Change of Bone Mineral Density and Biochemical Markers of Bone Turnover in Patients on Suppressive Levothyroxine Therapy for Differentiated Thyroid Carcinoma
- Affiliations
-
- 1Department of Endocrinology, Inha University School of Medicine, Incheon, Korea. sbhongmd@inha.ac.kr
- 2Department of Internal Medicine, Hallym General Hospital, Incheon, Korea.
- KMID: 2170110
- DOI: http://doi.org/10.11005/jbm.2015.22.3.135
Abstract
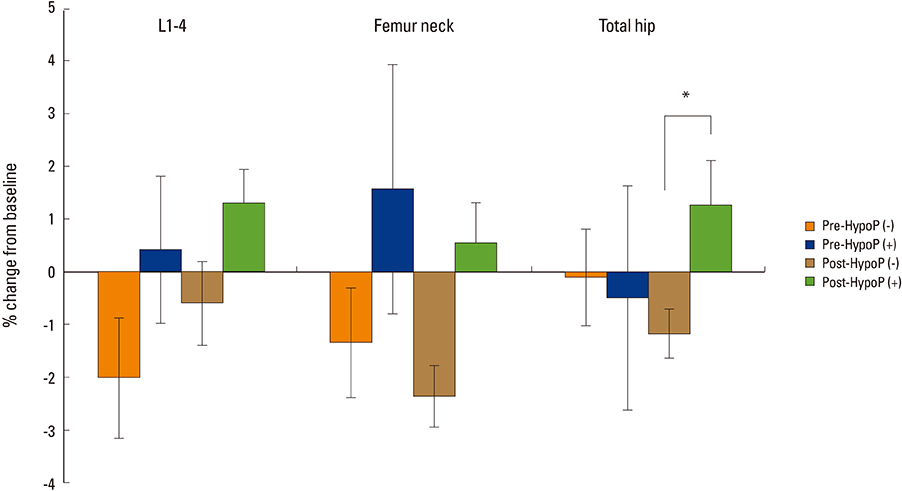
- Untreated hyperthyroidism and high-dose thyroid hormone are associated with osteoporosis, and increased bone mineral density (BMD) has been demonstrated in postmenopausal females with hypoparathyroidism. Studies on the effect of suppressive levothyroxine (LT4) therapy on BMD and bone metabolism after total thyroidectomy in patients with differentiated thyroid carcinoma have presented conflicting results, and few studies in relation to the status of hypoparathyroidism have been studied. One hundred postmenopausal women and 24 premenopausal women on LT4 suppression therapy were included in this study. BMD of lumbar spine and femur and bone turnover markers were measured at the baseline and during the follow-up period up to 18 months using dual energy X-ray absorptiometry. Biochemical marker of bone resorption was measured by urine deoxypyridinoline and bone formation by serum osteocalcin. The age ranged from 36 to 64 years old. Thyroid stimulating hormone (TSH) was suppressed during the study. The results showed that BMD of femur and lumbar spine were not significantly changed in both pre- and postmenopausal women except femur neck in postmenopausal women without hypoparathyroidism. Patients with hypoparathyroidism had higher BMD gain than those without hypoparathyroidism in total hip (1.25 vs. -1.18%, P=0.015). Biochemical markers of bone turnover, serum osteocalcin, and urine deoxypyridinoline did not show significant change. In conclusion, patients with well differentiated thyroid carcinoma are not at a great risk of bone loss after LT4 suppressive therapy. The state of hypoparathyroidism is associated with increased BMD, particularly in postmenopausal women.
MeSH Terms
-
Absorptiometry, Photon
Biomarkers*
Bone Density*
Bone Resorption
Female
Femur
Femur Neck
Follow-Up Studies
Hip
Humans
Hyperthyroidism
Hypoparathyroidism
Metabolism
Osteocalcin
Osteogenesis
Osteoporosis
Postmenopause
Spine
Thyroid Gland*
Thyroid Neoplasms*
Thyroidectomy
Thyrotropin
Thyroxine*
Osteocalcin
Thyrotropin
Thyroxine
Figure
Cited by 6 articles
-
Association between Hemoglobin Level and Bone Mineral Density in Korean Adults
Yun Hwan Oh, Ji Hyun Moon, Belong Cho
J Bone Metab. 2017;24(3):161-173. doi: 10.11005/jbm.2017.24.3.161.Effects of Thyrotropin Suppression on Bone Health in Menopausal Women with Total Thyroidectomy
Eun Heui Kim, Yun Kyung Jeon, Kyoungjune Pak, In-Joo Kim, Seong-Jang Kim, Seunghyeon Shin, Bo Hyun Kim, Sang Soo Kim, Byung-Joo Lee, Jeong-Gyu Lee, Tae Sik Goh, Keunyoung Kim
J Bone Metab. 2019;26(1):31-38. doi: 10.11005/jbm.2019.26.1.31.Risk of Osteoporotic Fractures after Thyroid-stimulating Hormone Suppression Therapy in Patients with Thyroid Cancer
Youjin Lee, Byung-Ho Yoon, Seeyoun Lee, Youn Kyung Chung, Young-Kyun Lee
J Bone Metab. 2019;26(1):45-50. doi: 10.11005/jbm.2019.26.1.45.Influence of Thyroid-stimulating Hormone Suppression Therapy on Bone Mineral Density in Patients with Differentiated Thyroid Cancer: A Meta-analysis
Byung-Ho Yoon, Youjin Lee, Hyun Jin Oh, Sung Han Kim, Young-Kyun Lee
J Bone Metab. 2019;26(1):51-60. doi: 10.11005/jbm.2019.26.1.51.TSH Suppression after Differentiated Thyroid Cancer Surgery and Osteoporosis
Kyoung Sik Park
Korean J Endocr Surg. 2016;16(1):1-5. doi: 10.16956/kjes.2016.16.1.1.Bone Mineral Density in Thyroid Cancer Patients: Data from the Korea National Health and Nutrition Examination Survey
Myung-Chul Chang
J Endocr Surg. 2017;17(4):153-159. doi: 10.16956/jes.2017.17.4.153.
Reference
-
1. Brito JP, Davies L. Is there really an increased incidence of thyroid cancer? Curr Opin Endocrinol Diabetes Obes. 2014; 21:405–408.
Article2. Cooper DS, Doherty GM, Haugen BR, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19:1167–1214.
Article3. Mosekilde L, Eriksen EF, Charles P. Effects of thyroid hormones on bone and mineral metabolism. Endocrinol Metab Clin North Am. 1990; 19:35–63.
Article4. Lee MY, Park JH, Bae KS, et al. Bone mineral density and bone turnover markers in patients on long-term suppressive levothyroxine therapy for differentiated thyroid cancer. Ann Surg Treat Res. 2014; 86:55–60.
Article5. Heijckmann AC, Huijberts MS, Geusens P, et al. Hip bone mineral density, bone turnover and risk of fracture in patients on long-term suppressive L-thyroxine therapy for differentiated thyroid carcinoma. Eur J Endocrinol. 2005; 153:23–29.
Article6. Larijani B, Gharibdoost F, Pajouhi M, et al. Effects of levothyroxine suppressive therapy on bone mineral density in premenopausal women. J Clin Pharm Ther. 2004; 29:1–5.
Article7. Reverter JL, Holgado S, Alonso N, et al. Lack of deleterious effect on bone mineral density of long-term thyroxine suppressive therapy for differentiated thyroid carcinoma. Endocr Relat Cancer. 2005; 12:973–981.
Article8. Marcocci C, Golia F, Bruno-Bossio G, et al. Carefully monitored levothyroxine suppressive therapy is not associated with bone loss in premenopausal women. J Clin Endocrinol Metab. 1994; 78:818–823.
Article9. Jódar E, Begoña López M, Garcia L, et al. Bone changes in pre- and postmenopausal women with thyroid cancer on levothyroxine therapy: evolution of axial and appendicular bone mass. Osteoporos Int. 1998; 8:311–316.
Article10. Kung AW, Yeung SS. Prevention of bone loss induced by thyroxine suppressive therapy in postmenopausal women: the effect of calcium and calcitonin. J Clin Endocrinol Metab. 1996; 81:1232–1236.
Article11. Kim MK, Yun KJ, Kim MH, et al. The effects of thyrotropin-suppressing therapy on bone metabolism in patients with well-differentiated thyroid carcinoma. Bone. 2015; 71:101–105.
Article12. Mohammadi B, Haghpanah V, Tavangar SM, et al. Modeling the effect of levothyroxine therapy on bone mass density in postmenopausal women: a different approach leads to new inference. Theor Biol Med Model. 2007; 4:23.
Article13. Mazokopakis EE, Starakis IK, Papadomanolaki MG, et al. Changes of bone mineral density in pre-menopausal women with differentiated thyroid cancer receiving L-thyroxine suppressive therapy. Curr Med Res Opin. 2006; 22:1369–1373.
Article14. Youngwirth L, Benavidez J, Sippel R, et al. Parathyroid hormone deficiency after total thyroidectomy: incidence and time. J Surg Res. 2010; 163:69–71.
Article15. Cooper DS, Specker B, Ho M, et al. Thyrotropin suppression and disease progression in patients with differentiated thyroid cancer: results from the National Thyroid Cancer Treatment Cooperative Registry. Thyroid. 1998; 8:737–744.
Article16. Lee MS, Kim SY, Lee MC, et al. Negative correlation between the change in bone mineral density and serum osteocalcin in patients with hyperthyroidism. J Clin Endocrinol Metab. 1990; 70:766–770.
Article17. De Sanctis V, Soliman A, Fiscina B. Hypoparathyroidism: from diagnosis to treatment. Curr Opin Endocrinol Diabetes Obes. 2012; 19:435–442.18. Chan FK, Tiu SC, Choi KL, et al. Increased bone mineral density in patients with chronic hypoparathyroidism. J Clin Endocrinol Metab. 2003; 88:3155–3159.
Article19. Duan Y, De Luca V, Seeman E. Parathyroid hormone deficiency and excess: similar effects on trabecular bone but differing effects on cortical bone. J Clin Endocrinol Metab. 1999; 84:718–722.
Article20. Dawson-Hughes B, Dallal GE, Krall EA, et al. A controlled trial of the effect of calcium supplementation on bone density in postmenopausal women. N Engl J Med. 1990; 323:878–883.
Article21. Reid IR, Ames RW, Evans MC, et al. Effect of calcium supplementation on bone loss in postmenopausal women. N Engl J Med. 1993; 328:460–464.
Article22. Chapuy MC, Arlot ME, Duboeuf F, et al. Vitamin D3 and calcium to prevent hip fractures in the elderly women. N Engl J Med. 1992; 327:1637–1642.
Article23. Haussler MR, Haussler CA, Jurutka PW, et al. The vitamin D hormone and its nuclear receptor: molecular actions and disease states. J Endocrinol. 1997; 154:Suppl. S57–S73.24. Cranney A, Weiler HA, O'Donnell S, et al. Summary of evidence-based review on vitamin D efficacy and safety in relation to bone health. Am J Clin Nutr. 2008; 88:513s–519s.
Article25. Uzzan B, Campos J, Cucherat M, et al. Effects on bone mass of long term treatment with thyroid hormones: a meta-analysis. J Clin Endocrinol Metab. 1996; 81:4278–4289.
Article26. Hawkins F, Escobar-Jiménez F, Jódar E, et al. Bone mineral density in hypoparathyroid women on LT4 suppressive therapy. Effect of calcium and 1,25(OH)2 vitamin D3 treatment. J Musculoskelet Neuronal Interact. 2003; 3:71–76.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bone mineral density and bone turnover markers in patients on long-term suppressive levothyroxine therapy for differentiated thyroid cancer
- The Bone Mineral Density and Bone Metabolism of Patients with Differentiated Thyroid Carcinoma and who are Receiving Long-term TSH Suppressive Therapy
- Changes of Biochemical Markers of Bone turnover in Pre-, Peri-and Postmenopausal Women
- Evaluation and Management of Bone Health in Patients with Thyroid Diseases: A Position Statement of the Korean Thyroid Association
- Bone Mineral Density in Postsurgical Thyroxine Replacement