Angelis D, Gerrits Van Den Ende AH, et al. Black fungi: clinical and pathogenic approaches. Med Mycol. 2000. 38:Suppl 1. 243–250.
Article17. Minotto R, Bernardi CD, Mallmann LF, Edelweiss MI, Scroferneker ML. Chromoblastomycosis: a review of 100 cases in the state of Rio Grande do Sul, Brazil. J Am Acad Dermatol. 2001. 44:585–592.
Article18. Silva JP, de Souza W, Rozental S. Chromoblastomycosis: a retrospective study of 325 cases on Amazonic region (Brazil). Mycopathologia. 1998-1999. 143:171–175.19. Hinshaw M, Longley BJ. Elder DE, Elenitsas R, Johnson BL, Murphy GF, editors. Fungal diseases. Lever's histopathology of the skin. 2005. 9th ed. Philadelphia: Lippincott Williams & Wilkins;619–620.20. De Hoog GS, Attili-Angelis D, Vicente VA, Van Den Ende AH, Queiroz-Telles F. Molecular ecology and pathogenic potential of Fonsecaea species. Med Mycol. 2004. 42:405–416.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Chromoblastomycosis Caused by Fonsecaea pedrosoi
- A Case of Chromoblastomycosis Showing a Good Response to Itraconazole
- Chromoblastomycosis Treated with Occlusive Dressing of Amphotericin B Cream
- Chromoblastomycosis Caused by Fonsecaea monophora
- A Case of Chromoblastomycosis Treated with Terbinafine