Ewha Med J.
2013 Sep;36(2):139-143. 10.12771/emj.2013.36.2.139.
Minimal Change Disease in Systemic Lupus: Another Renal Manifestation of Lupus?
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. hansh@yuhs.ac
- 2Department of Pathology, Yonsei University College of Medicine, Seoul, Korea.
- 3Brain Korea 21 for Medical Science, Severance Biomedical Science Institute, Yonsei University, Seoul, Korea.
- KMID: 2171249
- DOI: http://doi.org/10.12771/emj.2013.36.2.139
Abstract
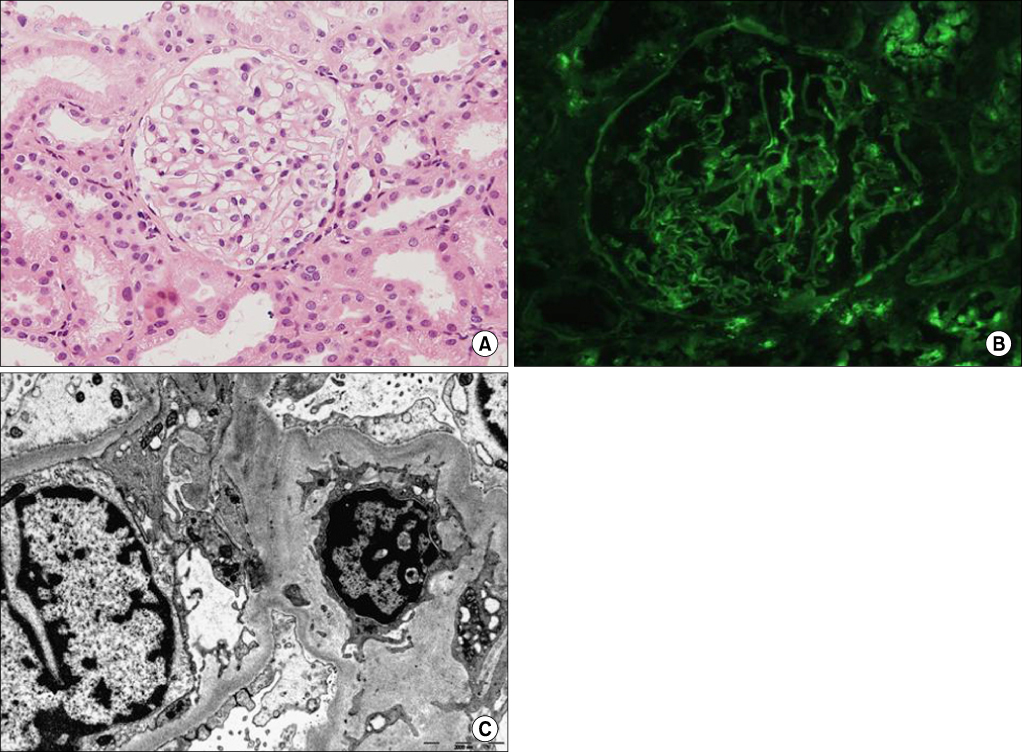
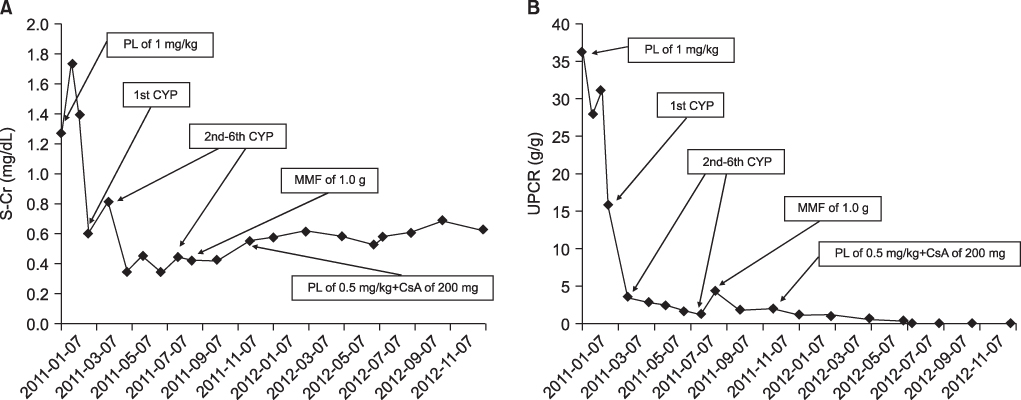
- Nephrotic syndrome is most commonly observed in membranous lupus nephritis in patients with systemic lupus erythematosus (SLE). However, other forms of idiopathic nephrotic syndrome rarely occur in these patients. Here, we report a case of SLE complicated by minimal change disease (MCD). A 24-year-old woman with SLE visited our hospital for generalized edema and heavy proteinuria. Laboratory tests did not support immunological exacerbation of lupus, while renal biopsy revealed diffusely effaced foot processes without electron-dense deposits that were consistent with MCD. Administration of high-dose corticosteroids and 6 subsequent cycles of monthly intravenous cyclophosphamide resulted in complete remission. Although nephrotic-range proteinuria recurred 1 month after switching to maintenance therapy with mycophenolate mofetil, complete remission was reestablished after a 6-month treatment with corticosteroids and cyclosporine. Physicians should be cautious in assessment and management of such a rare renal manifestation.
MeSH Terms
Figure
Reference
-
1. Cameron JS. Systemic lupus erythematosus. In : Neilson EG, Couser WG, editors. Immunologic renal diseases. 2nd ed. Philadelphia: Lippincott Williams & Wilkins;2001. p. 1057–1104.2. Shahane A, Khasnis A, Gota C. Rituximab-responsive nephrotic syndrome due to minimal change disease in systemic lupus erythematosus. J Clin Rheumatol. 2012; 18:199–202.3. Lupus nephritis: prognostic factors and probability of maintaining life-supporting renal function 10 years after the diagnosis: Gruppo Italiano per lo Studio della Nefrite Lupica (GISNEL). Am J Kidney Dis. 1992; 19:473–479.4. Perakis C, Arvanitis A, Sotsiou F, Emmanouel DS. Nephrotic syndrome caused by minimal-change disease in a patient with focal proliferative SLE nephritis (WHO III) in remission. Nephrol Dial Transplant. 1998; 13:467–470.5. Hertig A, Droz D, Lesavre P, Grunfeld JP, Rieu P. SLE and idiopathic nephrotic syndrome: coincidence or not? Am J Kidney Dis. 2002; 40:1179–1184.6. Seo DB, Lee SW, Song JH, Lee KJ, Han JY, Kim MJ. Acute renal failure associated with a minimal change nephrotic syndrome in a systemic lupus erythematosus patient. Yonsei Med J. 2002; 43:114–118.7. Horino T, Takao T, Morita T, Ito H, Hashimoto K. Minimal change nephrotic syndrome associated with systemic lupus erythematosus. Nephrol Dial Transplant. 2006; 21:230.8. Hong YH, Yun DY, Jung YW, Oh MJ, Kim HJ, Lee CK. A case of minimal change disease treated successfully with mycophenolate mofetil in a patient with systemic lupus erythematosus. Korean J Intern Med. 2011; 26:470–473.9. Redondo-Pachon MD, Enriquez R, Sirvent AE, Andrada E, Millan I, Amoros F. Minimal-change nephropathy in systemic lupus erythematosus. Nefrologia. 2012; 32:412–413.10. Zhou HQ, Zhang FC, Tian XP, Leng XM, Lu JJ, Zhao Y, et al. Clinical features and outcome of neuropsychiatric lupus in Chinese: analysis of 240 hospitalized patients. Lupus. 2008; 17:93–99.11. Smolen JS, Chused TM, Leiserson WM, Reeves JP, Alling D, Steinberg AD. Heterogeneity of immunoregulatory T-cell subsets in systemic lupus erythematosus. Correlation with clinical features. Am J Med. 1982; 72:783–790.12. Morimoto C, Steinberg AD, Letvin NL, Hagan M, Takeuchi T, Daley J, et al. A defect of immunoregulatory T cell subsets in systemic lupus erythematosus patients demonstrated with anti-2H4 antibody. J Clin Invest. 1987; 79:762–768.13. Okamoto A, Fujio K, Okamura T, Yamamoto K. Regulatory T-cell-associated cytokines in systemic lupus erythematosus. J Biomed Biotechnol. 2011; 2011:463412.14. Koyama A, Fujisaki M, Kobayashi M, Igarashi M, Narita M. A glomerular permeability factor produced by human T cell hybridomas. Kidney Int. 1991; 40:453–460.15. Ozaki T. Two-color analysis of lymphocyte subpopulations in membranous nephropathy and minimal change nephrotic syndrome. Nihon Jinzo Gakkai Shi. 1989; 31:797–806.16. Fiser RT, Arnold WC, Charlton RK, Steele RW, Childress SH, Shirkey B. T-lymphocyte subsets in nephrotic syndrome. Kidney Int. 1991; 40:913–916.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Transverse Myelitis as a First Manifestation of Systemic Lupus Erythematosus
- Pulmonary Hemorrhage with Hemoptysis in Systemic Lupus Erythematosis
- Acute Renal Failure Associated with a Minimal Change Nephrotic Syndrome in a Systemic Lupus Erythematosus Patient
- A case of Lupus Nephritis
- A Case of Systemic Lupus Erythematosus Involving the Kidneys in a Patient with IgA Nephropathy